Getting vaccinated while on immunosuppressants isn’t just about following a checklist-it’s about timing, type, and trust. If you’re taking steroids, rituximab, methotrexate, or any drug that dulls your immune system, the wrong vaccine at the wrong time can do more harm than good. The good news? There’s a clear, science-backed roadmap. The bad news? Many doctors still get it wrong. In 2025, the Infectious Diseases Society of America (IDSA) and the CDC updated their guidelines to reflect what actually works for people with weakened immune systems. This isn’t theoretical. It’s life-or-death advice based on real data from thousands of patients.
Live vs Inactivated: The Core Difference
Not all vaccines are created equal. The biggest split is between live attenuated vaccines and inactivated vaccines. Live vaccines use a weakened version of the actual virus-like the ones in MMR (measles, mumps, rubella), varicella (chickenpox), and the old nasal flu spray (LAIV). These work great in healthy people because they mimic a real infection and trigger a strong, lasting immune response. But for someone on immunosuppressants, even a weakened virus can replicate too much and cause disease. That’s why they’re outright banned for most immunocompromised patients. Inactivated vaccines, on the other hand, use killed viruses or just pieces of them-like the flu shot you get in the arm, the COVID-19 mRNA shots from Pfizer or Moderna, hepatitis B, and pneumococcal vaccines. These can’t cause infection. They’re safe. But they’re weaker. Your immune system doesn’t respond as strongly, so you often need extra doses or precise timing to get any protection at all.When to Get Vaccinated: Timing Is Everything
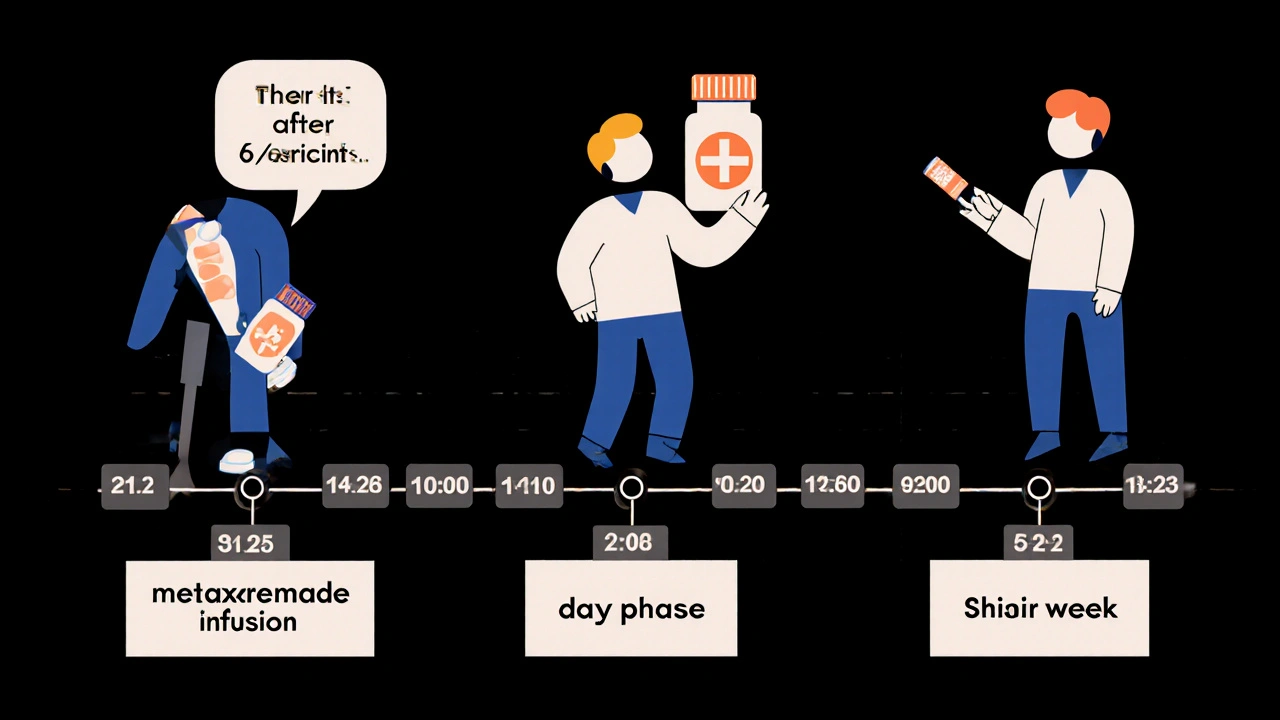
If you’re on immunosuppressants, getting a vaccine on the wrong day is like showing up to a battle unarmed. The IDSA 2025 guidelines say the best time to vaccinate is when your immune system is least suppressed. For most people, that means before starting treatment. If you’re planning a transplant or starting biologic therapy, get caught up on all needed vaccines at least 14 days before your first dose. But what if you’re already on treatment? Here’s where it gets specific:- If you’re on rituximab, ocrelizumab, or other B-cell depleting drugs: Wait at least 6 months after your last dose before getting any vaccine. The ideal window is 3-6 months after your last infusion. If you’re still getting regular infusions, schedule your vaccine 4 weeks before your next one.
- If you’re on cyclophosphamide: Vaccinate during the “nadir week”-the week when your white blood cell count is starting to recover after a cycle.
- If you’re on corticosteroids (like prednisone) at 20 mg or more daily for over two weeks: Hold off until your dose drops below 20 mg/day. Some patients skip their steroid dose for a week after vaccination to boost response-this should only be done under doctor supervision.
- If you’re on methotrexate: Some rheumatology clinics now recommend holding methotrexate for 1-2 weeks after each vaccine dose. One patient with rheumatoid arthritis reported developing detectable antibodies for the first time after doing this.
