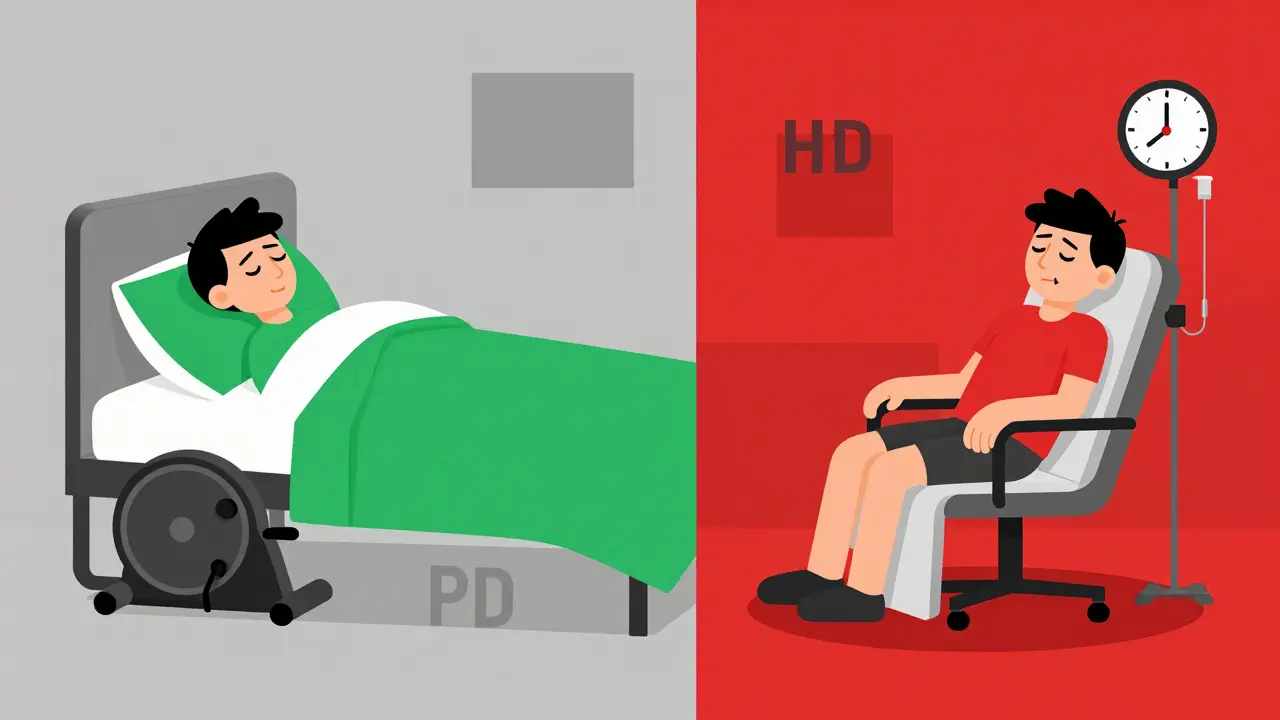
When your kidneys fail, life doesn’t stop-but how you manage it changes completely. Two main treatments keep people alive: hemodialysis and peritoneal dialysis. Both remove waste and extra fluid from your blood, but they do it in completely different ways. One happens in a clinic, three times a week. The other happens in your living room, every day. Choosing between them isn’t just about medical facts-it’s about your lifestyle, your body, and what you can handle day after day.
