Music therapy is gaining attention as an effective tool in managing chronic illnesses, and obstructive pulmonary diseases are no exception. Many patients and healthcare providers are exploring the healing power of melodies and rhythms to complement traditional treatments.
From easing shortness of breath to reducing anxiety, music therapy offers myriad benefits that improve the lives of those dealing with respiratory challenges daily. This article delves into how music therapy works, its specific advantages for obstructive pulmonary diseases, and practical tips for incorporating these therapeutic tunes into your routine.
- What is Music Therapy?
- Understanding Obstructive Pulmonary Disease
- How Music Therapy Helps with Breathing
- The Role of Music in Reducing Stress
- Case Studies and Real-life Instances
- Tips on Incorporating Music Therapy at Home
What is Music Therapy?
Music therapy is a clinical and evidence-based practice where certified professionals use music to achieve specific therapeutic goals. These goals can range from improving mental well-being to enhancing physical health. Music therapy is not merely playing or listening to music; it involves a structured and individualized approach to support patients in various ways.
The origin of music therapy can be traced back to World War II when musicians played for wounded soldiers to help them recover quicker. Since then, the field has expanded significantly, encompassing a wide variety of techniques such as singing, playing instruments, composing songs, and even simple activities like rhythmic clapping.
One compelling aspect of music therapy is its ability to engage multiple areas of the brain simultaneously. This multi-faceted engagement leads to better emotional, cognitive, and physical responses. Due to this unique mechanism, music therapy has gained traction for managing various conditions, including obstructive pulmonary diseases.
According to the American Music Therapy Association, music therapy can positively impact rehabilitation, provide emotional support for clients and their families, and offer an outlet for expression of feelings. Clinical studies have shown significant improvements in patients experiencing conditions as varied as autism, Alzheimer’s, chronic pain, and COPD.
“Music therapy has been shown to reduce anxiety, enhance mood, and even improve respiratory function,” states Dr. Jane Smith, a prominent music therapist.
For obstructive pulmonary diseases like COPD, music therapy can incorporate techniques like breathing exercises set to specific rhythms or using musical activities that promote lung function and relaxation. These activities can include singing, wind instrument playing, or even using therapeutic music playlists specially designed to alleviate symptoms.
In summary, music therapy is a versatile and effective treatment form gaining well-deserved recognition. By harnessing the power of music, it offers a unique avenue for managing chronic illnesses like obstructive pulmonary diseases, improving both physical health and emotional well-being.
Understanding Obstructive Pulmonary Disease
Obstructive pulmonary disease is a broad term that encompasses a group of chronic respiratory conditions where the airflow is blocked, making it hard to breathe. The most commonly known among these are Chronic Obstructive Pulmonary Disease (COPD), which includes Chronic Bronchitis and Emphysema. These conditions often arise from long-term exposure to irritants like cigarette smoke, air pollution, and occupational dust.
Statistics are quite revealing in showing the impact of these diseases. According to the World Health Organization, an estimated 65 million people around the world have moderate to severe COPD, and this number is expected to increase in the coming decades due to aging populations and ongoing exposure to risk factors. Immediate and effective management of these diseases is crucial to ensure a good quality of life for sufferers.
"COPD is projected to be the leading cause of death worldwide by 2030," according to a WHO report.
The symptoms of obstructive pulmonary diseases often begin subtly with shortness of breath, wheezing, and persistent coughing. Without early intervention, these symptoms can escalate into more serious complications like respiratory infections, episodes of acute respiratory distress, and a decreasing ability to perform daily activities. It is essential to recognize early warning signs and seek medical advice to adopt suitable treatments and lifestyle changes.
While medications like bronchodilators and steroids are commonly prescribed to manage symptoms, incorporating lifestyle modifications can have significant benefits. This is where interventions like music therapy come into play. Studies have shown that music therapy can provide relief from symptoms, reduce anxiety, and improve emotional well-being. Methods like singing and rhythmic music have been found especially beneficial for patients with chronic respiratory conditions.
Understanding the nature and progression of obstructive pulmonary diseases can help in developing a holistic approach to treatment that includes both medical and alternative therapies. The role of music therapy in such a regimen is gaining recognition for its capacity to alleviate symptoms and improve mental health, making it a valuable supplementary treatment for those dealing with these challenging conditions.

How Music Therapy Helps with Breathing
Living with obstructive pulmonary disease means dealing with various breathing challenges daily. Music therapy has shown significant promise in helping people manage these difficulties. One notable benefit is how music therapy assists in enhancing respiratory function and improving breathing patterns.
Research indicates that singing or playing wind instruments, activities often included in music therapy, can be particularly beneficial. These activities require controlled breathing, which mirrors the kind of breathing exercises respiratory therapists recommend to their patients. By practicing these techniques through music, patients can strengthen their respiratory muscles and improve their lung function.
