When hot flashes hit 15 times a day and sleep vanishes for weeks, it’s not just discomfort-it’s life shutting down. For millions of women, menopause isn’t a phase you gently walk through. It’s a sudden shift that leaves you drained, confused, and wondering if there’s any relief. Hormone therapy, or HRT, has been the go-to answer for decades. But after decades of fear, confusion, and conflicting headlines, the real question isn’t whether it works-it’s who it works for, and when it’s safe.
What Hormone Therapy Actually Does
Menopause hormone therapy (MHT), often called hormone replacement therapy (HRT), replaces the estrogen your body stops making after your ovaries slow down. For some women, that drop triggers night sweats, brain fog, vaginal dryness, and mood swings that wreck daily life. HRT doesn’t cure menopause. It doesn’t reverse aging. But it does stop those symptoms in their tracks-for most women, within days or weeks. Estrogen alone works for women who’ve had a hysterectomy. For those still with a uterus, you need progestogen too. Why? Because estrogen alone can cause the lining of the uterus to thicken, raising the risk of endometrial cancer. Adding progestogen keeps that lining thin and safe. The most effective forms? Low-dose transdermal patches or gels. They deliver estrogen straight through the skin, bypassing the liver. That means less strain on your blood clotting system. Oral pills? They go through the liver first, which can increase the risk of blood clots and stroke. Studies show transdermal estrogen cuts VTE risk by nearly half compared to pills.The Real Benefits: More Than Just Hot Flashes
If your main problem is hot flashes, HRT is still the gold standard. The Women’s Health Initiative found it reduces hot flash frequency by 75% compared to placebo. Real women report going from 20 flashes a day to two or three in under two weeks. That’s not a placebo effect-that’s life-changing. Bone health is another major win. Estrogen protects your bones. Without it, bone loss accelerates. After menopause, women can lose up to 20% of their bone density in the first five years. HRT slows that down. Women on HRT for five to eight years often show stable bone density on DEXA scans. Those who skip it? They’re far more likely to fracture a hip or spine later on. There’s also emerging evidence that timing matters. Starting HRT within 10 years of your last period-or before age 60-appears to lower heart disease risk. A 2025 study of 120 million patient records found women who started estrogen during perimenopause had 18% fewer heart events than those who waited until after menopause was complete. This isn’t about preventing heart disease in older women. It’s about protecting your heart when you’re still young enough for estrogen to help.The Risks: What You’re Not Being Told
