Every year, 125,000 preventable deaths in the U.S. happen because people don't take their medications correctly. But involving family or caregivers in medication support can cut those numbers significantly. This isn't just about helping someone take pills-it's about building a system that keeps them safe and healthy.
Caregiver Medication Management is the process of engaging family members or professional caregivers to help manage medications. This approach has become essential as more people take multiple medications, especially older adults. According to the Caregiver Action Network's 2023 guide, 48 million family caregivers in the U.S. handle some aspect of medication management, with 83% responsible for it. The stakes are high: medication non-adherence costs $300 billion annually in healthcare expenses and contributes to 125,000 preventable deaths each year.
Think about your own experience. If you've ever forgotten to take a pill, you know how easy it is to slip up. Now imagine someone with memory issues or complex health conditions. Without help, they're at serious risk. But caregivers who step in can make all the difference.
Why Caregiver Involvement Matters
When someone takes multiple medications, the risk of errors skyrockets. The Institute for Safe Medication Practices reports that 50% of medication errors happen in home settings. But caregivers who actively participate reduce these errors dramatically. For example, a 2023 study in the Journal of Palliative Medicine found that caregivers using a master medication list reduced errors by 33%.
Real-life proof comes from caregivers like "Mary from Ohio" who shared on the Caregiver Action Network forum: "Tracking everything in my binder helped me catch a dangerous interaction between my mother's new blood pressure med and her arthritis drug before it caused problems." This isn't rare-78% of caregivers who use organized tracking systems report fewer medication errors.
Creating a Master Medication List
Your first step should be a complete medication list. The Agency for Healthcare Research and Quality (AHRQ) says this list must include 17 specific details per medication: brand and generic names, exact dosage (like "Lisinopril 10mg"), timing instructions (e.g., "Take with breakfast"), prescribing doctor, purpose, and potential side effects or interactions. Update this list within 24 hours of any change.
During hospital-to-home transitions, where 50-60% of medication errors happen, this list is your lifeline. Reddit user "JohnDoe_Caregiver" explained how bringing a master list to appointments solved a major issue: "When my dad saw 4 different specialists, nobody knew what the others prescribed until I created a master list and brought it to every appointment."
Setting Up Reliable Routines and Reminders
How do you make sure meds are taken on time? Simple routines work best. The National Institute on Aging recommends "habit stacking"-linking medication times to existing habits. For example, "take blood pressure pills right after brushing teeth in the morning." This technique increases adherence by 28% according to a 2022 study.
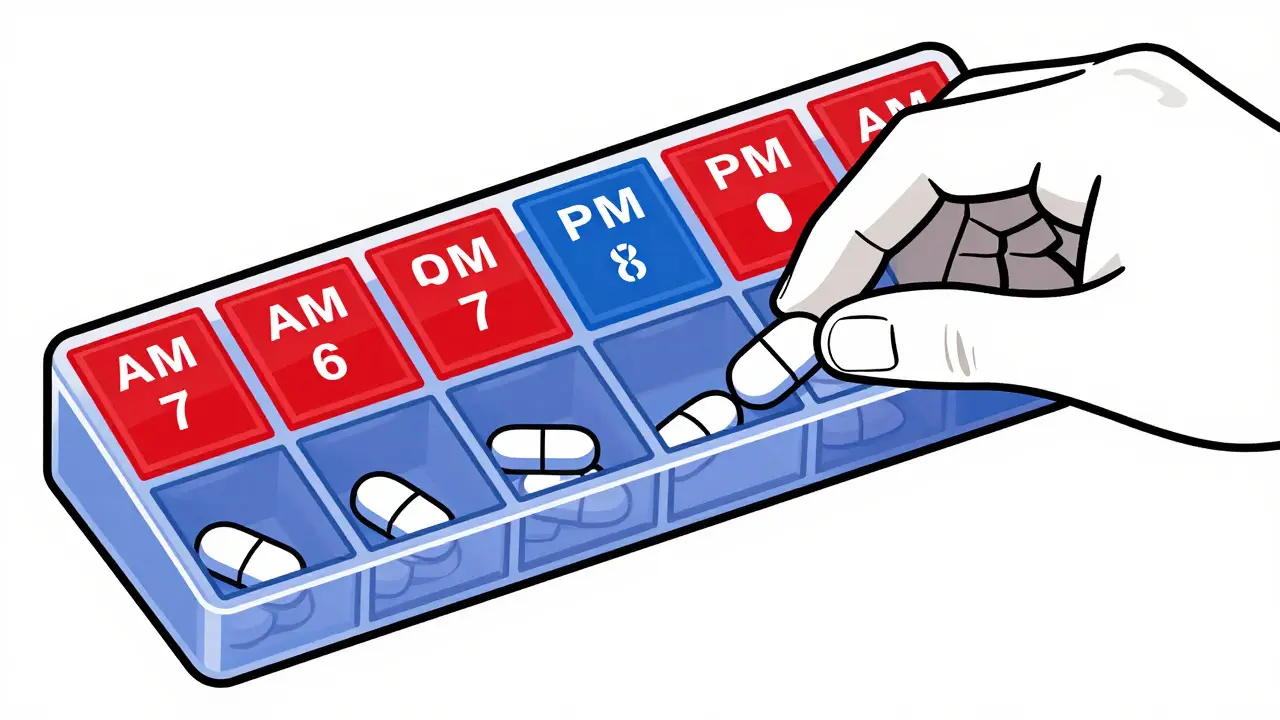
Pill organizers are simple tools that organize medications by day and time. A 2022 study in the Journal of the American Geriatrics Society found they reduce errors by 37% when used correctly. These come in 7-day AM/PM formats or electronic versions with alarms.
