When a patient picks up a generic version of their blood pressure pill and suddenly feels dizzy, nauseous, or develops a rash, most people assume it’s just a side effect. But what if it’s not? What if the generic version, though legally approved as "therapeutically equivalent," is causing a reaction that the brand-name drug never did? That’s where pharmacists come in - not just as dispensers, but as the last line of defense in catching hidden safety issues before they hurt more people.
Why Generic Medications Need Extra Scrutiny
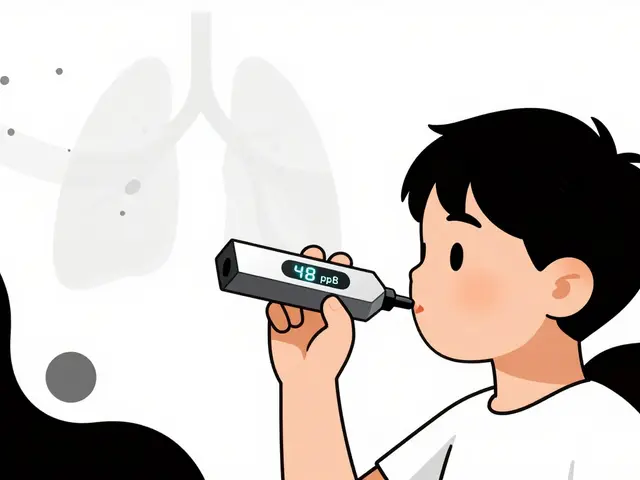
Generic drugs are supposed to be identical to their brand-name counterparts in active ingredients, strength, dosage, and effect. But "identical" doesn’t mean "exactly the same." The FDA requires generics to have the same active ingredient and be bioequivalent - meaning they deliver the same amount of drug into the bloodstream within a narrow range. But what’s not required to be identical? The fillers, dyes, preservatives, and other inactive ingredients - called excipients. These excipients can trigger allergic reactions or interfere with absorption in sensitive patients. A 2022 study in the Journal of the American Pharmacists Association found that 1 in 5 patients reporting unexpected side effects after switching to a generic had symptoms that disappeared when they switched back. Many of these cases went unreported because neither the patient nor the prescriber suspected the generic was the culprit. Pharmacists are often the first to notice these patterns. They see the same patient come back multiple times with the same complaint after a generic switch. They know the patient’s full medication history. They’ve counseled them on side effects before. That makes them uniquely positioned to spot when something doesn’t add up.What Pharmacists Are Legally Required to Do
The rules vary by state and country, but the core responsibility is the same: if you suspect a drug caused harm, you must report it. In British Columbia, pharmacists are legally required under the Health Professions Act to report any suspected adverse drug reaction to Health Canada, notify the prescriber, and document it in PharmaNet. It’s not optional. It’s part of their professional duty. In the U.S., federal law doesn’t force pharmacists to report - but the FDA strongly urges it, especially for serious reactions. The FDA defines serious as: hospitalization, life-threatening conditions, permanent disability, birth defects, or death. Even if you’re not sure, if there’s a reasonable chance the drug caused it, you should report. And here’s the catch: most reports to the FDA’s FAERS database come from drug manufacturers, not healthcare providers. That means if you don’t report, the data gap stays wide. A single pharmacist’s report can be the first clue that a whole batch of generics has a hidden problem.The Real Barrier: Time and Awareness
You might be thinking: "I’m already swamped. I don’t have time to fill out forms." You’re not alone. A 2021 survey by the National Community Pharmacists Association found that 78% of pharmacists spend 15 to 30 minutes per adverse event report. That’s time away from counseling, filling scripts, or just catching your breath. And 62% said they simply don’t have enough time during the workday to do it properly. But the bigger issue isn’t time - it’s awareness. Many pharmacists don’t know what counts as reportable. Is a headache after a new generic worth reporting? What about diarrhea? The answer: if it’s unexpected, and you think it might be linked to the medication, yes. The British Columbia Pharmacists Association calls under-reporting a "recognized problem" - and it’s not just because pharmacists are busy. It’s because many don’t know how to distinguish between expected side effects and true adverse reactions. A patient might get nausea on a new statin - that’s common. But if they get a rash and swelling after switching from one generic to another? That’s not expected. That’s a signal.
How to Report: Simple Steps
You don’t need to be a researcher to report. Here’s how to do it right:- Recognize the red flag: Patient reports new symptoms after switching to a generic. Symptoms don’t match the known side effect profile. Multiple patients report similar issues with the same generic.
- Document everything: Patient name (or identifier), drug name (including manufacturer), dose, start date, symptoms, onset time, duration, outcome, and any other meds they’re on. Even if you’re not sure, write it down.
