Protein-Medication Timing Calculator
This tool helps you determine the best time to take protein-sensitive medications based on your protein intake. Follow evidence-based timing to maximize medication effectiveness.
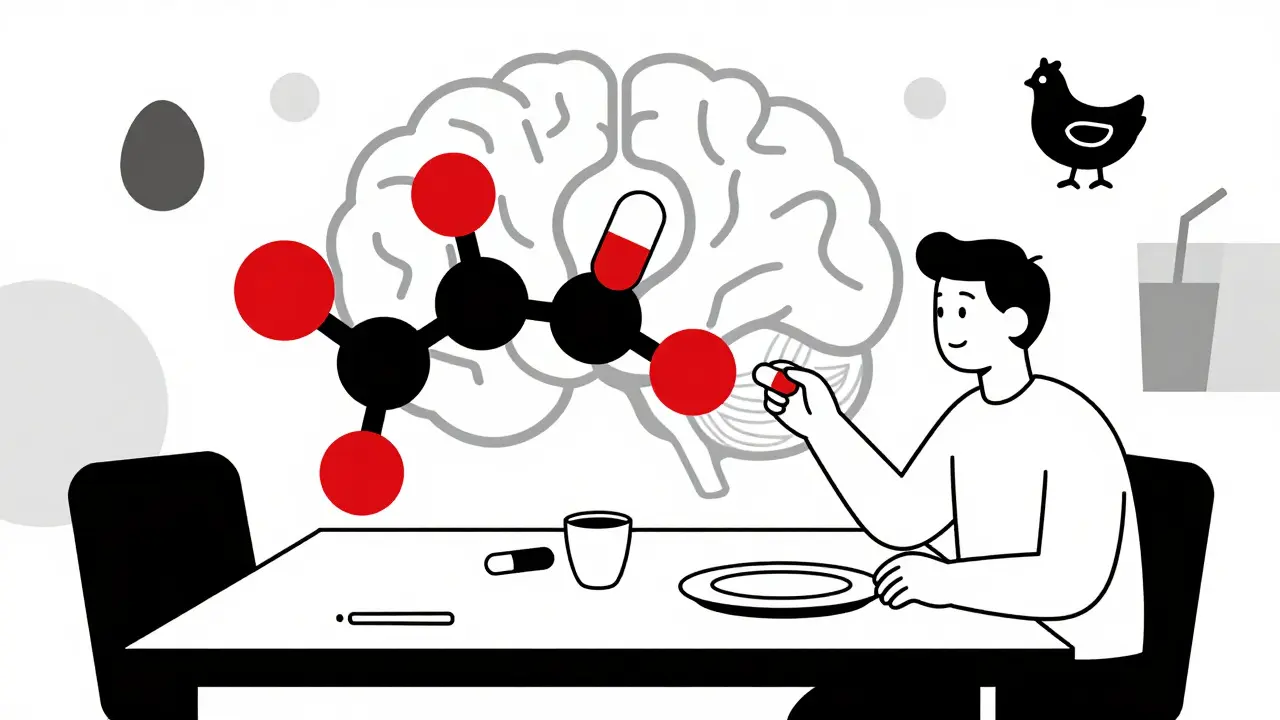
Many people don’t realize that what they eat for breakfast could be making their medication less effective. If you’re taking levodopa for Parkinson’s disease, or even certain antibiotics, the protein in your eggs, chicken, or protein shake might be blocking your body from absorbing it properly. This isn’t a myth or a vague warning-it’s a well-documented, clinically proven interaction that affects thousands of people every day.
