When someone starts hearing voices that aren’t there, or becomes convinced that strangers are watching them, it’s not just paranoia-it could be the early stages of psychosis. Many people don’t realize these signs are treatable, especially when caught early. The truth is, psychosis isn’t a life sentence. With the right support, most people can get back to school, work, and meaningful relationships. But time matters. Every week without treatment makes recovery harder.
What Exactly Is Psychosis?
Psychosis isn’t a diagnosis on its own. It’s a symptom-a break from reality that can show up in schizophrenia, bipolar disorder, severe depression, or even after drug use or extreme stress. People experiencing psychosis might hear, see, or feel things others don’t. They might believe things that aren’t true, like being followed or controlled by outside forces. Their thoughts can race or stall, making conversations confusing. Speech might jump from topic to topic, or stop mid-sentence. It’s not weakness. It’s a brain-based condition, and it’s more common than you think.
One in 100 people will experience psychosis before age 30. The average person waits nearly two years before getting help. That’s 74 weeks of untreated symptoms. And the longer it goes without care, the more damage it does. Studies show each extra month without treatment reduces the chance of full recovery by 3-5%. But here’s the good news: early intervention changes everything.
Early Warning Signs You Can’t Ignore
Psychosis doesn’t start with hallucinations. It creeps in slowly. The first signs are subtle-so subtle, many dismiss them as stress, teenage moodiness, or laziness. But they’re red flags.
- A sudden drop in grades or job performance, even if the person used to be high-achieving
- Withdrawal from friends and family-staying in their room, skipping meals, avoiding eye contact
- Unusual beliefs: thinking TV news is sending secret messages, or that neighbors are plotting against them
- Strange sensory experiences: hearing whispers when no one’s around, feeling bugs crawling on skin, seeing shadows move
- Confused thinking: jumping between unrelated topics, talking in riddles, forgetting words mid-sentence
- Mood swings: extreme anxiety, unexplained anger, or flat emotions-no joy, no sadness, just numbness
- Poor hygiene: stopping showering, wearing the same clothes for days, neglecting basic self-care
These signs don’t mean someone has psychosis. But if three or more last more than two weeks, it’s time to act. A 2023 study found that 78% of first-episode psychosis cases showed a clear decline in school or work before full-blown symptoms appeared. That’s a window-usually 6 to 12 months-where early help can stop things from getting worse.
Coordinated Specialty Care: The Gold Standard Treatment
