Lipid-Based Medication Fat Calculator
Medication Selection
Select your medication to determine the recommended dietary fat amount for optimal absorption.
Important: This calculator shows general recommendations based on medical guidelines. Always follow your prescription instructions and consult your doctor or pharmacist for personalized advice.
When you take a pill with a fatty meal, you might think it’s just about avoiding an upset stomach. But for some medications, that bite of avocado, cheese, or fried chicken isn’t optional-it’s part of the treatment. Lipid-based medications rely on dietary fat to work properly. Without it, they might not get absorbed at all. This isn’t a myth or old wives’ tale. It’s science backed by decades of research and FDA-approved formulations.
Why Fat Matters for Certain Drugs
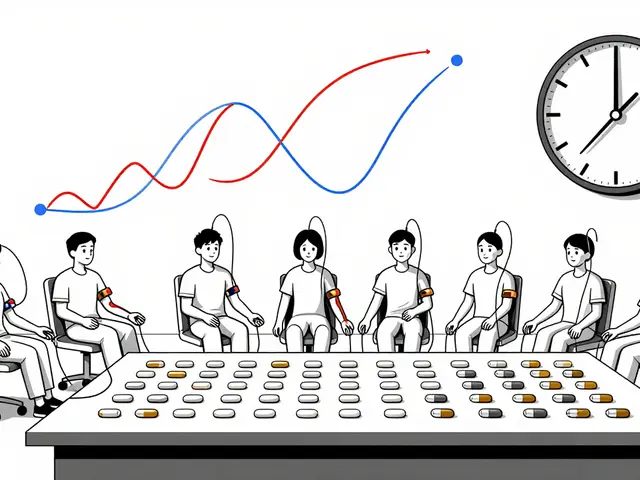
About 70% of new drugs being developed today don’t dissolve well in water. These are called poorly water-soluble drugs. They’re often lifesavers-used for cancer, HIV, high cholesterol, and autoimmune diseases-but if they can’t dissolve, your body can’t absorb them. That’s where fat comes in. When you eat fatty foods, your body releases bile and enzymes that break down lipids into tiny structures called micelles. These micelles act like molecular taxis, picking up drug molecules and carrying them through the gut lining into your bloodstream.Drugs like cyclosporine (used after organ transplants), fenofibrate (for cholesterol), and itraconazole (an antifungal) all depend on this process. Studies show that taking these drugs with a high-fat meal can increase absorption by 20% to over 300%. For example, the lipid-based version of cyclosporine, Neoral®, delivers 20-30% more of the drug into the blood than older versions taken on an empty stomach. That means better results, fewer side effects, and sometimes even lower doses.
How Lipid-Based Formulations Work
Pharmaceutical companies didn’t just wait for people to eat fatty meals-they built the solution into the medicine. Lipid-based drug delivery systems are specially designed to mimic what happens when you eat fat. These formulations contain oils, surfactants, and co-solvents that turn into micelles as soon as they hit your digestive tract.One of the most common types is called SEDDS-Self-Emulsifying Drug Delivery Systems. These are liquids packed into soft gel capsules. When swallowed, they mix with stomach fluids and form tiny droplets (100-300 nanometers wide) that keep the drug dissolved. Unlike regular pills that need to dissolve first, SEDDS start working immediately. This is why drugs like Sporanox® oral solution (itraconazole) work better than the capsule form-even on an empty stomach. The formulation does the work your body would normally do after a fatty meal.
Medium-chain triglycerides (MCTs), like those found in coconut oil, are preferred in these systems because they digest faster than long-chain fats. MCTs break down in 15-30 minutes, while long-chain fats take over an hour. Faster digestion means quicker drug release and more consistent absorption.
The Food Effect: More Than Just a Tip
In pharmacology, the "food effect" isn’t a suggestion-it’s a measurable, documented phenomenon. The FDA requires drug makers to test how meals impact absorption before approval. For many lipid-based drugs, the difference between taking them with or without food isn’t minor-it’s the difference between a drug working and failing.Take fenofibrate. The original version, Lopid®, had to be taken three times a day with meals. The lipid-based version, Tricor®, works once daily because it doesn’t rely on unpredictable food timing. A 2022 study found 87% of patients reported fewer stomach issues and 72% preferred the new formulation. That’s not just convenience-it’s improved quality of life.
But it’s not always that simple. Some drugs, like bisphosphonates used for osteoporosis, need an empty stomach and plain water. Fat interferes with their absorption. That’s why you can’t take alendronate with coffee, juice, or breakfast. It’s not a coincidence-these rules are based on hard data.
Who Benefits Most?
