Every year, millions of Medicare beneficiaries get a free, in-depth review of all their medications - but most don’t show up ready for it. And that’s a problem. If you’re taking multiple pills, supplements, or over-the-counter drugs, skipping proper preparation for your Medicare Annual Medication Review could mean missing dangerous interactions, paying more than you need to, or even ending up in the hospital. This isn’t just a chat with a pharmacist. It’s a legally required, structured review that can save your health - if you do it right.
What Exactly Is a Medicare Annual Medication Review?
The official name is a Comprehensive Medication Review (CMR). It’s not optional. By law, every Medicare Part D plan must offer this service at least once a year to people who qualify. The goal? To make sure every pill, capsule, cream, or herbal supplement you take is safe, necessary, and working the way it should.
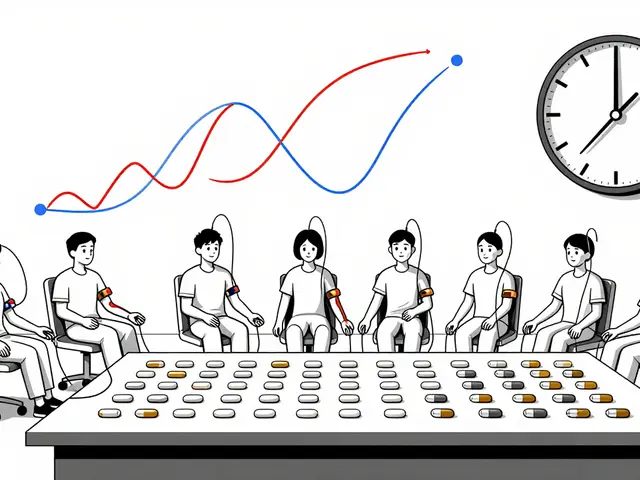
The review covers everything: prescription drugs, pain relievers like ibuprofen, antacids, fish oil, ginseng, melatonin, even vitamins you think are harmless. A licensed pharmacist sits down with you - in person or over video - and goes through each one. They check for duplicates, harmful interactions, side effects you might not have mentioned, and whether you’re actually taking them as prescribed.
It’s not a quick 10-minute chat. The CMS requires a full interactive session, followed by a written summary: a Consultation Letter, a Medication Action Plan, and a Personal Medication List. You get copies of all three. This isn’t just paperwork - it’s your roadmap for safer medication use.
Who Qualifies for the Review?
You don’t automatically get one. To qualify in 2025, you need to meet these three criteria:
- You have at least three chronic health conditions - like diabetes, heart disease, high blood pressure, COPD, or arthritis.
- You’re taking at least two to eight Part D-covered prescription medications, including maintenance drugs.
- You’ve spent at least $1,623 out of pocket on covered Part D drugs in the past year.
That last number dropped from $2,042 in 2024. That means more people qualify now. If you’re on multiple medications and paying a few hundred dollars a year for them, you’re likely eligible. Your plan will send you a letter if you qualify - but don’t wait for it. Call your plan if you’re unsure.
Even if you don’t meet the official criteria, many plans will still offer a review if you ask. It’s worth it.
Why Preparation Makes All the Difference
A 2024 analysis of 247 Medicare beneficiary reviews found that 78% of people who came prepared rated their CMR as “very helpful.” Only 42% of those who didn’t bring their meds did.
Why? Because pharmacists rely on what you tell them. If you forget your blood pressure pill or don’t mention the melatonin you take every night, they can’t spot the problem. One woman in Sydney missed a dangerous interaction between her blood thinner and daily fish oil - until she brought her bottles to the review. The pharmacist caught it. She stopped the combo. No stroke. No ER visit.
Another man thought his stomach pain was just aging. He didn’t mention the daily aspirin he took for “heart health.” The pharmacist realized it was causing a bleeding ulcer. He switched him to a safer option.
These aren’t rare cases. They’re the norm. Preparation turns a routine check-in into a life-saving conversation.
Step-by-Step: How to Get Ready for Your Review
You don’t need to be a medical expert. Just follow these steps. Set aside 60 to 90 minutes the week before your appointment.
- Gather every medication you take - in their original bottles. This includes prescriptions, OTC drugs (like Tums, Advil, or NyQuil), vitamins, supplements, herbal remedies, and even topical creams or patches. Don’t rely on memory. Don’t use a pill organizer. Bring the actual bottles.
- Take photos of each label - just in case. If a bottle is empty or lost, your photos will help the pharmacist identify the drug, dose, and frequency.
- Write down your questions - be specific. Examples: “Why am I taking this?” “I feel dizzy after I take this - is that normal?” “Can I switch to a cheaper version?” “Is this still needed?”
- Track your adherence - have you missed doses? Forgotten to take something? Had side effects like nausea, confusion, or falls? Write them down. Even small things matter.
- Bring your recent lab results - especially if you’ve had blood tests in the last 3 months. Kidney or liver function tests can show if your meds are stressing your body.
- Bring someone with you - a spouse, child, or friend. People forget things under pressure. A second set of ears helps.
- Make a timeline - list each medication, when you started it, and any changes (dose increase, new doctor, hospital stay). This takes 20 minutes but gives the pharmacist context they can’t get from a bottle.
Pro tip: If you take 8+ medications, plan for 90 minutes. If you take 4-7, 45 minutes is enough. Don’t rush. This is your health.