For decades, psychosis was treated with pills and hospital stays. That approach often failed. People dropped out. Jobs were lost. Relationships broke. Then came Coordinated Specialty Care (CSC)-a team-based, person-centered model built for first-time psychosis.
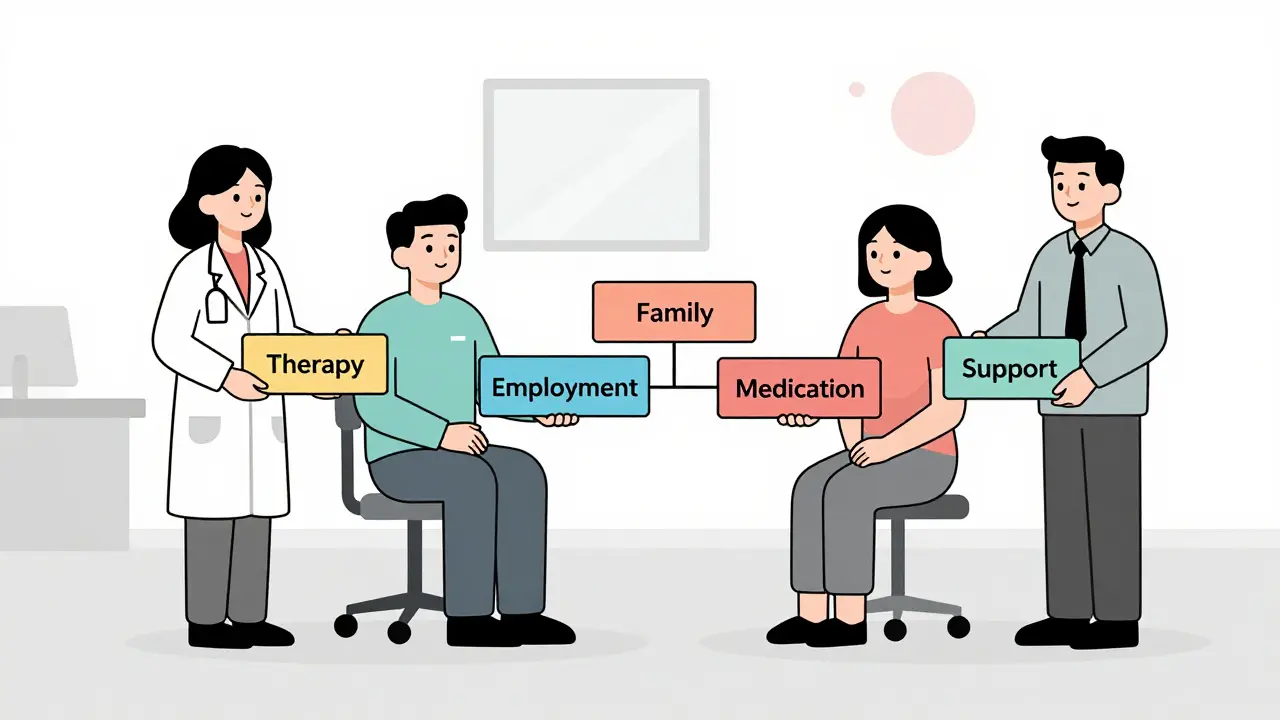
CSC isn’t one thing. It’s five evidence-backed pieces working together:
- Case management: A dedicated case worker visits the person at home, helps with appointments, bills, transportation. Staff-to-client ratios are kept at 1:10 to ensure real support.
- Family education: Families aren’t bystanders. They get 12 to 20 weekly 90-minute sessions to learn about psychosis, how to communicate, and how to reduce stress at home.
- Individual therapy: Cognitive Behavioral Therapy for Psychosis (CBTp) helps people question strange beliefs without dismissing them. It’s not about ‘fixing’ the person-it’s about rebuilding their sense of control.
- Supported education and employment: 80% of CSC participants return to school or work within three months. Job coaches help with resumes, interviews, and workplace accommodations.
- Medication management: Antipsychotic meds are used, but at low doses-25-50% of standard adult levels-and only if needed. The goal is symptom relief, not sedation.
People in CSC programs are 58% more likely to see their hallucinations and delusions fade. They’re 42% more likely to keep up with school or work. And they’re 35% more likely to stick with treatment. That’s not just improvement-it’s transformation.
Why Timing Is Everything
The ‘golden hour’ for psychosis isn’t the first hour-it’s the first 72 hours after someone starts showing clear warning signs. That’s when referral to a CSC program should happen. Delayed care doesn’t just mean longer symptoms. It means more hospitalizations, more lost income, more family strain.
One program in Oregon, EASA, cut the average time between first symptoms and treatment from 112 weeks to just 26 weeks by training teachers, pediatricians, and coaches to spot early signs. Schools started screening students with the 16-item Prodromal Questionnaire (PQ-16). A score of 8 or higher triggered a referral. The result? More people got help before they crashed.
Dr. Lisa Dixon from Columbia University says each month of untreated psychosis increases recovery time by 5-7%. That’s why early action isn’t optional-it’s survival.
Barriers to Getting Help
Despite the science, most people still don’t get CSC. Only 42% of those with first-episode psychosis receive it within two years. Why?
- Stigma: Families fear labeling someone as ‘crazy.’ They wait, hoping it’s just a phase.
- Lack of awareness: Doctors, teachers, even therapists miss the signs. Psychosis isn’t taught well in medical schools.
- Access: Only 28% of rural counties in the U.S. have CSC programs. Urban areas have 84% coverage.
- Funding: Many programs rely on short-term grants. 38% report financial instability.
