Why Mixing Up Side Effects and Allergies Can Hurt Your Health
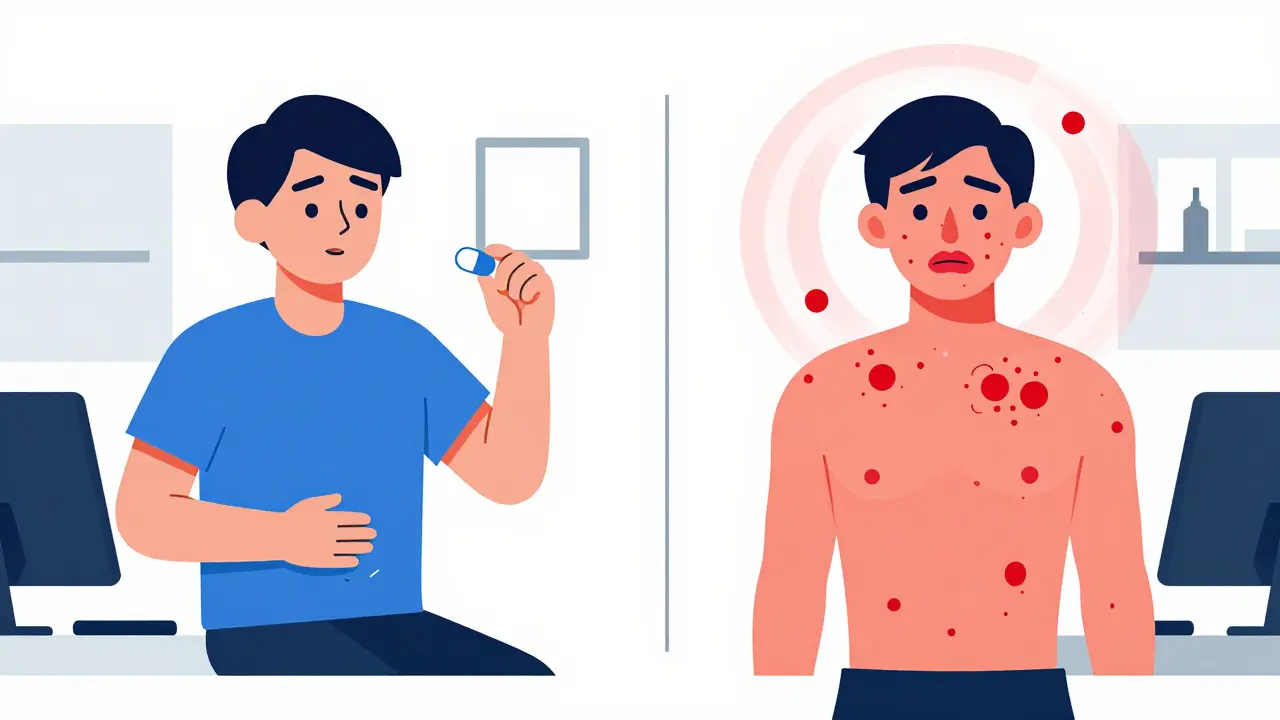
You start a new medication. A few days later, your stomach feels queasy. You get a rash. You feel dizzy. Your first thought? Allergy. But what if it’s not? Confusing a side effect with a true allergy isn’t just a mistake-it can lead to worse treatments, higher costs, and even dangerous antibiotic overuse.
According to the CDC, about 1.3 million emergency visits each year in the U.S. are caused by bad reactions to medications. And here’s the kicker: up to 70% of people who say they’re allergic to penicillin aren’t. They just had a side effect-like nausea or a mild rash-and labeled it wrong. That’s not just inaccurate. It means doctors skip the safest, most effective drug and reach for something stronger, costlier, and more likely to cause antibiotic resistance.
Side effects and allergies are not the same thing. Side effects are predictable, common, and usually harmless. Allergies are immune system overreactions that can be life-threatening. Knowing the difference isn’t just helpful-it’s essential for getting the right care.
Side Effects: Expected, Not Dangerous
Side effects happen because your body is adjusting to a new chemical. They’re not your immune system attacking the drug-they’re just the drug doing things it wasn’t meant to do.
Take statins, for example. One in five people on these cholesterol-lowering pills gets muscle aches. That’s a side effect. Or NSAIDs like ibuprofen? About 20% of users get stomach upset. Drowsiness from diphenhydramine (Benadryl)? Happens in over half the people who take it.
The good news? Most side effects fade. About 60-70% of them disappear within two to four weeks as your body gets used to the medication. If you’re feeling a little tired after starting a blood pressure pill, or your appetite drops after a new antidepressant, it’s likely not an emergency. But it still needs to be talked about.
