By age 80, more than half of all people either have a cataract or have had cataract surgery. It’s not a rare condition-it’s a normal part of aging for many. The lens inside your eye, which normally stays clear like a camera lens, slowly becomes cloudy over time. This isn’t dirt or film on the surface-it’s a change inside the lens itself. Proteins clump together, scattering light instead of focusing it. The result? Colors look faded, glare from headlights or sunlight becomes blinding, and reading fine print feels impossible-even with glasses.
What Exactly Happens in the Eye?
Your eye’s natural lens sits behind the iris, the colored part of your eye. It’s made mostly of water and protein. As you get older, these proteins start to break down and stick together. Think of it like egg white turning opaque when you cook it. That cloudiness blocks light from reaching the retina, the light-sensitive tissue at the back of your eye. The more it clouds, the worse your vision gets. You might notice halos around lights, double vision in one eye, or needing brighter light just to read a menu. Glasses won’t fix this. No amount of stronger prescription will help because the problem isn’t the shape of your eye-it’s the lens itself.It’s not just about aging. Long-term sun exposure, smoking, diabetes, steroid use, and eye injuries can speed up the process. But for most people, it’s simply time. The National Eye Institute estimates 24.4 million Americans over 40 have cataracts. That number grows every year as the population ages.
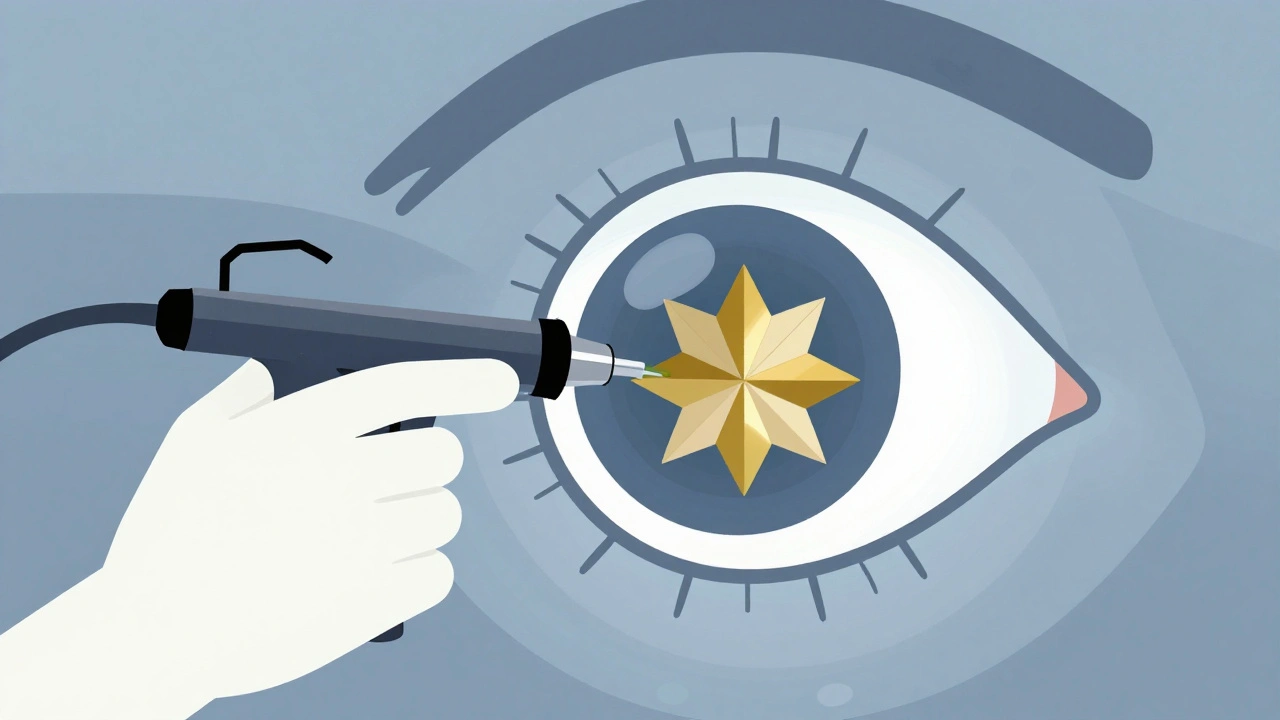
How Surgery Changed Everything
For centuries, the only option was “couching”-a crude method that pushed the cloudy lens out of the way without replacing it. Vision didn’t improve much, and complications were common. Everything changed in 1949 when Sir Harold Ridley implanted the first artificial lens, called an intraocular lens (IOL), in London. He realized the lens didn’t need to be removed and discarded-it could be replaced. That single idea revolutionized eye care.Today, cataract surgery is the most common surgical procedure in the U.S., with nearly 3.8 million operations performed each year. It’s done as an outpatient procedure, meaning you walk in and walk out the same day. Local anesthesia numbs the eye, and most people feel little to no pain. The surgery itself takes about 15 to 20 minutes. The standard technique now is called phacoemulsification. A tiny ultrasonic probe is inserted through a 2.2 to 2.8 millimeter incision in the cornea. It breaks up the cloudy lens into small pieces and suctions them out. Then, a foldable IOL is inserted into the empty lens capsule. It unfolds and settles into place, acting like your natural lens did before it clouded.