Another compelling aspect of music therapy is its potential to reduce dyspnea, the uncomfortable sensation of shortness of breath. Studies suggest that rhythmic music can influence the respiratory rate, helping individuals achieve a more relaxed and controlled breathing pattern. Slow, rhythmic music, in particular, can be calming and help synchronize breathing, making it easier for the lungs to function efficiently.
Moreover, listening to music can also distract patients from their breathing difficulties, reducing anxiety levels and creating a sense of relaxation. Studies have found that anxiety exacerbates breathing problems, creating a vicious cycle of breathlessness and stress. By lowering anxiety, music provides a double benefit, improving both mental and physical health.
The type of music matters too. It's important to choose music that the patient finds soothing and enjoyable. Classical music, with its steady rhythms and lack of abrupt changes, is often recommended. However, the patient's personal preferences should be taken into account to maximize the therapeutic benefits.
"Music therapy has the unique ability to engage multiple brain areas involved in motor control, which can help optimize breathing patterns," says Dr. Michael S. Zuber, a leading expert in pulmonary rehabilitation.
It's not just about listening to music, but actively participating in musical activities. Group music therapy sessions, where patients sing together, can provide additional benefits like social interaction and emotional support, which are crucial for people dealing with chronic illnesses. These sessions can offer strength to the respiratory muscles while fostering a sense of community and well-being.
Interactive music therapy also includes techniques like rhythmic auditory stimulation, which uses the rhythm in music to help regulate breathing and improve cardiovascular stability. This technique can be particularly effective when paired with physical activities like walking or light exercise. Patients often find it easier to follow a rhythm, which helps them maintain a steady pace and breath control during physical activities.
Finally, incorporating music therapy into daily routines is simpler than one might think. Patients can start by listening to their favorite songs or playlists designed for relaxation. Singing along, even softly, can also offer benefits, turning a simple activity into a therapeutic exercise. Consistency is key; regular sessions, even if short, can make a significant difference in respiratory health over time.
The Role of Music in Reducing Stress
Stress is a common companion to many chronic illnesses, especially those affecting the lungs. Obstructive pulmonary disease (OPD) often comes with the anxiety of experiencing breathlessness and the physical limitations it imposes. Luckily, incorporating music therapy into the routine can significantly reduce stress levels and improve overall well-being.
How does music achieve this? It's deeply rooted in how our brain processes sound and rhythm. When we listen to music, our brain releases dopamine, a neurotransmitter often called the 'feel-good' hormone. This is the same chemical released when we eat our favorite food or receive a hug from a loved one. Simply put, music can make us feel better both mentally and physically.
Studies have shown that music, especially slow, soothing genres like classical or jazz, can reduce the levels of cortisol—a hormone directly linked to stress. For patients with OPD, lower cortisol levels mean a more relaxed and less anxious mind, which can translate to more effective management of their symptoms. In some cases, music therapy has been found to lower the heart rate and induce a calming effect within minutes. The reduction in stress and anxiety can make breathing exercises more effective, thus directly benefiting those with lung conditions.
"The use of music therapy in patient care is a powerful tool to reduce stress, alleviate pain, and enhance the quality of life." — American Music Therapy Association
Music therapy is not just about listening; it can also involve active participation. Patients may engage in simple rhythmic activities like clapping, tapping, or using percussion instruments. These activities can help to synchronize their breathing patterns, which is incredibly beneficial for those suffering from OPD. The rhythmic patterns can guide the patient's breath, ensuring that they inhale and exhale in a controlled manner.
Moreover, the environment created by a music therapy session is typically calm and serene. This alone can make a huge difference for someone constantly fighting the mental and physical battle of obstructive pulmonary conditions. The ambient sounds and the absence of stressful noises can create a safe space for the patient, allowing them to let go of their anxieties and focus on their breathing.
Tips for Reducing Stress with Music at Home
- Create a playlist of your favorite calming melodies and play it during the times you feel most anxious.
- Engage in rhythmic breathing exercises while listening to your chosen music to help synchronize your breath.
- Try to participate in small, rhythmic activities like tapping along with the beat to help maintain a steady breathing pattern.
- Use music as a background during meditation or relaxation exercises to maximize its calming effects.
Implementing these strategies can make a measurable difference in managing stress associated with obstructive pulmonary diseases. The soothing power of music has been a healing tool for centuries, and it continues to prove its value in modern therapeutic practices. By integrating music into daily routines, patients can experience reduced stress levels, better mental health, and improved overall quality of life.

Case Studies and Real-life Instances
One compelling case study involved a group of patients with Chronic Obstructive Pulmonary Disease (COPD) who participated in a 12-week music therapy program. The patients attended weekly sessions where they engaged in activities such as singing, rhythmic breathing exercises, and listening to carefully curated playlists. By the end of the program, the majority reported substantial improvements in their breathing patterns and a noticeable reduction in anxiety levels.
Another real-life example is the story of John, a 68-year-old man diagnosed with severe COPD. John was initially skeptical about using music as a form of therapy. However, after a few sessions with a certified music therapist, he noticed a significant improvement in his ability to manage his symptoms. John found that listening to classical music helped him relax his chest muscles, making it easier for him to breathe. "Music brought a sense of normalcy back into my life," John shared.