And there’s another problem: false positives. Screening tools can flag 30-40% of teens who don’t actually develop psychosis. That’s why experts stress: don’t rush to medication. Start with therapy, family support, and monitoring. Medication should be a last step, not the first.

What’s Changing Now
Things are improving. The 21st Century Cures Act requires Medicaid to cover CSC by 2025. Thirty-two states already have billing codes for it. The federal government spent $27.8 million in 2022 to expand programs. The new EPINET network is tracking 15 key outcomes across 200+ clinics-and early data shows 63% of participants achieve remission within a year.
Research is also moving faster. Scientists have found 12 blood markers that predict psychosis with 82% accuracy. Mobile apps like PRIME Care help people track moods and sleep. Telehealth brings CSC to rural areas. But tech alone won’t fix this. Human connection still matters most.
Right now, a study called RAISE-3 is testing how to make CSC work better for Black, Latino, and Indigenous communities. Right now, Black Americans wait 2.4 times longer for help than white Americans. That’s not a gap in care-it’s a failure of equity.
What to Do If You Suspect Psychosis
If you’re worried about yourself or someone you love:
- Don’t wait. Don’t assume it’s ‘just stress.’
- Find a local CSC program. Search the National Alliance on Mental Illness (NAMI) website or call 1-800-950-NAMI.
- Go to a primary care doctor and ask for a referral to a psychosis early intervention clinic.
- Bring a family member. They’ll need support too.
- Don’t insist on medication right away. Ask about therapy, family education, and supported work or school first.
Psychosis doesn’t have to mean a life on disability. With the right care, most people return to their lives-with stronger relationships, better coping skills, and a future they thought was lost.
Can psychosis be cured?
Psychosis isn’t ‘cured’ like an infection, but it can be managed effectively. With early intervention through Coordinated Specialty Care, up to 63% of people achieve symptom remission within a year. Many return to school, work, and independent living. The goal isn’t to erase the experience-it’s to rebuild a life around it.
Is medication always necessary for psychosis?
No. Medication is one tool, not the only one. Coordinated Specialty Care starts with therapy, family support, and education. Antipsychotics are only added if symptoms are severe or persistent, and even then, they’re started at low doses. The focus is on minimizing side effects and maximizing function-not sedation.
How long does Coordinated Specialty Care last?
Most CSC programs last 2 to 3 years, with the most intensive support in the first 6 to 12 months. After that, care gradually tapers as the person gains stability. The goal is to transition to regular mental health care or community services-without losing support.
Can teens get Coordinated Specialty Care?
Yes. CSC is designed for people aged 15 to 40 experiencing their first episode of psychosis. Programs tailor services to teens and young adults, including school accommodations, peer support groups, and family counseling. Early treatment during adolescence leads to the best long-term outcomes.
What if I can’t find a CSC program near me?
Call NAMI (1-800-950-NAMI) or the Substance Abuse and Mental Health Services Administration (SAMHSA) helpline at 988. They can connect you to local resources, even if a full CSC program isn’t available. Telehealth options are expanding, and some clinics offer remote case management. Don’t wait-start with a primary care doctor or school counselor.
Is psychosis hereditary?
Genetics play a role, but they’re not destiny. Having a parent with schizophrenia increases risk to about 10%, but 90% of people with psychosis have no family history. Environmental factors-like trauma, drug use, chronic stress-often trigger the condition in those with biological vulnerability.
Can substance use cause psychosis?
Yes. Marijuana, especially high-potency strains, methamphetamine, and hallucinogens can trigger psychotic episodes, even in people without prior mental illness. In some cases, these episodes resolve after stopping use. But in others, they become the start of a longer-term condition. That’s why early screening includes substance use history.
How do I know if it’s psychosis or just anxiety?
Anxiety causes worry, racing thoughts, and physical tension. Psychosis involves a break from reality: hearing voices, believing in impossible things, or feeling like thoughts are being inserted or removed. If someone can’t tell what’s real anymore-even if they’re scared or confused-it’s time for a professional assessment. Don’t guess. Get help.



Write a comment