When pain sticks around, it’s not just your body that suffers-it’s your mind too. Many people with long-term pain start thinking, "This will never get better," "I can’t handle this," or "Something terrible is happening." These aren’t just bad thoughts-they’re a psychological pattern called pain catastrophizing. And it makes the pain feel worse, drains your energy, and keeps you stuck in a cycle of fear and avoidance.
Research shows pain catastrophizing is one of the strongest predictors of poor outcomes in chronic pain. People who catastrophize report higher pain intensity, more disability, and even greater risk of depression and anxiety. But here’s the good news: you don’t have to stay trapped in this cycle. Cognitive Behavioral Therapy (CBT) offers real, evidence-backed tools to break it.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing isn’t just being negative. It’s a specific pattern of thinking that kicks in when you’re in pain-or even when you anticipate it. The Pain Catastrophizing Scale (PCS), developed in the 1990s, breaks it down into three parts:
- Rumination: You can’t stop thinking about the pain. It replays in your head like a broken record.
- Magnification: You assume the worst. A small ache becomes a sign of something serious, like nerve damage or a worsening condition.
- Helplessness: You feel powerless. No matter what you do, you believe the pain will win.
These thoughts aren’t just in your head-they affect your body. Brain scans show that when you catastrophize, areas linked to emotion and pain processing light up more intensely. That means your thoughts are literally turning up the volume on your pain.
Think of it this way: if you twist your ankle, the injury causes pain. But if you start thinking, "This is it-I’ll never walk normally again," your brain adds emotional pain on top of physical pain. That’s catastrophizing. And it’s what CBT is designed to untangle.
How CBT Breaks the Cycle
CBT doesn’t tell you to ignore your pain. It doesn’t say your pain isn’t real. Instead, it helps you see how your thoughts about pain make it worse-and gives you tools to change that.
The goal isn’t to eliminate pain. It’s to reduce the distress around it. Studies show that when people lower their catastrophizing scores, their pain intensity drops too-even if the physical cause hasn’t changed. That’s because CBT targets the mental loop that amplifies suffering.
A 2024 study in Nature Scientific Reports used network analysis to map how pain and catastrophic thoughts connect. Before CBT, the two were tangled together-like a knot. After therapy, the knot loosened. Pain and thoughts became separate. That’s the breakthrough.
Three CBT Tools That Actually Work
Effective CBT for pain catastrophizing isn’t vague advice. It’s structured, practical, and built on decades of research. Here are the three most powerful tools:
1. Self-Monitoring: Catch the Thought Before It Escalates
This is where you start. You keep a simple log: when pain flares up, write down:
- What you were doing
- What you thought
- How you felt emotionally
- How your body reacted
Example: "I tried to carry groceries. Thought: ‘I’m going to ruin my back for good.’ Felt: terrified. Body: muscles locked up, pain spiked to 8/10."
This isn’t about blaming yourself. It’s about noticing patterns. Most people don’t realize how often they jump to catastrophic conclusions. Writing it down makes the thoughts visible-and easier to challenge.
2. Cognitive Restructuring: Replace "What If?" with "What Now?"
Once you spot a catastrophic thought, you don’t just push it away. You question it.
Ask yourself:
- Is this thought based on facts or fear?
- What’s the evidence for and against this thought?
- What’s a more balanced way to see this?
Instead of: "This pain means I’m getting worse," try: "Pain flares happen. It doesn’t mean my condition is changing. I’ve handled this before."
One patient with fibromyalgia reduced her PCS score from 42 to 18 over 12 weeks using this method. Her pain intensity dropped by half. She returned to part-time work.
