Heat Intolerance Risk Calculator
This tool helps you assess your risk of heat intolerance based on medications you're taking and environmental conditions. Select the medications you're currently using from the list below, and the calculator will determine your risk level.
Medication Selection
Select all medications you're currently taking that might affect your body's ability to cool down.
Environmental Factors
How hot is it where you are?
Your Heat Intolerance Risk Assessment
0
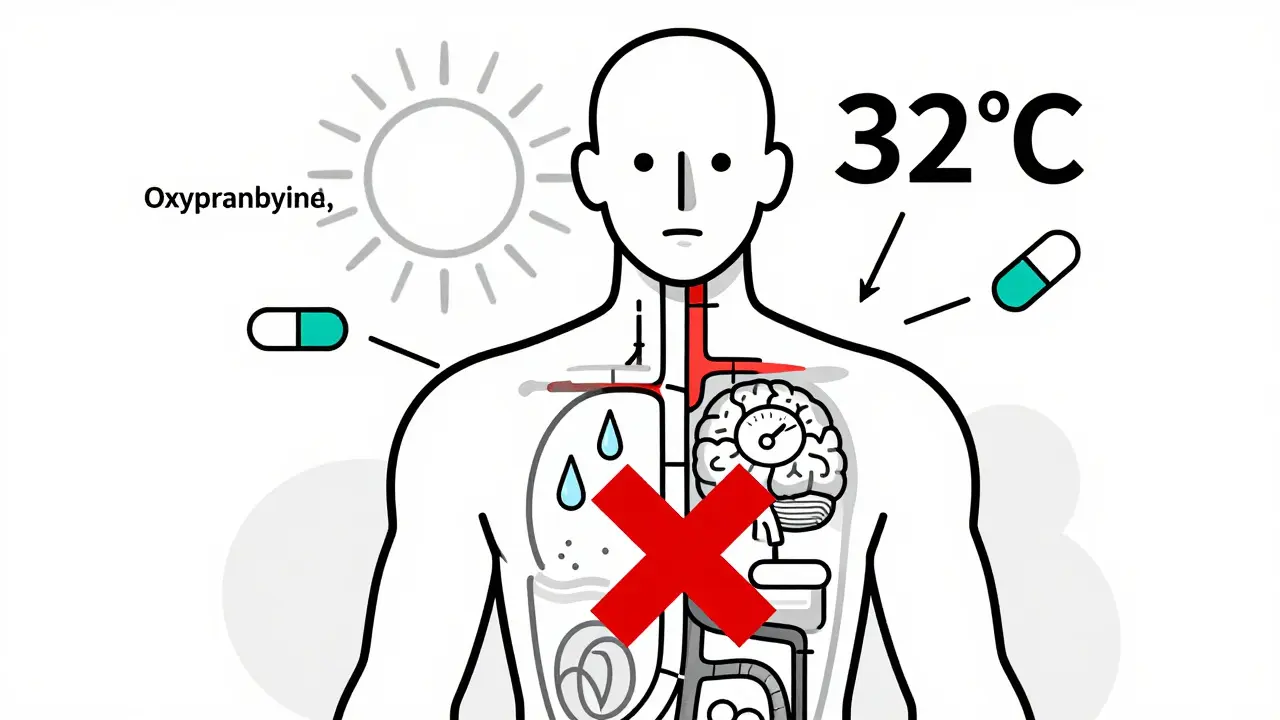
When the temperature climbs above 32°C (90°F), most people sweat to stay cool. But if you're taking certain medications, your body might not be able to sweat at all - and that’s not just uncomfortable. It’s dangerous. Heat intolerance from drugs isn’t rare. In fact, medication-induced heat intolerance is one of the most underrecognized risks in modern medicine. Around 15% of U.S. adults on prescription drugs experience this, and during heat waves, their risk of heat exhaustion or heat stroke jumps dramatically. If you or someone you care for is on long-term meds, this isn’t something to ignore.
How Medications Break Your Body’s Cooling System
Your body cools itself in two main ways: sweating and blood flow to the skin. When it gets hot, your brain tells sweat glands to produce moisture, and your blood vessels widen to carry heat to the surface. Medications can interfere with either - or both.