How Hemodialysis Works
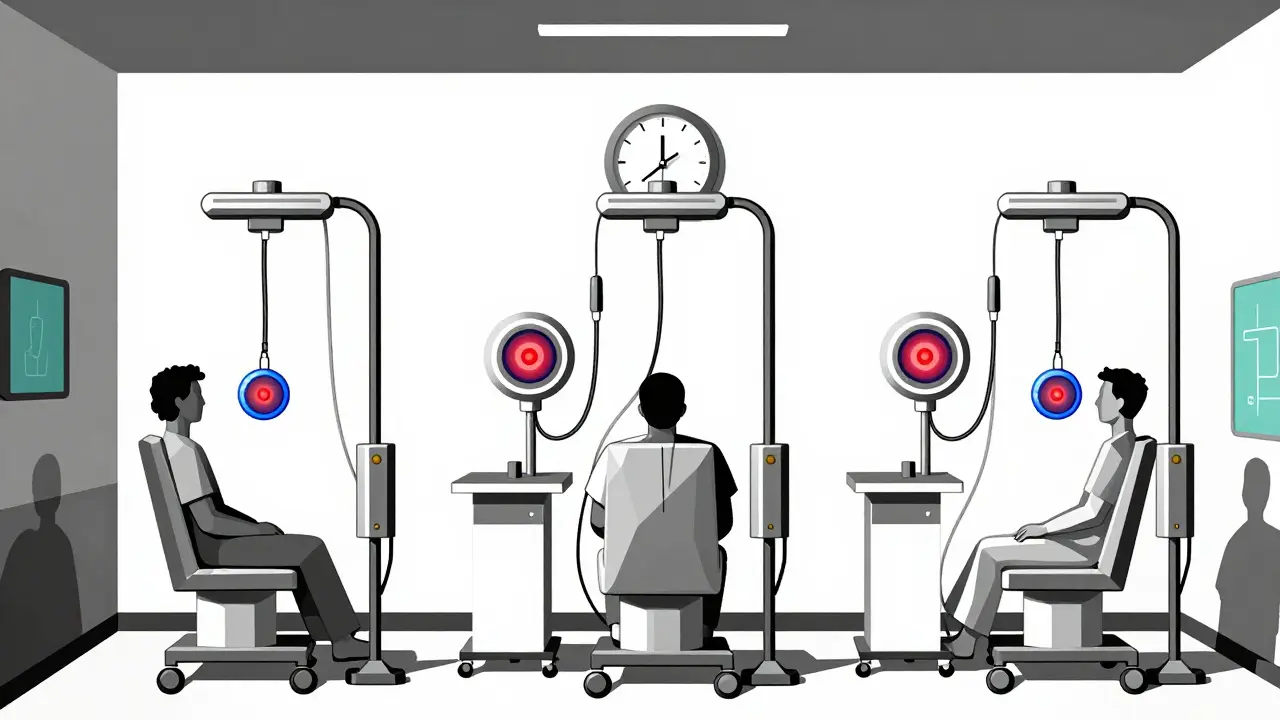
Hemodialysis uses a machine to clean your blood outside your body. Blood flows out through a tube, into a filter called a dialyzer, then back in. This process takes 3 to 5 hours, usually done three times a week at a clinic. Some people do it at home, but that requires space, training, and a water purification system.To get your blood to the machine, doctors create a vascular access. The best option is an arteriovenous (AV) fistula-a direct connection between an artery and vein in your arm. It takes 6 to 8 weeks to mature before it can be used. If that’s not possible, a graft or a central catheter may be used. Catheters are quick to set up but carry higher infection risks.
Each session removes a lot of waste quickly. The clearance rate, measured as Kt/V, is usually between 1.2 and 1.4 per treatment. That means your blood gets cleaned efficiently in a short window. But that speed comes with trade-offs. Your blood pressure can drop sharply during treatment. Many patients feel exhausted, nauseous, or crampy afterward. It’s common to feel wiped out for hours, sometimes all day.
How Peritoneal Dialysis Works
Peritoneal dialysis uses your own abdominal lining-the peritoneum-as a natural filter. A soft tube called a Tenckhoff catheter is surgically placed in your belly. You fill your abdomen with dialysis fluid, let it sit for 4 to 6 hours, then drain it out. This fluid pulls out waste and extra water through your peritoneal membrane.There are two types: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD). CAPD means you do 3 to 5 exchanges manually during the day, each taking about 30 minutes. APD uses a machine (a cycler) that does the exchanges while you sleep. You wake up with your belly empty and go about your day.
Unlike hemodialysis, peritoneal dialysis works slowly and continuously. Weekly Kt/V is usually 1.7 to 2.1-higher than what you get in a single hemodialysis session. Because it’s spread out, your body doesn’t experience the big swings in fluid and electrolytes. That means fewer crashes in blood pressure and heart rate. Studies show PD patients have better long-term control of blood pressure and less strain on the heart.