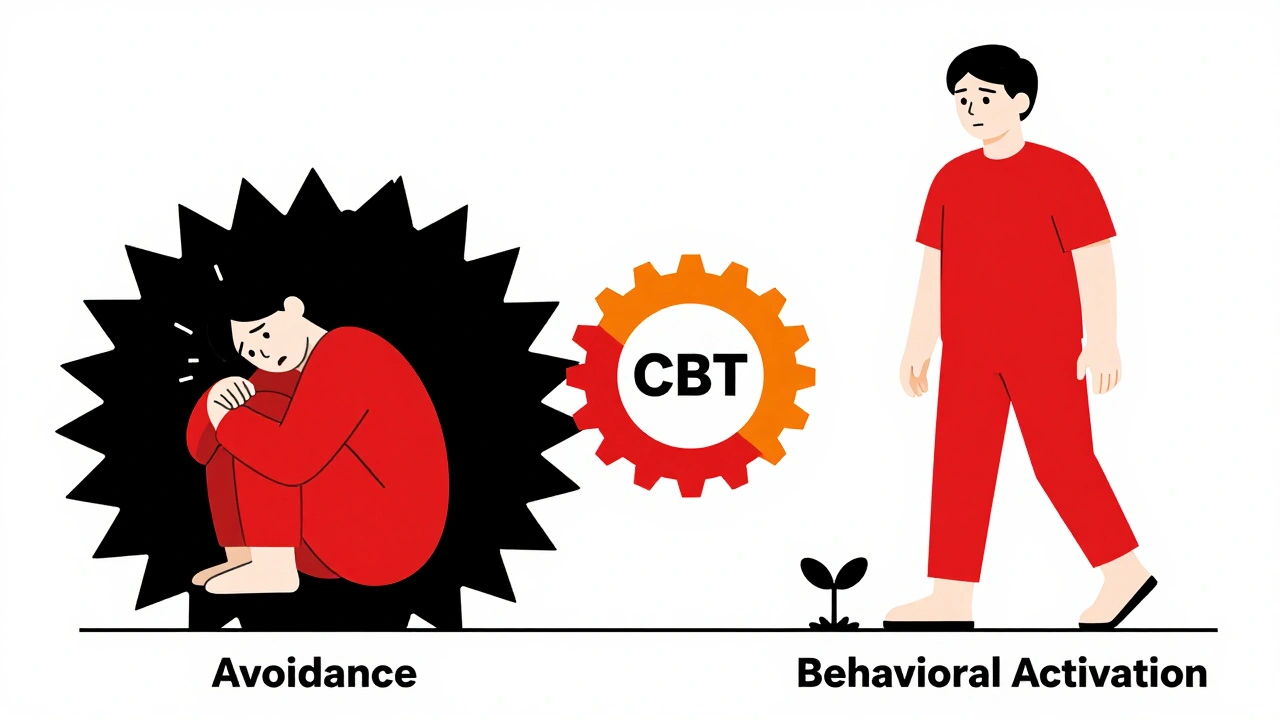
3. Behavioral Activation: Move Even When You Don’t Want To
Catastrophizing leads to avoidance. You stop walking, cooking, socializing-anything that might trigger pain. But avoidance makes your body weaker and your mind more fearful.
Behavioral activation means doing small, meaningful activities even when pain is present. Start tiny: five minutes of stretching, a short walk around the block, calling a friend.
It’s not about pushing through pain. It’s about proving to yourself that pain doesn’t have to control your life. Over time, your brain learns: "I can do things even with pain. It won’t destroy me."
What the Research Says About Effectiveness
CBT isn’t just popular-it’s proven.
A 2023 review by the International Association for the Study of Pain found that when studies focused specifically on reducing pain catastrophizing, CBT was the most effective treatment. Its effect size was nearly double that of other therapies.
Combining CBT with gentle movement or exercise boosted results even further. People who did both saw the biggest improvements in pain, mood, and function.
Compare that to Acceptance and Commitment Therapy (ACT). While ACT helps, studies show it has a smaller impact on catastrophizing specifically. CBT wins here because it directly targets the thinking patterns that fuel the problem.
And it’s not just in labs. The Veterans Health Administration screens every chronic pain patient for catastrophizing. Since 2020, they’ve offered CBT to over a million veterans. Results? 92% report high satisfaction. Many say CBT gave them back control.
Real People, Real Results-and Real Challenges
Success stories are common. On Reddit’s chronic pain forums, 78% of users who tried CBT said it reduced their distress. One wrote: "I finally understood that my thoughts were making the pain louder. CBT gave me the quiet."
But it’s not easy. Some people struggle when pain is high. One user on PainForum.org said: "When my pain hits 8/10, I can’t think straight. How am I supposed to do CBT then?"