Take diuretics, like hydrochlorothiazide or chlorthalidone. These are commonly prescribed for high blood pressure or swelling. They make you pee more - sometimes 1.5 to 2.5 liters a day. Less fluid means less sweat. Studies show this can cut your sweating capacity by 30-50%. In hot weather, that’s like trying to cool down with half your normal radiator. A 2022 Kaiser Permanente study found people on hydrochlorothiazide had 2.3 times the risk of heat exhaustion during summer heat waves.
Beta blockers - such as metoprolol or propranolol - work differently. They don’t reduce fluid, but they block your body’s ability to send blood to the skin. Research shows these drugs reduce cutaneous blood flow by 25-40%. That means heat gets trapped inside. Even if you’re sweating, your skin stays warm because the heat can’t escape. A 2024 study found patients on propranolol had a 0.15°C higher core temperature during heat exposure than those not on the drug.
Anticholinergics are another big offender. These include drugs for overactive bladder (oxybutynin), allergies (diphenhydramine/Benadryl), and some antidepressants. They block acetylcholine - the chemical that tells sweat glands to activate. In some cases, sweating drops by 60-80%. That’s not just dry skin - it’s a total shutdown of your main cooling system. The CDC warns this group is among the highest risk for heat stroke, even at temperatures as low as 27°C (80°F).
The Most Dangerous Drug Classes
Not all medications affect heat the same way. Some are worse than others.
Antipsychotics like olanzapine, risperidone, and haloperidol are the most dangerous. They don’t just reduce sweating - they confuse your brain’s thermostat. These drugs directly disrupt the hypothalamus, the part of your brain that controls body temperature. Studies show they can cut sweating by 50-70% and raise core temperature even in mild heat. People on these drugs have been hospitalized at 29°C (85°F) - a temperature most people handle just fine.
Tricyclic antidepressants (TCAs) like amitriptyline and clomipramine also severely reduce sweating - by 65-75%. But here’s the twist: SSRIs like fluoxetine or sertraline do the opposite. They often increase sweating, sometimes to the point of causing dehydration. So if you switch from a TCA to an SSRI, you might go from not sweating at all to sweating too much - and still end up dehydrated.
Stimulants like Adderall and Ritalin are another surprise. They don’t stop sweating. They make you hotter. These drugs boost your metabolism by 15-25%, meaning your body generates more internal heat. At the same time, they can reduce your ability to sweat efficiently. It’s a double hit: more heat, less cooling.
GLP-1 agonists like Ozempic and Wegovy are newer but already a concern. These drugs suppress thirst by 40-50%. That means you don’t feel thirsty - even when you’re dehydrated. You might drink water, but your brain isn’t telling you to keep going. A 2023 clinical trial showed users of semaglutide often drank less than 1.5 liters of fluid a day, even in hot weather. That’s far below what’s needed to stay safe.
Who’s at Highest Risk?
It’s not just about the drug - it’s about how many you’re taking. People on three or more heat-affecting medications have a much higher risk. The CDC found that 18-22% of heat-related ER visits in adults over 50 involve these drugs. And it gets worse with age.
Adults over 65 are especially vulnerable. Their bodies naturally sweat less. Their kidneys don’t hold fluid as well. And they’re more likely to be on multiple medications. The American Geriatrics Society says having five or more medications increases heat stroke risk by 300% compared to younger people. Lithium - used for bipolar disorder - is especially risky. Dehydration can spike lithium levels by 25-35%, leading to toxicity. That’s why the CDC recommends checking blood levels during heat waves.
Climate change is making this worse. With 2023 being the hottest year on record, and projections showing a 40-60% rise in heat-related medication complications by 2050, this isn’t a seasonal issue anymore. It’s a long-term health threat.