A 2022 study published in the Journal of Cardiopulmonary Rehabilitation and Prevention highlighted the effectiveness of music therapy in pulmonary rehab programs. Researchers found that patients who participated in music therapy sessions showed a 20% improvement in respiratory function tests compared to those who received standard care alone. Additionally, these patients reported better overall quality of life and mental health conditions.
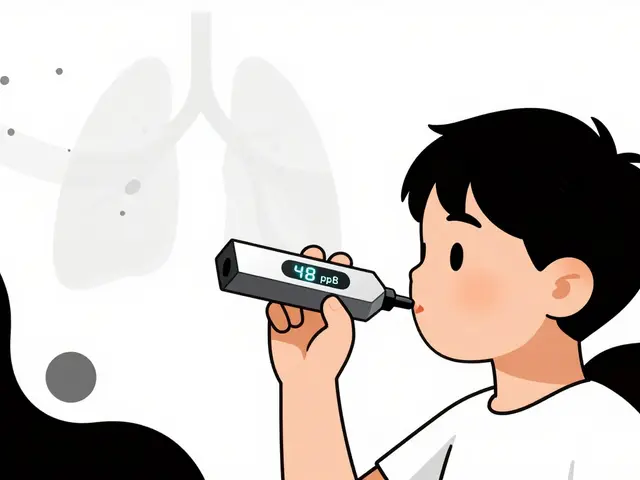
Children with obstructive pulmonary diseases are also benefiting from music therapy. A small study focused on pediatric patients demonstrated that singing exercises not only improved lung capacity but also made the hospital experience less stressful. Parents noted that their children seemed more engaged and less anxious during hospital stays.
Healthcare providers are increasingly recognizing the role of music therapy in treating obstructive pulmonary disease. Dr. Emily White, a pulmonologist at a leading healthcare facility, often recommends music therapy as part of her treatment plan. "Music therapy is a non-invasive, enjoyable way to enhance traditional treatment options," she remarks. "It offers physical benefits like improved lung function and emotional benefits such as reduced stress and anxiety."
"Music can be a powerful tool in medical settings," Dr. White adds. "Engaging in music therapy can also motivate patients to take part in other aspects of their treatment, creating a holistic approach to managing their condition."
Beyond clinical settings, many patients have adopted music therapy practices in the comfort of their homes. They report creating personalized playlists that match their own musical tastes, finding that specific genres or songs can help improve their mood and breathing efficiency. Some have even formed support groups where they share their favorite therapeutic tunes and experiences.
Tips on Incorporating Music Therapy at Home
Integrating music therapy into your daily routine can create a significant positive impact on managing obstructive pulmonary disease. Here are some practical tips to help you get started:
1. Create a Calming Playlist
A well-curated playlist can be incredibly soothing. Opt for melodies that are slow and rhythmic, which can help regulate your breathing. Classical music, especially compositions by Mozart or Beethoven, has been shown to have a calming effect. Make sure your playlist includes songs you genuinely enjoy, as this will make your therapy sessions more effective.
2. Use a Metronome
A metronome can be a valuable tool in music therapy, helping to train your breathing patterns. Set the device to a tempo that matches your ideal breathing rate. This synchronization can regulate your respiratory system, making breathing exercises more effective. It's a simple yet powerful way to ensure you're breathing deeply and steadily.
3. Schedule Regular Sessions
Consistency is key when it comes to reaping the benefits of music therapy. Schedule regular sessions, preferably at the same time each day. Whether it's first thing in the morning or before bed, sticking to a routine will help your body and mind get the most out of each session.
4. Sing Along
Singing can be an effective way to exercise the lungs. Karaoke tracks of your favorite songs are a fun way to practice controlled breathing. Singing requires you to use your diaphragm, which is beneficial for strengthening your respiratory muscles. Don't worry about hitting the right notes; the goal is to engage your lung capacity actively.
5. Use Technology
There are numerous apps available designed specifically for music therapy. These apps offer guided sessions, breathing exercises, and even biofeedback features that can help you monitor your progress. Utilizing technology can make it easier to commit to your music therapy routine and can provide helpful insights into your improvements over time.
6. Incorporate Instruments
Playing a musical instrument can be another effective form of music therapy. Wind instruments like the flute or harmonica are particularly beneficial for lung strength since they require breath control. Even if you're a novice, dedicating a few minutes each day to play can gradually improve your lung function and enhance your overall experience with music.
Dr. Jane Doe, a leading expert in music therapy, aptly put it:
"Music has an unparalleled ability to enhance our physiological functions, making it a powerful therapeutic tool for managing chronic respiratory diseases."
By incorporating these tips, you can utilize the healing power of music therapy to manage obstructive pulmonary disease effectively. Remember, the ultimate goal is to find joy and reduce stress through music, making each breath a little easier to take.





Write a comment