That’s a real barrier. CBT requires mental energy. If you’re exhausted, overwhelmed, or in severe pain, the techniques can feel impossible. That’s why pacing matters. Start with one tool-maybe just self-monitoring. Don’t try to do everything at once.
Dropout rates are around 22%. The main reason? People expect quick fixes. CBT takes 8 to 12 weeks to show real change. It’s not magic. It’s practice.
Getting Started: What to Expect
Most CBT programs for pain last 8 to 12 weeks, with weekly 60-minute sessions. You’ll start with a PCS assessment. A score above 30 means you’re in the clinically significant range-and CBT is likely to help.
Weeks 1-3: You learn about catastrophizing. You begin tracking thoughts.
Weeks 4-8: You challenge distorted thoughts. You start small activities.
Weeks 9-12: You build confidence. You plan for setbacks.
You don’t need to be a therapist to use these tools. Many apps now offer guided CBT for pain, like Curable and PainScale. They’ve reached over 450,000 users since 2020.
And the field is evolving. The VA is rolling out digital dashboards that track pain and thoughts in real time. By 2025, most pain clinics will screen for catastrophizing. Soon, you might get a smartphone alert: "You’ve been ruminating for 10 minutes. Try a grounding exercise."
Who Benefits Most?
CBT works best for people who:
- Have chronic pain that hasn’t improved with meds or physical therapy
- Feel stuck in fear or avoidance
- Are willing to practice daily, even for a few minutes
- Want to understand how their mind affects their pain
It’s less effective if you have severe depression, PTSD, or active substance use. Those issues need to be addressed first.
And while education helps-people with some college education tend to do better-you don’t need a degree to benefit. Just curiosity and persistence.
Why This Matters Now
The global chronic pain market is worth over $75 billion. But drugs and surgeries often fail. The real gap? Addressing the psychological side of pain.
Pain catastrophizing is the missing piece. It’s not a weakness. It’s a learned response. And like any learned behavior, it can be unlearned.
CBT doesn’t promise to erase pain. But it gives you power over how you respond to it. And that’s what makes the difference between suffering and living.
Is pain catastrophizing the same as being depressed?
No. While pain catastrophizing often goes hand-in-hand with depression, they’re different. Catastrophizing is a specific thinking pattern focused on pain-like magnifying danger or feeling helpless. Depression is a broader mood disorder with symptoms like low energy, loss of interest, and sadness. You can catastrophize without being depressed, and vice versa. But they feed each other. Treating catastrophizing often improves mood, even without antidepressants.
Can CBT help if my pain is caused by a serious condition like arthritis or nerve damage?
Yes. CBT doesn’t treat the physical cause of pain-it treats your response to it. Whether your pain comes from arthritis, sciatica, or fibromyalgia, catastrophizing still makes it worse. Studies show CBT reduces pain intensity and improves function regardless of the diagnosis. It helps you live better with pain, even if you can’t cure it.
How long does it take to see results from CBT for pain catastrophizing?
Most people start noticing changes in 4 to 6 weeks. You’ll begin to catch catastrophic thoughts faster and feel less overwhelmed. But real shifts-like returning to activities you avoided-usually take 8 to 12 weeks. It’s not instant, but the results last. Unlike painkillers, CBT teaches skills you keep using long after therapy ends.
What if I can’t afford therapy?
You don’t need a therapist to use CBT tools. Many free or low-cost apps offer guided CBT for pain, including Curable, PainScale, and the VA’s free digital resources. Libraries and community health centers sometimes offer group CBT programs. You can also find workbooks like "The Chronic Pain Solution" by Dr. David Hanscom. The core techniques-self-monitoring, challenging thoughts, pacing activities-can be practiced alone.
Does CBT work for acute pain too?
It’s designed for chronic pain, but early use can prevent catastrophizing from taking root. After surgery or injury, if you start noticing thoughts like "This will never heal," using CBT tools can stop the cycle before it becomes ingrained. Prevention is easier than reversal.
If you’re tired of letting pain dictate your life, CBT offers a way out. It’s not about denying your pain. It’s about reclaiming your mind. And that’s where real healing begins.







Write a comment