Warning Signs You’re in Danger
Heat intolerance doesn’t always come with a siren. Symptoms can sneak up. Look for:
- Cramps (happens in 65% of cases)
- Dizziness or lightheadedness (55%)
- Headache (70%)
- Flushed or dry skin (45%)
- Lack of sweating - or suddenly stopping sweat
- Nausea or vomiting (35%)
- Weakness or fatigue (60%)
These symptoms usually show up within 30-90 minutes of being in the heat. If you’re on any of these medications and notice even one, get out of the heat immediately. Don’t wait for confusion or fainting - that’s already heat stroke.
What You Can Do to Stay Safe
There’s no magic fix - but there are clear steps that work.
- Drink more water - even if you’re not thirsty. Add 500-1000 mL extra per day during hot weather. For people on GLP-1 drugs, this isn’t optional - it’s life-saving.
- Avoid the sun between 10 AM and 4 PM. That’s when UV radiation and heat peak. If you must go out, stay in shade and wear a wide-brimmed hat.
- Use air conditioning. Even a few hours a day helps your body recover. If you don’t have AC, visit a library, mall, or cooling center. Many cities offer these during heat advisories.
- Monitor your weight. Losing more than 2% of your body weight in a day means you’re dangerously dehydrated. Weigh yourself daily in the morning.
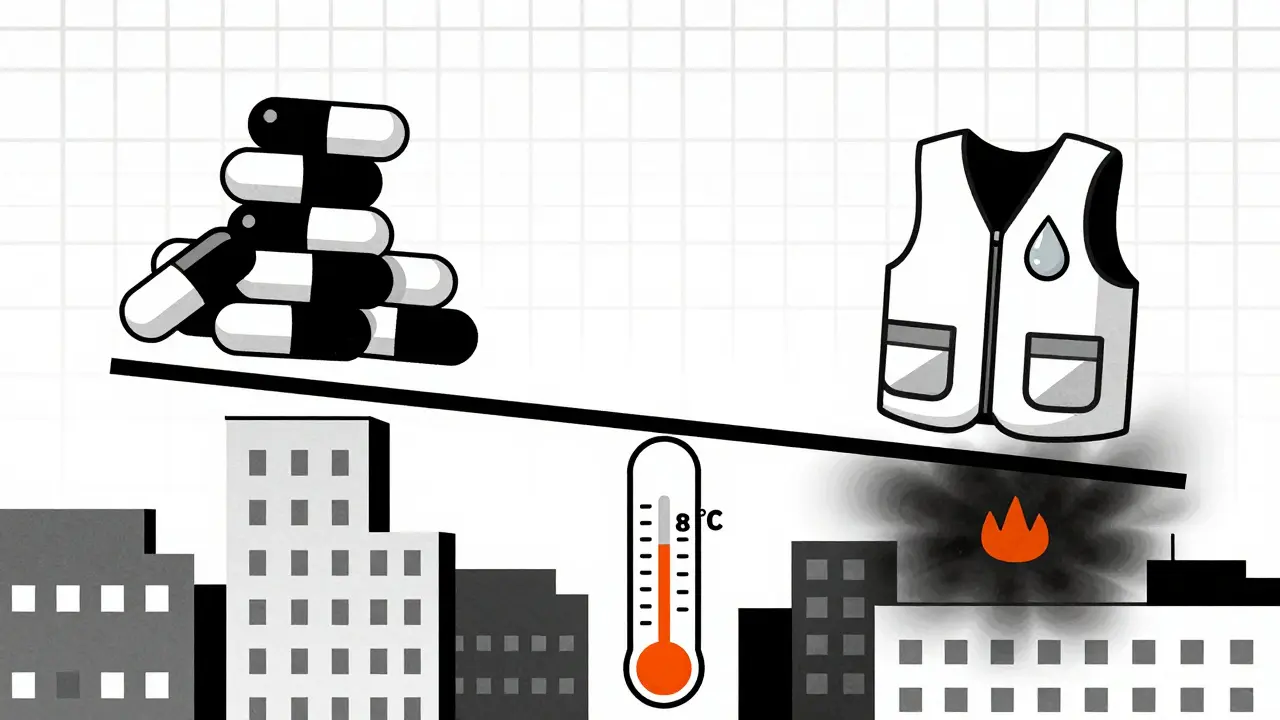
- Wear cooling gear. Cooling vests - now used in hospitals - can lower core temperature by 0.5-1.0°C. They’re affordable and available online. For people on antipsychotics or anticholinergics, they’re a game-changer.