Which One Is More Effective?
There’s no single answer to “which is better.” Both keep you alive. But their strengths differ.A 2023 study from the First People’s Hospital of Tonglu County compared 77 PD patients to 74 HD patients. The PD group had significantly lower systolic and diastolic blood pressure, better control of parathyroid hormone, and fewer total complications. They also preserved their remaining kidney function longer.
Peritoneal dialysis removes toxins more gently and continuously. That’s why it’s often better for people with heart problems or unstable blood pressure. Hemodialysis clears toxins faster in a single session, which makes it the go-to for acute kidney failure or severe fluid overload.
But here’s the twist: long-term survival rates are similar between the two. A 2023 review in the Journal of Peritoneal Therapy and Clinical Practice found no consistent survival advantage for either. The real difference is in quality of life, flexibility, and how much your body can tolerate.
Side Effects and Risks
Every treatment has downsides.Hemodialysis risks include:
- Low blood pressure during treatment
- Vascular access infections or clotting
- Cramps and nausea
- Need for frequent clinic visits
- Time-consuming schedule-often 12+ hours per week spent traveling and sitting
Peritoneal dialysis risks include:
- Peritonitis (abdominal infection)-0.3 to 0.7 episodes per patient per year
- Catheter problems or blockages
- Weight gain from glucose in dialysis fluid
- Damage to the peritoneal membrane over time
- Need for strict sterile technique every time you exchange fluid
Patients on PD often say the biggest challenge is the daily routine. You’re always managing your catheter, storing bags of fluid, and worrying about infection. One Reddit user wrote: “I hate that I can’t just forget it exists. It’s always there.”
On the other hand, HD patients often say: “I feel like a number on a schedule.” The rigidity of clinic visits, the long waits, the feeling of being drained after each session-it wears on people.
Who Is a Better Candidate for Each?
Not everyone can do both.Peritoneal dialysis works best for people who:
- Are medically stable
- Have good manual dexterity (can handle small tubes and bags)
- Have no major abdominal scarring from past surgeries
- Have a supportive home environment
- Want to avoid frequent clinic visits
- Have heart conditions or unstable blood pressure
It’s harder for people with:
- BMI over 35 (obesity makes catheter placement and fluid distribution difficult)
- Severe hernias
- Very limited mobility or vision
- Difficulty learning new routines
Hemodialysis is often chosen for:
- Patients with advanced kidney failure and severe symptoms
- Those with abdominal issues that make PD unsafe
- People who prefer professionals handle their treatment
- Those with poor home support or unstable living situations
- Patients who need rapid fluid removal (like after a heart attack or severe fluid overload)
Age isn’t a hard barrier. Many older adults do PD successfully. But if someone has dementia, tremors, or can’t follow complex steps, HD at a clinic might be safer.
Cost, Convenience, and Lifestyle
Cost-wise, peritoneal dialysis is cheaper. A 2023 study in the Journal of Peritoneal Therapy and Clinical Practice found PD delivers better value for money. It uses fewer staff hours, less equipment, and reduces hospital visits.Convenience is where PD shines. You can do it while watching TV, working from home, or sleeping. No need to rearrange your life around clinic hours. Many patients say this freedom improves their mental health.
But here’s the catch: PD requires you to be your own nurse. You need a clean space, storage for dialysis fluid (about 20-30 bags per week), and the discipline to do exchanges on time. Miss one, and toxins build up. Do it wrong, and you risk infection.
Hemodialysis requires less daily effort-but you give up control. You’re tied to a schedule. Miss a session? You get sicker fast. Travel becomes harder. You can’t just hop on a plane without planning weeks ahead.
Global Trends and Future Outlook
In the U.S., 70% of dialysis patients are on hemodialysis. Only 12% use peritoneal dialysis. But that’s changing.In Hong Kong, 77% of patients use PD. In the U.K., it’s 22%. Why the difference? It’s not about medical superiority-it’s about healthcare systems. Countries with strong home dialysis programs and better training for nephrologists see higher PD use.
