Women with polycystic ovary syndrome (PCOS) often struggle with more than irregular periods or acne. For 50 to 80% of them, excess weight is a constant, frustrating reality-and it’s not just about appearance. Carrying extra weight makes insulin resistance worse, drives up testosterone levels, and shuts down ovulation. Traditional treatments like metformin help, but they rarely deliver the kind of weight loss that turns things around. That’s where GLP-1 receptor agonists come in. These aren’t magic pills, but they’re the most effective weight-loss drugs we’ve seen for PCOS in decades.
How GLP-1s Actually Work in PCOS
GLP-1s-like liraglutide and semaglutide-were originally made for type 2 diabetes. But their power goes far beyond blood sugar. These drugs mimic a natural gut hormone that tells your brain you’re full, slows down digestion, and helps your pancreas release insulin only when needed. For someone with PCOS, that’s a game-changer.
When you take a GLP-1 agonist, you don’t just eat less-you crave less. The hunger signals from your brain quiet down. Food doesn’t feel like the only comfort left. That’s why women on semaglutide often report losing weight even without drastic diet changes. Studies show that after 68 weeks on semaglutide 2.4 mg, people without diabetes lost nearly 15% of their body weight. In PCOS-specific trials, the average was 10-12%. That’s not a few pounds. That’s enough to reset hormones.
And it’s not just weight. Testosterone levels drop. Fasting insulin improves. Liver fat decreases. Even cholesterol gets better. One study found that after 24 weeks on liraglutide, 42% of women with PCOS started ovulating again-without fertility drugs. That’s not coincidence. It’s metabolic healing.
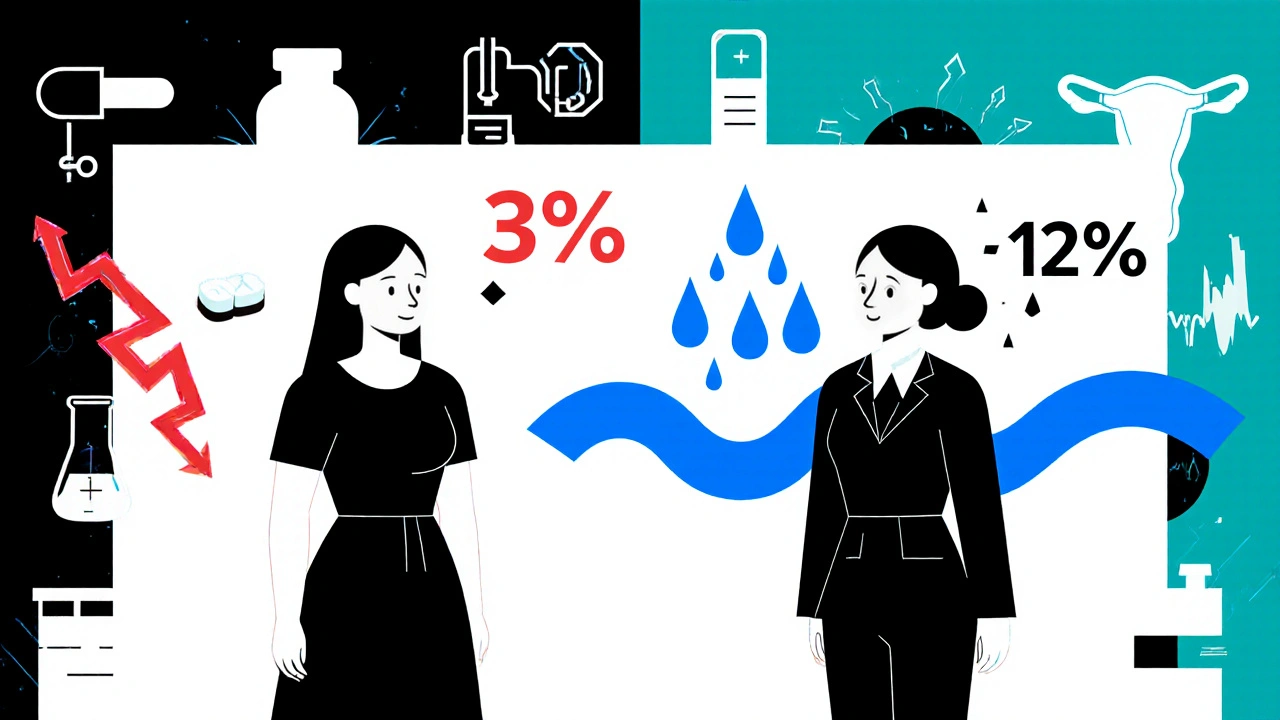
GLP-1s vs. Metformin: The Real Difference
Metformin has been the go-to for PCOS for over 20 years. It’s cheap, safe, and helps with insulin resistance. But here’s the truth: most women on metformin lose 2-4% of their body weight. That’s helpful, but not transformative. GLP-1s? They consistently deliver 5-12% weight loss in PCOS patients. That’s the difference between feeling a little better and feeling like your body is finally working with you.