Which Vaccines Are Safe? The 2025 List
Here’s what’s recommended for immunocompromised adults and children in 2025:- Safe and recommended: Inactivated flu shot (not the nasal spray), all COVID-19 mRNA vaccines (Pfizer, Moderna), Novavax protein-based vaccine, hepatitis B (Engerix-B, Recombivax HB, or Heplisav-B), pneumococcal vaccines (PCV20 and PPSV23), Tdap, and inactivated polio.
- Avoid completely: MMR, varicella, zoster (Zostavax), live attenuated influenza vaccine (LAIV), and oral polio.
- Special cases: The new recombinant zoster vaccine (Shingrix) is safe and recommended for those on immunosuppressants-even if you’ve had shingles before. It’s not live, and it’s more effective than the old version.
Why Do Some Vaccines Fail? The Reality Check
It’s not just about safety-it’s about effectiveness. Studies show that while healthy people develop over 90% antibody protection after mRNA COVID-19 vaccines, immunocompromised patients range from 15% to 85%. That’s a huge gap. A patient on rituximab might have zero response. Someone on low-dose methotrexate might respond well. That’s why one-size-fits-all doesn’t work. A University of Washington study from 2023-2024 found that kidney transplant patients who got structured, scheduled vaccinations had 42% fewer breakthrough COVID-19 infections than those who got vaccines randomly. The key? Coordination. When your oncologist, rheumatologist, and pharmacist are all on the same page, your protection improves dramatically.What About Your Family?
Your vaccine isn’t the only one that matters. The IDSA guidelines strongly recommend that everyone in your household gets fully vaccinated too. This is called “cocooning.” If your partner, kids, or roommate are up to date on flu and COVID shots, they’re less likely to bring the virus home to you. The Payne 2025 study showed this strategy cut household transmission by 57%. Don’t assume your family’s vaccines protect you. They reduce risk-but they don’t eliminate it. That’s why you still need your own shots, timed right.What If You Got the Wrong Vaccine?
It happens. A Reddit user shared how their oncologist scheduled them for the nasal flu vaccine while they were on rituximab. They only caught it because their infectious disease specialist intervened. Another patient on Inspire.com said their pharmacy kept running out of the updated COVID vaccine, delaying their booster during a winter surge. If you think you got a live vaccine by mistake, contact your doctor immediately. For MMR or varicella, they may need to monitor you for fever, rash, or other signs of infection. For inactivated vaccines that were given too early or too late, you may just need to repeat the dose when timing is better.
Tools and Resources That Actually Help
You don’t have to figure this out alone. In November 2025, the IDSA launched a free online decision tool that generates a personalized vaccination schedule based on your exact medications. Just enter your drugs, doses, and treatment dates, and it tells you when to vaccinate and which ones to get. The CDC also runs a 24/7 clinical consultation line for providers. In the first quarter of 2025, they handled over 1,200 calls from doctors unsure about vaccinating immunocompromised patients. If your doctor is unsure, ask them to call it. Epic’s electronic health records system now auto-alerts providers when a patient on immunosuppressants is due for a vaccine. That means fewer missed opportunities.The Bigger Picture: What’s Coming Next
The field is moving fast. By 2026, researchers expect to identify immune markers that predict who will respond to a vaccine-and who won’t. That could lead to blood tests that tell you if you need another dose before you even get sick. The NIH is already testing new adjuvanted vaccines-formulations with stronger immune boosters-designed specifically for people with suppressed immune systems. These could be game-changers. For now, stick to the proven plan: avoid live vaccines, get inactivated ones at the right time, coordinate with your care team, and make sure your household is protected too. It’s not glamorous. But it’s the difference between getting through winter without a hospital stay-and not.Can I get the flu shot if I’m on prednisone?
Yes, but timing matters. If you’re taking 20 mg or more of prednisone daily for two weeks or longer, wait until your dose drops below 20 mg/day. If you can’t reduce it, get the inactivated flu shot anyway-it’s still safer than risking the flu. Avoid the nasal spray version completely.
I’m on rituximab. When should I get my COVID booster?
Wait at least 6 months after your last rituximab infusion. The best window is 3-6 months post-treatment. If you’re still getting regular infusions, schedule your booster 4 weeks before your next one. Don’t wait for symptoms to appear-get it done before your next cycle.
Are mRNA vaccines safe for transplant patients?
Yes. mRNA vaccines (Pfizer and Moderna) are the safest and most effective option for transplant recipients. They’re not live and don’t contain the virus. Most transplant centers now recommend two doses of the 2025-2026 updated vaccine, and sometimes a third if your immune response is low.
Can I get Shingrix if I’m on immunosuppressants?
Yes. Shingrix is not a live vaccine-it’s recombinant and safe for immunocompromised patients. It’s even more effective than the old zoster vaccine and recommended for anyone over 50 on immunosuppressants, even if you’ve had shingles before.
Do I need to stop my methotrexate for the vaccine?
Some rheumatologists recommend holding methotrexate for 1-2 weeks after each vaccine dose to improve response. This isn’t for everyone-talk to your doctor. Some patients report better antibody levels after doing this, but it’s not required if your condition is unstable.
What if my pharmacy doesn’t have the right vaccine?
Call ahead. Many community pharmacies don’t stock the updated 2025-2026 COVID vaccines for immunocompromised patients. Ask your doctor’s office for a prescription and a list of nearby clinics or hospitals that carry it. Specialized networks like IVAN (Immunocompromised Vaccine Access Network) coordinate directly with oncology centers and often have the right doses on hand.






Write a comment