The U.S. Centers for Medicare & Medicaid Services launched a program in 2021 to push more patients toward home dialysis or transplant. By 2025, they want 80% of new patients to be educated on these options. That’s already moving the needle. Home dialysis (both PD and home HD) is growing at 2.5% per year.
Experts predict PD will rise to 18-22% of U.S. patients by 2027. Why? Because the data is clear: PD is gentler on the body, cheaper, and gives more freedom. The real barrier now isn’t medical-it’s education. Only 34% of U.S. nephrology fellows get proper PD training. Many doctors still think it’s “less effective,” even though studies show otherwise.
What Patients Really Say
A 2022 National Kidney Foundation survey asked patients how satisfied they were.- 68% of PD users said they were happy with their treatment flexibility.
- Only 32% of HD users felt the same.
- But 41% of PD users struggled with the physical demands of exchanges.
- Just 9% of HD users had trouble with the treatment itself.
On Reddit, one HD patient wrote: “I used to hate leaving my job every Tuesday, Thursday, Saturday. Now I do my dialysis while I sleep. I feel like I have my life back.”
Another PD user said: “I had peritonitis twice. I cried every time. But I still wouldn’t go back to the clinic. I’d rather deal with the risk than the schedule.”
There’s no perfect choice. But there is a right one-for you.
How to Decide
Ask yourself these questions:- Can I handle daily tasks like washing my hands, handling tubing, and following sterile steps?
- Do I have a quiet, clean space at home to store supplies?
- Am I comfortable with the idea of a tube in my belly forever?
- Do I want to avoid going to a clinic 3 times a week?
- Do I have heart problems or low blood pressure?
- Do I travel often or work irregular hours?
Talk to your nephrologist. Ask: “Which option gives me the best shot at staying healthy, feeling well, and living my life?” Don’t let fear of complexity push you toward HD if PD fits your life better. And don’t let the idea of freedom make you ignore the risks if you’re not ready to manage them.
Both treatments are life-saving. The goal isn’t to pick the “best” one-it’s to pick the one that lets you live the best life possible.
Can you switch from hemodialysis to peritoneal dialysis?
Yes, many people switch. But it’s not simple. You need to be medically stable, have no abdominal scarring, and be willing to learn a new routine. The catheter placement requires surgery and a 10-14 day healing period before starting. Some clinics offer transition programs to help patients make the change safely.
Is one treatment more painful than the other?
Hemodialysis can cause cramps, low blood pressure, and fatigue during or after sessions. Peritoneal dialysis involves minor discomfort during catheter insertion and occasional abdominal pressure during exchanges, but it’s usually not painful. Most patients say the daily hassle of PD is more mentally taxing than physically painful.
How long does it take to learn peritoneal dialysis?
Training typically takes 10 to 14 days. You’ll work with a dialysis nurse who teaches you how to do exchanges, recognize signs of infection, manage supplies, and handle emergencies. Many patients feel confident after a week of practice. The hardest part isn’t the technique-it’s sticking to the routine every single day.
Can you still travel with peritoneal dialysis?
Yes. Many PD patients travel with portable dialysis fluid supplies. You can ship bags ahead of time or buy them locally in most countries. APD users just need to bring their cycler. Some airlines allow the machine as medical equipment. HD patients often need to book clinic appointments abroad weeks in advance-something PD users rarely have to do.
Does peritoneal dialysis damage the kidneys faster?
No. In fact, studies show PD helps preserve remaining kidney function longer than hemodialysis. The gentle, continuous filtration reduces stress on the kidneys. HD’s rapid fluid shifts can accelerate loss of residual function. This is one reason PD is often recommended for patients who still have some kidney activity.
What happens if peritoneal dialysis stops working?
If the peritoneal membrane becomes too damaged or infected repeatedly, PD may no longer be effective. In that case, patients usually switch to hemodialysis. It’s not a failure-it’s a change in treatment plan. Many people live for years on PD, then transition smoothly to HD without major issues.







Write a comment