One 2024 study directly compared liraglutide and metformin in women with PCOS. The liraglutide group lost 7.8% of their weight on average. The metformin group? 3.1%. The GLP-1 group also saw bigger drops in waist size, liver enzymes, and androgen levels. Metformin is still useful-especially if you’re on a budget or can’t tolerate injections. But if you’ve tried it and hit a wall, GLP-1s are the next step.
What the Numbers Really Show
Let’s cut through the noise. Here’s what actual clinical data says about GLP-1s in PCOS:
- Weight loss: Average 5.6% with semaglutide over 12 weeks; up to 14.9% over 68 weeks
- BMI reduction: 1.59 kg/m² lower than placebo, 1.11 kg/m² lower than metformin
- Visceral fat: Reduced by 18% in trials-this is the dangerous fat around organs
- Testosterone: Drops of 20-30% reported in multiple studies
- Menstrual regularity: Improved in 68% of users after 24 weeks
- Ovulation: Spontaneous ovulation occurred in 42% of women on liraglutide
These aren’t small changes. Losing 10% of your body weight can reverse insulin resistance, lower inflammation, and restore ovulation. For many women with PCOS, that’s the difference between needing fertility treatment and conceiving naturally.
The Side Effects Nobody Talks About
GLP-1s aren’t risk-free. The most common problem? Nausea. Up to 44% of users feel sick, especially when starting. Vomiting happens in 24%. Dizziness in 15%. These aren’t rare. They’re expected.
But here’s what most doctors don’t tell you: these side effects usually fade. Starting low-like 0.25 mg of semaglutide weekly-and slowly increasing over 16-20 weeks makes a huge difference. Eating smaller, low-fat meals helps. Skipping sugary drinks helps even more. Many women say the nausea peaks at week 2 and is gone by week 6.
Other issues: injection site reactions (redness, itching), constipation, or feeling fatigued. About 15-20% of people stop because of side effects. That’s not nothing. But for many, the trade-off is worth it. One Reddit user wrote: “I lost 28 lbs, my testosterone dropped from 68 to 42, and I had my first regular period in 3 years.” That’s not an outlier. It’s a pattern.
Cost, Access, and the Real Barriers
Let’s be honest: GLP-1s are expensive. Brand-name semaglutide (Wegovy) or liraglutide (Saxenda) can cost $800 to $1,400 a month in Australia without insurance. Generic metformin? $15. That’s why many women can’t access them-even if their doctor prescribes them.
Off-label use for PCOS is growing fast. In 2023, an estimated 15-20% of GLP-1 prescriptions in the U.S. were for PCOS, even though it’s not yet an approved use. Europe is moving faster: in June 2024, the EMA accepted Novo Nordisk’s application to approve semaglutide 2.4 mg specifically for obese women with PCOS. A decision is expected in early 2025.
Some women are switching to compounded versions or buying from overseas pharmacies. But that comes with risks-contamination, incorrect dosing, no medical oversight. If you’re considering this route, talk to your endocrinologist first. There’s no shortcut to safety.
What Happens When You Stop?
Weight comes back if you stop. That’s true for every weight-loss drug. But with GLP-1s, the rebound can be sharp.
One 2024 study followed women who stopped semaglutide after 68 weeks. Those who stopped completely regained 60-70% of their lost weight in two years. But those who stayed on metformin after stopping the GLP-1? They only regained one-third. That’s huge. It means GLP-1s aren’t meant to be short-term fixes. They’re a bridge. And metformin is the safety net.
Doctors are starting to recommend a “step-down” plan: use the GLP-1 to lose weight, then keep metformin going to hold onto the gains. Lifestyle changes-sleep, stress management, protein-rich meals-are still the foundation. The drug just makes it possible.