What Happens During the Review?
The pharmacist will:
- Compare your list with what’s in your plan’s records - they often get data from claims, but it’s not always accurate.
- Check for duplicate drugs - like taking two different painkillers that both contain acetaminophen.
- Look for interactions - for example, statins with grapefruit juice, or blood thinners with NSAIDs.
- Assess whether any meds are no longer needed - especially if you’ve changed doctors or had surgery.
- Discuss cost - many drugs have cheaper generics or patient assistance programs.
- Ask about side effects - even ones you think are “just part of getting older.”
- Give you a written Medication Action Plan - this tells you what to change, stop, or start, and when.
You’ll leave with a Personal Medication List - updated, accurate, and easy to carry. Keep it in your wallet. Show it to every new doctor.
What If You’re Not Eligible?
If you don’t meet the Medicare criteria, you’re not out of luck. Many community pharmacies offer free medication reviews - just ask. Independent pharmacists often do them for seniors, even without Medicare requirements. Some AARP chapters or local senior centers host monthly med reviews too.
Or, ask your primary care doctor for a “medication reconciliation” during your next visit. It’s not the same as a CMR, but it’s still better than nothing.
Common Mistakes People Make
Based on feedback from thousands of beneficiaries, here’s what goes wrong:
- Bringing only prescriptions - forgetting OTC drugs and supplements. These cause 30% of dangerous interactions.
- Not bringing bottles - saying “I take 10 mg of lisinopril” but it’s actually 20 mg. The pharmacist can’t verify.
- Not preparing questions - walking in thinking “I’ll just ask if I need all these.” By the end, you’ve forgotten what you wanted to ask.
- Going alone - you’re nervous. You miss key details. Someone else remembers what you didn’t.
- Not following up - the action plan says “stop the naproxen.” You don’t. A month later, you’re back with stomach bleeding.
Don’t be that person. Do the prep. It’s not hard. It’s just important.

Real Results - What People Gain
Studies show CMRs reduce hospitalizations by up to 20% in high-risk seniors. They cut medication costs by an average of $300 per year by switching to generics or eliminating unnecessary drugs.
One 78-year-old man in Melbourne was taking seven pills a day. After his CMR, two were stopped (they weren’t helping), one was switched to a cheaper version, and he was advised to take his blood pressure pill in the morning instead of at night - which fixed his dizziness. His monthly out-of-pocket cost dropped from $120 to $45.
Another woman discovered her memory issues were caused by an antihistamine she’d been taking for allergies for 10 years. The pharmacist switched her to a non-drowsy alternative. Her brain fog cleared.
These aren’t miracles. They’re outcomes of a simple, free service that most people ignore.
What’s New in 2025?
The rules keep improving. In 2024, CMS lowered the out-of-pocket cost threshold to $1,623, so more people qualify. Plans are also using electronic health records more - your pharmacist might see your doctor’s notes before your appointment.
A new pilot program is testing AI tools that help you prepare. You answer a few questions online, and it generates a pre-review checklist. Early results show a 22% drop in missed interactions. It’s not mandatory yet - but it’s coming.
Also, Medicare is pushing harder to reach rural seniors. In 2023, only 42% of rural beneficiaries had a CMR - compared to 61% in cities. That gap is shrinking.
Next Steps - What to Do Now
It’s November 2025. Your next CMR is likely due in the next few months.
- Call your Medicare Part D plan. Ask: “Am I eligible for a Comprehensive Medication Review this year?”
- If yes, schedule it now. Don’t wait for them to call.
- Start gathering your meds today. Take photos. Write down your questions.
- Ask a family member to join you.
- After the review, follow the action plan. Don’t ignore it.
This isn’t a box to check. It’s your best shot at staying healthy, safe, and in control of your medications - without unnecessary risks or costs.
Do I have to pay for a Medicare Annual Medication Review?
No. The Comprehensive Medication Review (CMR) is a free benefit included in your Medicare Part D plan. There is no copay, no fee, and no charge for the consultation, written summary, or follow-up. It’s part of your coverage.
Can I do the review over the phone or video call?
Yes. Medicare allows CMRs to be done in person, over the phone, or via video call (telehealth). Many people prefer video because they can show their medication bottles on screen. Just make sure you’re in a quiet place with good lighting so the pharmacist can see your labels clearly.
What if I don’t have all my medication bottles?
If you don’t have the bottles, bring a written list with the drug name, dose, frequency, and reason for taking it. But this is risky - pharmacists can’t verify accuracy without the original label. If possible, call your pharmacy and ask them to print a current medication list. Even better, take photos of your bottles before they’re empty.
Will the pharmacist change my prescriptions?
No. Pharmacists can’t change your prescriptions. But they can recommend changes to your doctor - like stopping a drug, lowering the dose, or switching to a cheaper alternative. They’ll send a note to your doctor with their suggestions. You’ll need to follow up with your doctor to approve any changes.
How often should I update my Personal Medication List?
Update it every time you start, stop, or change a medication - even if it’s just a new OTC pain reliever. Keep the list in your wallet, purse, or phone. Show it to every new doctor, ER staff, or pharmacist. It’s your most important health document.
What if I disagree with the pharmacist’s recommendations?
You have the right to disagree. Ask for the reasoning behind their suggestion. If you’re unsure, take the action plan to your primary care doctor for a second opinion. Never stop a medication without talking to your doctor first - even if the pharmacist says it’s safe.






Write a comment