Allergic Reactions: The Real Emergency
An allergic reaction is your immune system treating the drug like a threat. It doesn’t matter how much you take-even one pill can trigger it. Symptoms show up fast: within minutes to a few hours after taking the medication.
Look for these red flags:
- Hives or raised, itchy welts on the skin
- Swelling of the lips, tongue, or throat
- Difficulty breathing or wheezing
- Dizziness, rapid pulse, or feeling like you’re going to pass out
If you get any of these, stop the medication and get help immediately. Anaphylaxis-a severe allergic reaction-can kill within minutes. About 1 in 10,000 people on antibiotics end up in the hospital because of it.
Even if you’ve only had a mild rash before, don’t assume it’s safe to take the drug again. Allergies can get worse with each exposure. And if you’ve ever had swelling or breathing trouble, you need to be evaluated by an allergist.
How to Talk to Your Doctor Without Getting Misunderstood
Doctors hear “I’m allergic to this” all the time. But they can’t fix what they don’t understand. If you say, “I got sick after taking amoxicillin,” they don’t know if you had diarrhea (side effect) or broke out in hives (allergy).
Here’s how to make it clear:
- Be specific about timing: “I took the pill at 8 a.m. and broke out in hives by 10 a.m.” That’s an allergy. “I took it at 8 a.m. and felt nauseous by 2 p.m.” That’s a side effect.
- Describe the symptom, not just the feeling: Say “red, itchy bumps” instead of “I broke out.” Say “my throat felt tight” instead of “I felt weird.”
- Track how long it lasted: Did the rash go away in a day? Or did it come back every time you took the pill?
- Know if it got worse with more doses: Side effects often get better. Allergies get worse.
One study found patients who used this exact language got accurate assessments 89% of the time. Those who just said “it made me feel bad”? Only 52%.
What to Bring to Your Appointment
Don’t rely on memory. Your brain is busy. Your doctor is busy. Bring proof.
- Your medication bottles: Even empty ones. This cuts down on mix-ups. One hospital study showed bringing bottles reduces errors by 28%.
- A symptom log: Write down the date, time, medication name, dose, symptom, severity (1-10), and how long it lasted. Do this for at least 72 hours before your visit. Patients who do this are over three times more likely to get the right adjustment.
- A list of questions: Write these down before you go:
- Is this a known side effect or a possible allergy?
- How soon after taking it did the symptom start?
- Is there another drug in a different class I could try?
- Should I see an allergist to get tested?
Use the S.O.A.P. method to organize your thoughts:
- Subjective: “I felt dizzy after taking the pill.”
- Objective: “My blood pressure dropped 15 points after the second dose.”
- Assessment: “This happened every time I took it, within 2 hours.”
- Plan: “Can we try a different blood pressure med?”
What Happens When You Get It Wrong
Getting the label wrong has real consequences.
People labeled as penicillin-allergic are given broader-spectrum antibiotics 63% more often. These drugs are more expensive, more likely to cause C. diff infections, and fuel antibiotic resistance. The Institute for Safe Medication Practices estimates this adds $1,200-$2,500 in extra costs per person every year.
And it’s not just penicillin. One patient in San Diego had chronic headaches for months. Her doctor thought it was migraines. Turns out, it was a side effect of her blood pressure medication. She was put on two other drugs before someone finally asked: “When did the headaches start?”
That’s the problem. Side effects get misdiagnosed as new conditions. Allergies get ignored because they’re “just a rash.” Both lead to unnecessary treatments, more pills, and more risk.
What’s Being Done to Fix This
Hospitals and pharmacies are catching on.
The American Academy of Allergy, Asthma & Immunology now uses a standardized “Allergy Reconciliation Protocol.” Clinics using it cut penicillin mislabeling by 62%. The FDA now requires all new patient medication guides to clearly separate side effects from allergic reaction symptoms. And the CDC’s National Action Plan aims to reduce these communication errors by 30% by 2026.
There’s also a free app now-the Medication Reaction Tracker-launched in January 2023. It walks you through questions like: “Did the symptom happen within hours of taking the drug?” and “Did it get worse with more doses?” It’s been downloaded over 87,000 times.
What You Can Do Today
You don’t need to wait for your next appointment to start fixing this.
- Check your own records: Look at your chart. Do you have a penicillin allergy listed? If you’ve never been tested, ask if you can get a skin test. Over 90% of people who think they’re allergic can safely take it.
- Start a symptom log: Grab a notebook or use your phone. Track every new medication, every symptom, every time.
- Ask the right question next time: “Is this a side effect or a true allergy? Can we rule out an allergy with a test?”
- Don’t assume you’re allergic just because someone else is: Your body reacts differently. Don’t let your mom’s penicillin reaction become your label.
Medications are powerful. But they’re only safe if you and your care team understand what’s really happening in your body. Don’t let a simple mix-up cost you your health-or your future treatment options.






Write a comment