- Check your meds. Talk to your doctor about alternatives. Sometimes switching from a diuretic to a potassium-sparing one, or from a TCA to an SSRI, can reduce risk. Don’t stop meds on your own - but do ask.
Also, if you’re on calcium channel blockers, ACE inhibitors, or ARBs, use SPF 30+ sunscreen. These drugs can make your skin more sensitive to sunburn - and sunburn makes heat stress worse.
What’s New in 2026?
Technology is catching up. In December 2023, the FDA approved the first wearable core temperature monitor - TempTraq - specifically for people on heat-affecting drugs. It tracks your internal temperature continuously and alerts you if it rises above safe levels. Electronic health records now include automatic alerts when patients are prescribed multiple high-risk drugs. In July 2023, Epic Systems added heat risk warnings for 14 drug classes during summer months.
Research is moving fast. The NIH is funding a $2.5 million study starting in September 2024 to build AI tools that predict heat risk based on your exact drug combination. The goal? To give each patient a personalized safety plan - not a one-size-fits-all warning.
Final Thought
Heat intolerance from medication isn’t a side effect you can ignore. It’s not just about discomfort. It’s about survival. If you’re on diuretics, anticholinergics, beta blockers, antipsychotics, stimulants, or GLP-1 drugs - and you live in a place where summer temperatures hit 30°C or more - you need a plan. Talk to your doctor. Know your symptoms. Stay hydrated. Avoid the sun. Use cooling tools. Your body’s ability to cool down is fragile. Don’t let your meds take it away.
Can I stop my medication if it causes heat intolerance?
No - never stop a prescribed medication without talking to your doctor. Many of these drugs treat serious conditions like high blood pressure, depression, or diabetes. Stopping them suddenly can be dangerous. Instead, ask your doctor if there’s a safer alternative. For example, switching from a thiazide diuretic to a potassium-sparing diuretic, or from a TCA to an SSRI, might reduce heat risk without compromising your health.
Do all people on these medications get heat intolerance?
No. Risk varies by dose, age, overall health, and environment. Someone on a low dose of hydrochlorothiazide who drinks plenty of water and stays indoors during heat waves may never have an issue. But someone on multiple high-risk drugs, over 65, with kidney problems, and who works outside is at very high risk. It’s not guaranteed - but it’s common enough that everyone on these meds should assume they’re at risk and take precautions.
Is heat intolerance reversible when I stop the medication?
Usually, yes. Once you stop the drug (under medical supervision), your body’s thermoregulation system typically returns to normal within days to weeks. For example, sweating returns within 3-7 days after stopping anticholinergics. But if you’ve had repeated heat injuries or are older, recovery may take longer. Always follow up with your doctor after making changes.
Can I still exercise if I’m on these medications?
Yes - but with major adjustments. Avoid outdoor exercise during hot hours. Stick to early morning or evening, and only if it’s under 27°C (80°F). Use fans, air conditioning, or indoor equipment. Drink water before, during, and after. Monitor for symptoms. If you feel dizzy, stop immediately. Some people on beta blockers or diuretics need to reduce workout intensity. Talk to your doctor about safe activity levels.
Are there any over-the-counter drugs that cause heat intolerance?
Yes. Many OTC meds can cause this. Diphenhydramine (Benadryl), doxylamine (Unisom), and some cold/flu remedies contain anticholinergics. Pain relievers like ibuprofen and naproxen can reduce kidney function in heat, increasing dehydration risk. Even some herbal supplements - like valerian root or kava - have anticholinergic effects. Always read labels and check with a pharmacist if you’re unsure.
What should I do if I think I’m having heat stroke?
Call emergency services immediately. While waiting, get out of the heat, remove clothing, and cool down with cold water or ice packs on your neck, armpits, and groin. Do not drink water if you’re confused or vomiting - that can cause choking. Heat stroke is life-threatening. Never wait to see if it gets better. Time matters.

Write a comment