Why Protein Interferes With Medication
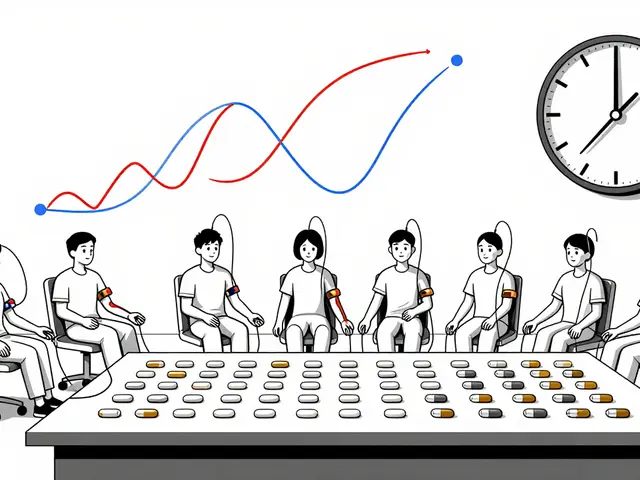
Protein-rich foods break down into amino acids during digestion. These amino acids use the same transporters in your gut and blood-brain barrier as some medications, especially levodopa and certain antiepileptic drugs. Think of it like a crowded elevator: if too many amino acids are trying to get through at once, the medication gets left behind. Research from the 2022 NIH study (PMC8747252) shows that after eating a high-protein meal, amino acid levels in your blood spike by 200-300% within 30 minutes. That surge overwhelms the large neutral amino acid transporters (LNAATs), which are also the main route for levodopa to enter the brain. As a result, up to 50% less medication reaches its target. This isn’t just theory-it’s measurable. Clinical trials show that a 50g protein meal (about the amount in a large chicken breast) can reduce levodopa bioavailability by 25% or more. The effect isn’t the same for all drugs. The Biopharmaceutics Classification System (BCS) helps explain why. Drugs like levodopa are BCS Class III: highly soluble but poorly permeable. That means they rely heavily on those specific transporters. Meanwhile, BCS Class I drugs-like some statins or painkillers-don’t care as much about protein because they slip through cell membranes easily. So if your medication is for Parkinson’s, epilepsy, or certain infections, protein timing matters. If it’s for cholesterol or headaches, it likely doesn’t.Levodopa: The Most Studied Example
Levodopa is the poster child for protein-medication conflicts. It’s the gold-standard treatment for Parkinson’s, but its absorption is notoriously sensitive to dietary protein. The Michael J. Fox Foundation’s 2022 clinical trials found that patients who took levodopa with meals saw a 30-50% drop in drug levels. That translates to more ‘off’ time-when symptoms return because the medication isn’t working. But here’s the good news: you don’t have to stop eating protein. You just need to rethink when you eat it. The protein-redistribution diet has become a game-changer. Instead of spreading protein evenly across meals, you consume 70% of your daily protein at dinner. That leaves breakfast and lunch low in protein, giving levodopa a clear path to absorption during the day when you need it most. One patient, tracked with a wearable sensor, reported cutting their daily ‘off’ time from 5.2 hours to just 2.1 hours after switching to this approach. That’s not luck-it’s science. A 2024 review in the Journal of Parkinson’s Disease confirmed that this strategy improves motor control without risking malnutrition, as long as total daily protein stays within recommended limits (0.8-1.0g per kg of body weight).Other Medications That Play Nice (or Not) With Protein