Who Benefits Most? Who Should Avoid It?
GLP-1s work best for women with PCOS who have:
- BMI over 30
- Insulin resistance or prediabetes
- Failed to lose weight with diet, exercise, or metformin
- High testosterone or irregular periods
They’re not ideal for:
- Lean PCOS patients (BMI under 25)-they don’t show the same metabolic benefits
- People with a personal or family history of medullary thyroid cancer
- Those with severe gastrointestinal disorders
- Women who can’t afford the cost or tolerate side effects
And no, they’re not a replacement for birth control pills if you need contraception. GLP-1s don’t prevent pregnancy. You still need to manage that separately.
The Future: What’s Coming Next
Oral GLP-1s like Rybelsus are already here-no injections needed. They’re less effective than the injectables, but better for people who hate needles. In 2025, we’ll see the first results from the STEP-PCOS trial, a major 72-week study of 450 women on semaglutide. Early data shows 10.2% weight loss at 36 weeks.
Even more exciting? New drugs like retatrutide, which targets three hormones at once (GLP-1, GIP, and glucagon). Early trials show up to 24% weight loss. That’s bariatric surgery territory-without surgery.
By 2027, experts predict GLP-1s will be standard care for obese women with PCOS. But until then, access remains uneven. Insurance coverage in Australia is still rare. Public hospitals rarely offer them. You’ll likely need a private endocrinologist and out-of-pocket spending.
What to Do If You’re Considering GLP-1s
Here’s a practical checklist:
- Get tested for insulin resistance (fasting insulin, HOMA-IR) and HbA1c
- Try metformin and lifestyle changes first-give it 6 months
- If no progress, ask your doctor about GLP-1s
- Start low: 0.25 mg semaglutide weekly, increase slowly
- Pair with a diet rich in protein and fiber, low in sugar
- Keep taking metformin after stopping the GLP-1
- Track your periods, testosterone, and weight monthly
It’s not a quick fix. But for women who’ve spent years trying everything, it’s the first real chance at reclaiming their health.
Can GLP-1s help me get pregnant if I have PCOS?
Yes, indirectly. GLP-1s don’t directly cause ovulation, but by helping you lose weight and lowering testosterone, they often restore natural ovulation. In studies, 42% of women on liraglutide started ovulating again within 6 months-without fertility drugs. Weight loss of just 5-10% is often enough to restart your cycle.
How long does it take to see results with GLP-1s for PCOS?
Most women notice reduced hunger and slight weight loss within 2-4 weeks. Noticeable changes in body composition and energy levels show up by 8-12 weeks. Hormonal improvements-like lower testosterone and more regular periods-usually take 3-6 months. Full metabolic benefits, including liver fat reduction and improved insulin sensitivity, often take 6-12 months.
Are GLP-1s safe for long-term use in PCOS?
Current data shows they’re safe for up to 2 years in PCOS patients. Long-term studies beyond that are still ongoing. The biggest concern isn’t organ damage-it’s dependency. Weight tends to rebound if you stop. That’s why doctors recommend combining GLP-1s with metformin and lifestyle changes to maintain results after stopping.
Can I take GLP-1s if I’m not overweight but have PCOS?
Not usually. GLP-1s work best in women with insulin resistance and excess weight-typically BMI over 30. Lean PCOS patients (BMI under 25) rarely see the same metabolic benefits. For them, metformin, diet adjustments, and exercise are still the first-line options. GLP-1s aren’t proven to help with symptoms like acne or hair loss in lean women.
Do GLP-1s cause muscle loss?
Some weight loss from any drug can include muscle, but studies show GLP-1s preserve muscle better than dieting alone. In trials, up to 70% of the weight lost was fat, not muscle-especially when protein intake is kept high (1.6-2.2 g per kg of body weight) and strength training is included. That’s better than most other weight-loss methods.
Is there a cheaper alternative to Wegovy or Saxenda?
There’s no true generic version yet. But some patients use compounded liraglutide or semaglutide from licensed compounding pharmacies, which can cost 30-50% less. However, quality control varies. Another option is to ask your doctor about patient assistance programs from Novo Nordisk or Eli Lilly-they sometimes offer discounts or free medication for low-income patients.

Write a comment