Patients with chronic conditions that require long-term medication are the biggest winners. People on immunosuppressants after transplants, those managing HIV with antivirals, or individuals with severe high cholesterol often depend on lipid-based drugs. For them, consistent absorption means fewer hospital visits, lower risk of rejection, and better control of disease.But there’s a catch: not everyone digests fat the same way. People with Crohn’s disease, cystic fibrosis, or gallbladder removal may not produce enough bile. Their bodies can’t form the micelles needed to carry the drug. That’s why some patients on lipid-based meds still have unpredictable results. Experts warn that these formulations aren’t magic-they still need a functioning digestive system to work properly.
Cost and Accessibility
Lipid-based drugs are expensive. A 30-day supply of Sporanox® oral solution can cost $1,200. The generic capsule version? Around $300. That’s a 4x difference. Insurance doesn’t always cover the branded version unless the generic fails. Many patients on Reddit’s r/pharmacy forum share stories of switching to the lipid version only to be shocked by the price tag.Manufacturing these drugs is also more complex. They require special capsules, precise mixing, and stability testing under different temperatures. Production costs are 25-35% higher than regular tablets. That’s why many older drugs still come in simple pills-because the cost-benefit doesn’t always justify the upgrade.
What’s Next?
The future of lipid-based delivery is getting smarter. Researchers at MIT developed a "smart lipid capsule" that changes how it releases the drug based on real-time pH and enzyme levels in the gut. It’s still experimental, but early results show it could eliminate food dependency entirely.Another breakthrough came in 2023 with Vybar®, a new lipid-based fenofibric acid formulation that boosts absorption by 45% and shows no food effect at all. That means patients can take it anytime-no meals required. This is the next step: making lipid-based drugs reliable even without dietary help.
Companies are also moving away from fish oil-based lipids toward plant-derived alternatives to reduce environmental impact. The European Federation for Pharmaceutical Sciences has pushed for greener options, and several new formulations now use sunflower or palm kernel oils instead.
What You Should Do
If you’re on a medication that might be affected by food, check the label. Look for phrases like:- "Take with food"
- "Best absorbed with a high-fat meal"
- "Avoid grapefruit juice"
- "May be taken without regard to meals"
Don’t guess. If the label doesn’t say, ask your pharmacist. A simple question could mean the difference between your drug working or not.
And if you’re prescribed a lipid-based version, don’t skip the fat. A handful of nuts, a spoonful of olive oil on your salad, or a small serving of cheese can make a real difference. You’re not just eating-you’re activating your medicine.
When Lipid-Based Drugs Don’t Work
Even the best formulations have limits. If your drug has solubility below 1 microgram per milliliter, even fat won’t help much. Some drugs are too stubborn to dissolve, no matter how many micelles are around. In those cases, scientists are turning to nanoparticles or crystalline modifications-but those are still in development.Also, if you’re on a low-fat diet for medical reasons (like pancreatitis or certain liver conditions), talk to your doctor. You might need a different formulation or a dose adjustment. Never assume a drug will work the same way without fat.
And remember: not all fats are equal. Trans fats and heavily processed oils don’t trigger the same digestive response as natural fats like avocado, olive oil, or fatty fish. Stick to whole-food sources when possible.
Do all medications need fatty foods to work?
No. Only poorly water-soluble drugs-mostly those classified as BCS Class II or IV-benefit from fat. Most common medications like antibiotics, pain relievers, or blood pressure pills work fine without food. Always check the label or ask your pharmacist.
Can I use any type of fat with lipid-based medications?
Not all fats are equally effective. Medium-chain triglycerides (MCTs) from coconut oil or MCT oil are ideal because they digest quickly. Long-chain fats like butter or fried foods work too, but slower. Avoid trans fats and highly processed oils-they don’t trigger the same digestive response. Natural sources like avocado, nuts, olive oil, or fatty fish are best.
Why do some lipid-based drugs say "take without food"?
Some drugs need an acidic environment to dissolve, like bisphosphonates for osteoporosis. Fat neutralizes stomach acid and slows digestion, which can block absorption. Other drugs are designed to be absorbed in the upper intestine, and food delays gastric emptying too much. Always follow the specific instructions on your prescription.
Are lipid-based medications safer than regular ones?
They can be. Because they improve absorption, lower doses are often needed, which reduces side effects. For example, patients on Tricor® report fewer stomach issues than those on older versions. But they’re not inherently safer-they just work differently. All medications carry risks, and lipid-based ones can be more expensive or harder to access.
Can I take lipid-based meds with a protein shake or smoothie?
It depends. If the shake contains fat-like peanut butter, avocado, or full-fat yogurt-then yes. But a protein shake made with water and whey powder won’t help. The key is fat content, not protein or calories. Aim for at least 10-15 grams of fat with your dose to trigger the necessary digestive response.
Is there a test to know if my body absorbs lipid-based drugs properly?
There’s no routine test for most patients, but doctors can measure blood levels of the drug to see if absorption is adequate. This is common for drugs like cyclosporine, where even small changes in absorption can affect organ rejection risk. If you’re not responding as expected, ask your doctor about therapeutic drug monitoring.






Write a comment