- Report it: In the U.S., use the FDA’s MedWatch Online portal. In Canada, use Health Canada’s online form. Many states now integrate reporting into pharmacy software - check if yours does.
- Follow up: Tell the prescriber. Ask the patient if they’re willing to switch back to the brand or another generic. Track if symptoms improve.
Why This Matters for Generic Safety
Generic drugs save billions in healthcare costs. That’s good. But assuming they’re all perfectly safe because they’re "equivalent" is dangerous. A 2022 study showed that only 5-10% of all adverse drug reactions are reported. For generics, the rate is likely even lower. Why? Because prescribers assume the drug is the same. Patients assume it’s just their body adjusting. Pharmacists assume someone else will report it. But here’s what happens when reports pile up: Health Canada issues safety alerts. The FDA investigates manufacturers. Companies reformulate. Pharmacies stop stocking problematic batches. Patients are protected. Without pharmacist input, those alerts never come. The system relies on frontline observations - and pharmacists are the only healthcare professionals who see every patient, every drug, every switch.What’s Changing - And What’s Coming
The tide is turning. California and Texas have already integrated reporting tools into pharmacy management systems, cutting reporting time by 40%. The FDA’s Sentinel Initiative is now pulling data from community pharmacies to detect safety signals in real time. In Europe, mandatory reporting for all healthcare professionals since 2012 led to a 220% increase in reports. Now, U.S. industry analysts predict that by 2025, 75% of states will adopt rules similar to British Columbia’s - making reporting not just encouraged, but required. This isn’t about adding paperwork. It’s about closing a dangerous blind spot in our drug safety system. Generics are not all created equal in practice - even if they are in theory. And pharmacists, with their unique access and clinical insight, are the only ones who can spot the difference.What You Can Do Today
- Check your pharmacy’s reporting system. If it doesn’t have a built-in tool, go to MedWatch Online or Health Canada’s portal and bookmark it. - Talk to your manager. Ask if training on ADR recognition is available. - Next time a patient says, "This generic doesn’t feel right," don’t dismiss it. Ask: "When did you start it? What changed?" Write it down. Report it. - Share this with your colleagues. Under-reporting is a team problem - and it takes a team to fix it. Your signature on a report might not change your day. But it could change someone else’s life.Do pharmacists have to report adverse events from generic drugs?
In some places like British Columbia, yes - it’s a legal requirement. In the U.S., federal law doesn’t mandate it, but the FDA strongly encourages reporting, especially for serious reactions. Even if not required, failing to report when you suspect harm could be seen as a breach of professional duty. Pharmacists are uniquely positioned to catch issues others miss, and their reports are critical for drug safety.
What counts as an adverse event worth reporting?
Any unexpected, harmful reaction linked to a medication. This includes symptoms like rash, dizziness, nausea, or changes in heart rate that appear after starting or switching a generic drug. Serious events include hospitalization, life-threatening reactions, permanent disability, or death. Even if you’re unsure, if the reaction doesn’t match the known side effects, report it. The agencies analyze patterns - your single report could be the first clue.
Can inactive ingredients in generics cause reactions?
Yes. While the active ingredient must match the brand-name drug, the fillers, dyes, and preservatives (excipients) can differ. Some patients are allergic to certain dyes like FD&C Red No. 40 or lactose-based fillers. Others may have absorption issues due to different binders. These differences are rarely tested in bioequivalence studies, which is why pharmacists often spot problems first.
How long does it take to file an adverse event report?
It typically takes 15-30 minutes, depending on how much detail you have. Many pharmacy systems now have built-in reporting tools that auto-fill patient and drug info, cutting time in half. The FDA’s MedWatch Online portal is designed for quick submission - you just need to answer key questions about the reaction, drug, and patient.
What happens after I report an adverse event?
Your report goes into a national database like the FDA’s FAERS or Health Canada’s database. Analysts look for patterns - if multiple reports come in about the same generic drug from different locations, it triggers an investigation. Manufacturers may be asked to explain, reformulate, or issue warnings. In some cases, the product is pulled from the market. Your report helps protect future patients.
Can reporting lead to liability for pharmacists?
No. Reporting in good faith is protected under law in most jurisdictions. The goal is to improve safety, not assign blame. In fact, failing to report when you have reason to suspect harm could expose you to professional liability. Regulatory bodies view reporting as part of the pharmacist’s duty of care.
Are there tools to make reporting easier?
Yes. Many pharmacy management systems now integrate with MedWatch or Health Canada’s portal. The National Association of Boards of Pharmacy has partnered with state boards to embed reporting into software used by over 30 states. This reduces reporting time by up to 40%. Ask your vendor if your system supports automated reporting - if not, push for it.






Write a comment