Let’s be clear: HRT isn’t risk-free. But the risks aren’t the same for everyone. Breast cancer risk rises slightly with long-term use. The data shows estrogen-progestogen therapy adds about 29 extra cases per 10,000 women per year. That sounds scary. But compare it to smoking (which adds 150+ cases) or being overweight (adds 50+). For women on estrogen-only therapy (no uterus), the increase is just 9 extra cases per 10,000-almost negligible. Stroke risk? Higher with oral estrogen. Transdermal estrogen cuts that risk by 30%. Blood clots? Same story. Pills increase VTE risk to 3 per 1,000 women per year. Patches? Around 1.3 per 1,000. That’s why experts now say: if you’re going to take HRT, go transdermal. Gallbladder disease? Slightly higher with pills. Mood swings? Sometimes. Bloating? Common at first. These side effects often fade with dose adjustments. Many women quit HRT because they were given a high dose of oral Prempro and told to tough it out. That’s not the standard anymore. The biggest risk? Not taking it when you need it. Women who avoid HRT due to fear often end up with worse outcomes: more fractures, more severe hot flashes, more depression, and poorer quality of life.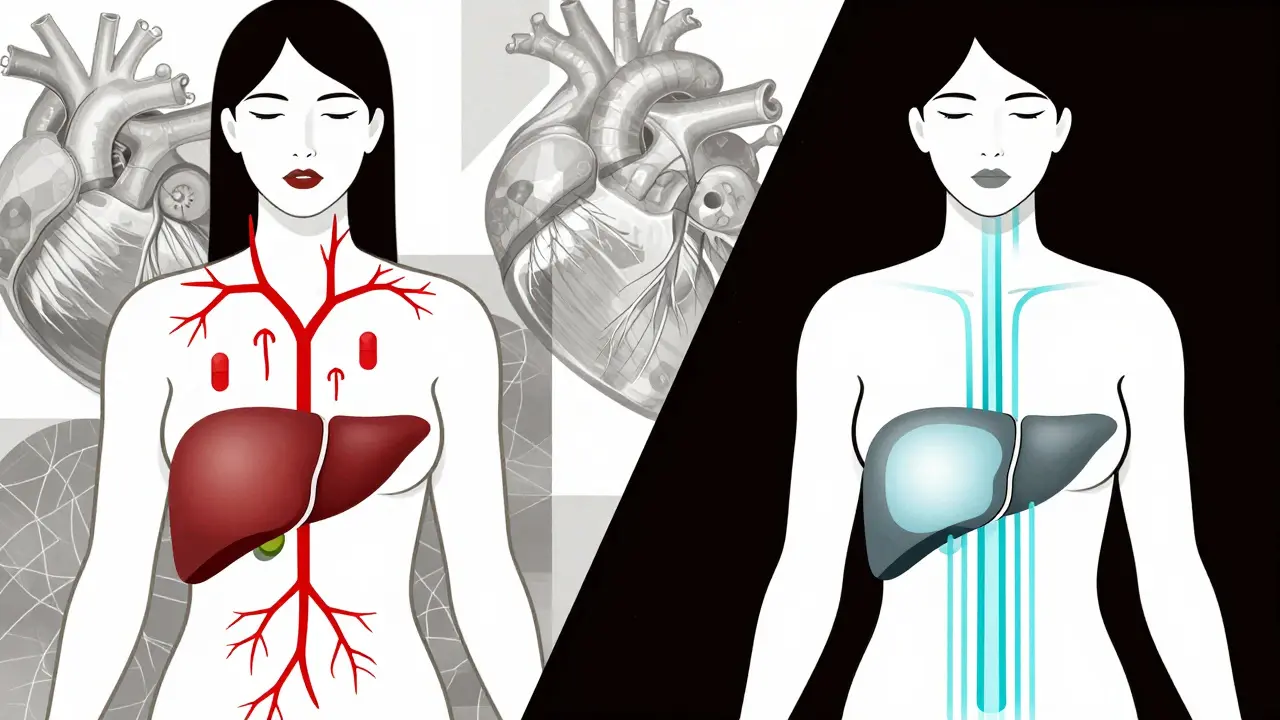
Who Should Avoid HRT Altogether
HRT isn’t for everyone. You should avoid it if you have:- A history of breast cancer (especially estrogen-receptor positive)
- Current or past blood clots (deep vein thrombosis or pulmonary embolism)
- History of stroke or heart attack
- Unexplained vaginal bleeding
- Severe liver disease
Alternatives That Don’t Work as Well
You’ve heard about black cohosh, soy isoflavones, and CBD oil. They’re everywhere. But here’s the truth: none come close to HRT. SSRIs like paroxetine can reduce hot flashes by 50-60%. That sounds good-until you realize HRT does 75-90%. And SSRIs come with side effects: weight gain, low libido, nausea. Gabapentin helps about 45% of women, but leaves a quarter dizzy or drowsy. Phytoestrogens? A Cochrane Review found they reduce hot flashes by just half a flash per day compared to placebo. That’s barely noticeable. Lifestyle changes-cooling your room, cutting caffeine, practicing mindfulness-help a little. But for severe symptoms? They’re not enough.Getting Started: What to Ask Your Doctor
Don’t just accept a prescription. Ask these questions:- Am I within 10 years of my last period or under 60? (That’s the sweet spot for benefit over risk.)
- Should I use estrogen alone or with progestogen? (Depends on whether you have a uterus.)
- Is transdermal the best option for me? (Usually yes, unless you have skin sensitivities.)
- What’s the lowest dose that works? (Start low-0.5 mg estradiol or 0.3 mg conjugated estrogens daily.)
