Not All Rashes Are Allergies
You give your child amoxicillin for an ear infection. Three days later, a red, spotty rash appears on their chest and arms. Your heart drops. Antibiotic rash-you’ve heard the warnings. You panic and stop the medicine right away. But here’s the truth: in most cases, you shouldn’t have.
Up to 10% of kids on amoxicillin get a rash. Yet less than 1% are truly allergic. The rest? Non-allergic reactions, often tied to a virus they already had. The rash isn’t a sign the drug is dangerous-it’s just the body’s odd response to the combo of infection and medication. Stopping the antibiotic unnecessarily doesn’t protect them. It hurts them.
What Does a Real Allergic Reaction Look Like?
True allergic reactions to antibiotics happen fast. Think minutes to an hour after taking the dose. The rash looks like raised, red, itchy welts-hives. They move around. One spot fades, another pops up. You might also see swelling of the lips, tongue, or eyelids. Trouble breathing? Wheezing? Dizziness? Vomiting? That’s anaphylaxis. It’s rare, but it’s life-threatening.
If you see any of these signs, stop the antibiotic immediately. Call emergency services or go to the nearest ER. Use an epinephrine auto-injector if one is available. This isn’t something to wait out. Anaphylaxis can worsen in minutes.
The Most Common Rash: Not an Allergy at All
Most antibiotic rashes aren’t allergic. They’re delayed. They show up between day 5 and day 10 of treatment. They’re flat, red spots-like a sunburn with dots. They usually start on the trunk, spread to the limbs, and don’t itch much, if at all. They don’t move. They don’t swell. They just sit there.
This kind of rash is especially common in kids with mononucleosis or other viral infections. The body’s immune system is already stirred up. The antibiotic adds fuel. The result? A harmless, ugly rash that looks scary but isn’t dangerous.
Studies show that 92% of pediatricians who see this rash keep the antibiotic going. Why? Because stopping it increases the chance of the infection coming back worse. And when you switch to a different antibiotic, you’re more likely to get diarrhea, C. diff, or even a resistant infection. The CDC reports that patients mislabeled as penicillin-allergic have a 63% higher risk of antibiotic-associated diarrhea.
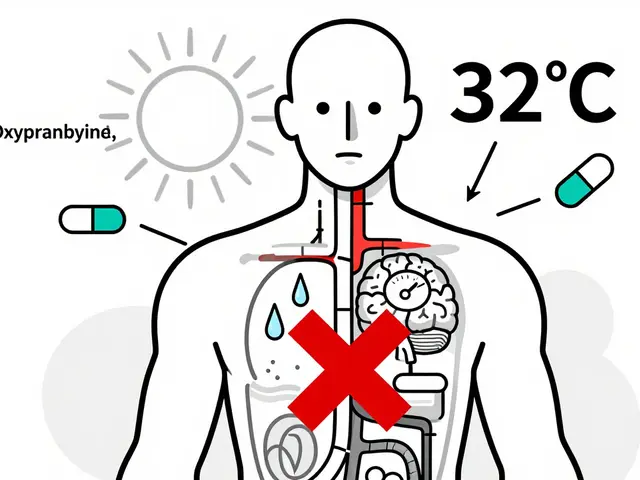
When to Stop the Antibiotic-For Real
You don’t stop every rash. But there are red flags that mean you must stop immediately and get help:
- Blistering skin or peeling (like a bad sunburn)
- Rash in the mouth, eyes, or genitals
- Fever over 38.5°C (101.3°F)
- Swollen lymph nodes
- Joint pain or swelling
- Dark urine, yellow skin, or extreme fatigue
These signs point to severe reactions like Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN), or DRESS syndrome. These are medical emergencies. Mortality rates for TEN can hit 50%. Don’t wait. Go to the ER. Don’t call your doctor’s office-go.

What to Do If It’s Just a Non-Allergic Rash
If the rash is flat, not itchy, and your child feels fine otherwise-keep giving the antibiotic. Finish the full course. That’s the rule.
If there’s mild itching, you can try:
- Cetirizine (Zyrtec) or loratadine (Claritin) for kids over 2
- Topical hydrocortisone 1% cream on the worst spots
- Calamine lotion to soothe the skin
Don’t use oral steroids unless a doctor says so. Studies show they don’t speed up healing and can increase complications.
The rash will fade on its own in 5 to 10 days. You might see it darken a bit-like a bruise-as it heals. That’s normal.