Levodopa isn’t the only one. Antibiotics like penicillins and cephalosporins can also see reduced absorption when taken with protein-rich meals. Studies show a 15-20% drop in peak concentration, which might seem small-but in infections, that’s the difference between clearing the bug and letting it hang on. On the flip side, some drugs actually absorb better with protein. Certain antibiotics, like tetracyclines, benefit from the increased blood flow to the gut that protein triggers. Pancreatic enzymes and some antivirals also see improved uptake when taken with food. But here’s the catch: the benefit isn’t from protein itself-it’s from the overall meal. That’s why general advice like “take with food” can be misleading. You need to know what kind of food. The FDA’s 2019 guidance now requires all new drugs to be tested with both low-fat and high-fat meals. But protein-specific testing? That’s still inconsistent. A 2024 European Medicines Agency review found that 61% of drug labels don’t mention protein interactions-even when they’re proven. If your prescription doesn’t say anything about food, ask your pharmacist. Don’t assume it’s safe.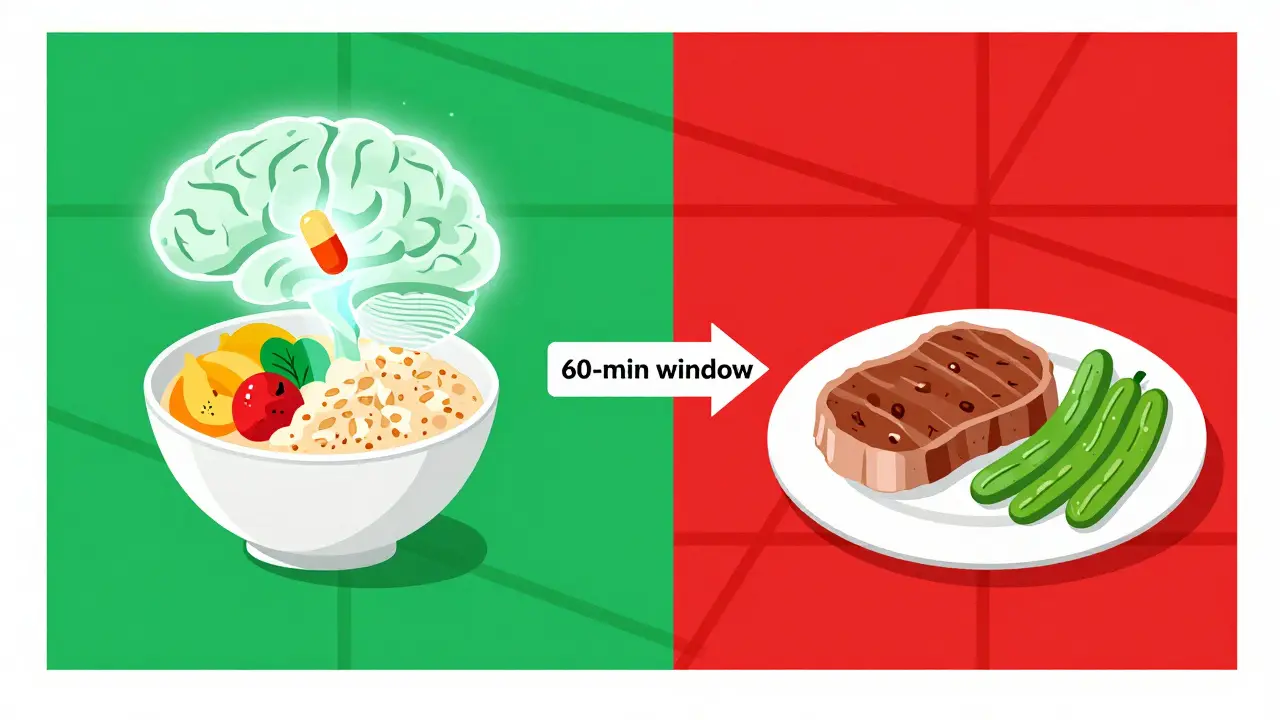
What Happens When You Ignore Protein Timing
Ignoring protein-medication interactions doesn’t just mean your meds don’t work as well. It leads to real, measurable consequences. Patients with Parkinson’s who don’t time their medication properly report more falls, longer ‘off’ periods, and increased hospital visits. A 2023 report from the University of Rochester found that protein-related absorption issues account for 12-15% of therapeutic failures in Parkinson’s management. That’s not rare-it’s common. And here’s a hidden risk: some people try to fix the problem by going on low-protein diets. Sounds logical, right? But the Journal of Parkinson’s Disease found that 23% of patients on strict low-protein diets developed muscle wasting within 18 months. Your body needs protein to maintain muscle, immune function, and organ health. Cutting it too low is just as dangerous as eating too much at the wrong time.How to Get It Right: Practical Steps
You don’t need to become a nutritionist. But you do need a simple plan.- Take levodopa 30-60 minutes before meals that contain more than 15g of protein. That’s about the amount in one egg, 2 tablespoons of peanut butter, or a small yogurt.
- Choose low-protein snacks if you get nauseous. Oatmeal (1g protein per serving), fruit, or rice cakes are safe options.
- Shift your protein to dinner. Have eggs for breakfast? Skip them. Swap chicken for tofu or beans at lunch. Save the steak, salmon, or whey shake for the evening.
- Read labels. Many ‘healthy’ foods hide protein. A granola bar can have 7g. A protein-fortified smoothie? 20g. That’s enough to ruin your morning dose.
- Use a tracker. Apps like ProteinTracker for PD (developed by Johns Hopkins) let you log meals and meds. Users report 40% fewer timing errors after just two weeks.