- How will we monitor me? (Blood pressure, breast exams, bone density every 2-3 years.)

What Happens When You Stop
Many women stop HRT after a year or two because they’re scared. But symptoms often return-and sometimes worse than before. That’s normal. Estrogen isn’t addictive. But your body got used to having it. If you want to stop, don’t quit cold turkey. Taper slowly. Drop the dose by 25% every 4-6 weeks. Some women stay on low-dose patches for 5-10 years without issue. Others stop after 2 years and manage with non-hormonal tools. There’s no rule that says you have to stop at five years. The old “five-year limit” was based on outdated fear, not data. If you’re still symptomatic, healthy, and under 60, staying on HRT is a reasonable choice.The Future: Personalized Hormone Therapy
The next big shift? Personalization. By 2030, genetic tests may tell you how fast your body breaks down estrogen. Some women metabolize it slowly-meaning they need lower doses. Others clear it fast and need more. Right now, we guess. Soon, we’ll know. New formulations are coming too. TSECs (tissue-selective estrogen complexes) like Duavee combine estrogen with a compound that protects the breast and uterus without needing progestogen. They’re pricier, but they’re an option for women who can’t tolerate progesterone. The message from experts is clear: HRT isn’t the villain it was made out to be in 2002. It’s a tool. And like any tool, it’s dangerous in the wrong hands-but lifesaving in the right ones.Is hormone therapy safe for women over 60?
For women over 60 or more than 10 years past menopause, hormone therapy is generally not recommended for symptom relief or disease prevention. The risks-especially for stroke, blood clots, and breast cancer-outweigh the benefits at this stage. If you’re over 60 and still having severe symptoms, non-hormonal options like low-dose SSRIs, gabapentin, or cognitive behavioral therapy are safer choices. Always discuss your individual risk profile with your doctor.
Does HRT cause weight gain?
HRT itself doesn’t directly cause weight gain. Weight gain during menopause is mostly due to aging, reduced muscle mass, slower metabolism, and changes in fat distribution. Some women report bloating or fluid retention when starting HRT, especially with oral pills. This usually fades within a few months. Transdermal estrogen is less likely to cause this. If you’re gaining weight, focus on strength training and protein intake-these are far more effective than stopping HRT.
How long should I stay on hormone therapy?
There’s no fixed time limit. The goal is to use the lowest dose for the shortest time needed to manage symptoms. For most women, that’s 2-5 years. But if you’re still having severe hot flashes, night sweats, or bone loss after five years-and you’re under 60 and healthy-continuing is reasonable. Many women stay on low-dose transdermal estrogen for 7-10 years without increased risk. Regular check-ups with your doctor are key to reassessing your needs.
Can I use HRT if I have a family history of breast cancer?
It depends. If you have a strong family history or a known genetic mutation like BRCA1 or BRCA2, estrogen therapy may not be recommended, especially if you’ve had breast cancer. But if your family history is distant or you’ve tested negative for mutations, low-dose transdermal estrogen may still be an option. Talk to a specialist about your personal risk. Some women with BRCA mutations choose to have their ovaries removed early and then use short-term HRT until age 50 to protect bone and heart health.
Are natural or herbal options safer than HRT?
No. Herbal supplements like black cohosh, red clover, or soy are not regulated like prescription drugs. Their estrogen content varies wildly, and they haven’t been proven to reduce hot flashes reliably. Some can even interfere with medications or increase cancer risk in sensitive individuals. There’s no evidence they’re safer than HRT. If you want effective, predictable relief, FDA-approved hormone therapy remains the most reliable choice.
Next Steps: What to Do Today
If you’re struggling with menopause symptoms:- Track your symptoms for two weeks using a simple journal or app.
- Find a certified menopause practitioner through the North American Menopause Society’s directory.
- Ask your doctor about transdermal estrogen-don’t settle for pills unless there’s a clear reason.
- Get a bone density test if you’re over 55 and haven’t had one.
- Don’t let fear stop you from asking for help. Menopause isn’t something you have to suffer through.


Write a comment