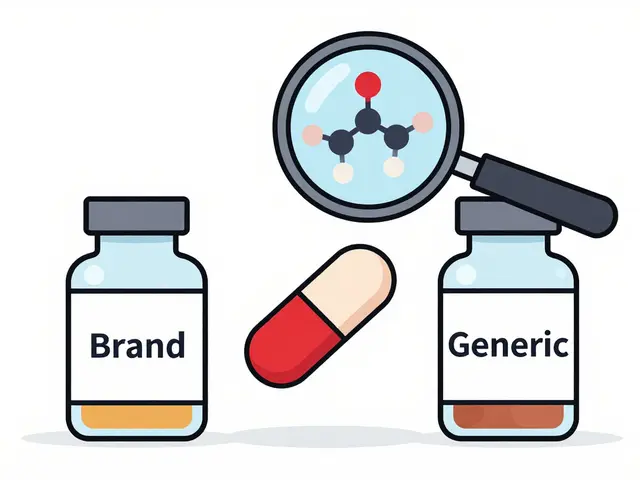
Don’t Label Your Child as Allergic
Too many parents write down “penicillin allergy” on their child’s medical forms after a rash. That label sticks. It follows them into adulthood. And it’s often wrong.
Research from Cincinnati Children’s Hospital shows that 90% of kids labeled allergic to amoxicillin because of a rash turn out not to be allergic when properly tested. That means they’re being denied the safest, most effective antibiotic for infections like strep throat, ear infections, and pneumonia.
Instead of writing “allergic,” write: “Rash during amoxicillin treatment, day 7, non-itchy, resolved without intervention.” That’s accurate. That’s helpful.
What Happens When You Stop the Antibiotic Too Soon
Stopping antibiotics for a non-allergic rash doesn’t make your child safer. It makes them sicker.
One parent on Reddit shared: “Stopped amoxicillin after a rash. Infection came back worse. Had to use clindamycin. Diarrhea lasted two weeks.” That’s not rare. In fact, 37% more treatment failures happen when antibiotics are stopped for rashes that aren’t allergic.
Doctors end up prescribing broader-spectrum drugs like clindamycin, azithromycin, or fluoroquinolones. These are more expensive. They’re harder on the gut. And they fuel antibiotic resistance.
The CDC estimates that mislabeling penicillin allergies costs the U.S. healthcare system $1.2 billion a year. That’s billions spent on drugs that aren’t needed, longer hospital stays, and preventable infections.
What’s New in Testing and Diagnosis
There’s good news: testing for true penicillin allergy is easier now than ever.
A new rapid test called PENtest gives results in 15 minutes-no 3-hour clinic visits needed. It’s being rolled out in hospitals and allergist offices across the U.S. and Australia. If you or your child had a rash years ago and you’re unsure if it was an allergy, ask your doctor about testing.
AI tools are also emerging. A smartphone app currently in trials can analyze photos of rashes and distinguish allergic from non-allergic with 89% accuracy. It’s not a replacement for a doctor, but it’s a powerful tool for parents who are unsure.
Bottom Line: Don’t Guess. Assess.
Here’s your simple checklist when a rash appears on antibiotics:
- Timing: Did it show up in the first 24-72 hours? If yes, watch for hives or swelling.
- Appearance: Raised and itchy? That’s hives. Flat and non-itchy? Likely harmless.
- Symptoms: Fever? Blisters? Swollen throat? Go to the ER.
- Feelings: Is your child acting normal? Eating? Playing? Then it’s probably not dangerous.
If you’re unsure, call your doctor. But don’t stop the antibiotic unless you’re certain it’s an allergic reaction or a severe rash.
Finishing the antibiotic protects your child from a worse infection. And it protects the rest of us from more drug-resistant bacteria.
When to Call the Doctor
You don’t need to rush to the ER for every rash. But call your doctor if:
- The rash spreads quickly or looks worse after 48 hours
- Your child develops a fever or seems unusually tired
- You’re unsure whether it’s hives or a flat rash
- You want to know if testing for penicillin allergy is right for your child
Bring a photo of the rash. Note the day of treatment when it started. That helps your doctor make a faster, smarter call.
Final Thought: Trust the Science, Not the Fear
Antibiotic rashes scare parents. And rightly so-they look bad. But fear shouldn’t override facts. Most rashes aren’t allergies. Most rashes don’t need stopping. Most rashes fade on their own.
By continuing the antibiotic when appropriate, you’re not risking your child’s safety. You’re protecting it. And you’re helping fight the bigger threat: antibiotic resistance.


Write a comment