For tech-savvy caregivers, apps like Medisafe send push notifications and track doses. Research shows these apps improve adherence by 45% compared to paper logs. Voice-activated reminders through Amazon Alexa Care Hub reduce missed doses by 37% for people with cognitive issues, per a 2023 University of Pittsburgh study.
Conducting Regular Medication Reviews
Medications change over time. Regular reviews prevent dangerous combinations. The American Geriatrics Society's Beers Criteria lists 30 medication classes that pose special risks for older adults. Always check new prescriptions against this list during doctor visits.
Medication Therapy Management (MTM) services are available through Medicare Part D and private insurance. These free pharmacist consultations review all medications for safety and effectiveness. As of January 2024, 85% of major pharmacies offer automatic refill programs that prevent gaps in coverage.

Emergency Protocols for Critical Medications
Some medications require immediate action if missed. Create a "medication red list" for drugs like insulin, blood thinners, or seizure medications. Keep this list visible and share it with all caregivers.
A 2023 Annals of Internal Medicine study found that having a clear red list decreases emergency department visits by 19%. For example, if someone misses a dose of warfarin (a blood thinner), they should know to contact their doctor immediately. Write down exactly what to do for each red-listed drug. Keep this information in your medication binder or app.
Navigating Common Challenges
Transitioning from hospital to home is a high-risk period. A 2022 University of Michigan study found 68% of caregivers feel confused during this phase. Bring your master medication list to every appointment and ask doctors to confirm all changes.
Multiple prescribers can lead to duplicate medications. As Reddit user "JohnDoe_Caregiver" shared, bringing a master list to each specialist appointment prevented dangerous overlaps: "Nobody knew what the others prescribed until I created a master list and brought it to every appointment."
When overwhelmed, use pharmacy resources. Pharmacists are medication experts-92% of U.S. pharmacies have pharmacists available for consultations without appointments. Ask the four critical questions: What time should this be taken relative to meals? Are there specific food or medication interactions? What should I do if a dose is missed? When should I expect to see effects?
What's the most important thing caregivers should do for medication support?
Creating and maintaining a complete master medication list is the foundation. This list should include all medications (brand and generic names), exact dosages, timing instructions, prescribing doctors, and potential side effects. The Agency for Healthcare Research and Quality (AHRQ) states that caregivers with a full 17-element list reduce adverse drug events by 41% compared to those with incomplete lists.
How often should medication lists be updated?
Update the list within 24 hours of any medication change. This includes new prescriptions, dosage adjustments, or discontinuations. During hospital discharges, which are high-risk periods, verify the list with the discharge team before leaving the hospital. The Agency for Healthcare Research and Quality recommends this timing to prevent dangerous errors during care transitions.
What should I do if a dose is missed?
Never double up on doses unless instructed. For most medications, skip the missed dose and take the next one at the regular time. However, for critical drugs like insulin or blood thinners, contact the prescribing doctor immediately. The American Pharmacists Association recommends always asking pharmacists about missed dose protocols during medication consultations.
Are there free resources to help caregivers manage medications?
Yes. Medicare Part D offers free Medication Therapy Management (MTM) services for eligible beneficiaries taking multiple medications. Most major pharmacies like CVS and Walgreens provide free pharmacist consultations without appointments. The Caregiver Action Network also offers a free "Caregiver's Notebook" template for organizing medication details. These resources are available to all caregivers regardless of insurance status.
How can caregivers avoid dangerous drug interactions?
Always review all medications with a pharmacist before starting a new prescription. Use the Beers Criteria checklist for older adults to spot high-risk combinations. Keep a complete master medication list and share it with all healthcare providers. The American Geriatrics Society reports that regular pharmacist consultations reduce drug interactions by 29% in seniors taking multiple medications.







Write a comment