What to Expect After Surgery
You’ll leave the clinic with a protective shield over your eye. Your vision will likely be blurry at first. That’s normal. Many patients say things look “foggy” or “washed out” right after surgery. But improvement starts fast. Most people notice clearer vision within 1 to 3 days. Colors seem brighter-almost shocking. One patient on Reddit described it as “seeing HD for the first time in decades.”But full recovery takes longer. While some clinics say you’re healed in four weeks, others say it can take up to 10 weeks. Your brain needs time to adjust to the new lens. Depth perception can feel off. You might misjudge stairs or distances. That’s not the surgery failing-it’s your brain relearning how to interpret visual signals. Vision therapy, which involves simple eye movement exercises, can help speed up this adaptation. Some clinics recommend focusing on near and far objects several times a day, starting as early as 24 hours after surgery.
You’ll also need eye drops. Antibiotics like moxifloxacin prevent infection, and steroid drops like prednisolone acetate reduce inflammation. These are usually taken four times a day for the first week, then gradually tapered over four weeks. Skipping them-even if your eye feels fine-can lead to serious complications.
Will You Still Need Glasses?
This is one of the biggest surprises for patients. Even after surgery, you might still need glasses-especially for reading. That’s because most standard IOLs are monofocal. They’re designed to give you clear distance vision. Reading glasses become necessary again for close work. If you don’t mind wearing readers, this is a simple, reliable option.But there are alternatives. Premium IOLs can reduce or eliminate the need for glasses. Toric lenses correct astigmatism. Multifocal and trifocal lenses provide clear vision at multiple distances. Alcon’s PanOptix trifocal IOL, approved in 2019, gives 81% of patients complete freedom from glasses. Johnson & Johnson’s Tecnis Symfony offers extended depth of focus, with 89% of users achieving 20/25 vision or better at all distances. These lenses cost more-anywhere from $2,500 to $4,500 per eye out-of-pocket-because insurance typically only covers the basic monofocal option.
How Much Does It Cost?
Medicare and most private insurers cover the cost of standard cataract surgery and a basic monofocal IOL. That includes the surgeon’s fee, facility costs, and anesthesia. But if you want a premium lens, you pay the difference. A basic monofocal IOL might cost $1,500 to $3,000 per eye, but the insurance portion is only for the lowest-tier device. The extra cost for advanced lenses is entirely out-of-pocket. There’s no middle ground-you either go with the covered option or pay the full premium.Recovery Rules: What Not to Do
Your eye is healing. Even though you feel fine, you need to be careful. Avoid heavy lifting, bending over, or strenuous exercise for at least two weeks. Don’t rub your eye. Keep water out of it for the first week-no swimming, showers with direct spray, or washing your hair with your head tilted back. You can’t drive the day of surgery. Your doctor will clear you when your vision meets legal standards, usually within a few days to a week.
When Surgery Doesn’t Fully Restore Vision
Cataract surgery has a 98% satisfaction rate, and 95% of patients see major improvement. But it’s not magic. If you’ve had other eye problems-like glaucoma, macular degeneration, or diabetic retinopathy-your vision might not return to perfect. The cataract may have been hiding damage that can’t be fixed. In these cases, surgery still helps, but expectations need to be realistic. You’ll likely see better than before, but not necessarily 20/20.Another common issue is posterior capsule opacification (PCO). About 20 to 30% of patients develop a cloudy film behind the IOL months or years later. It’s not a recurrence of the cataract-it’s just scar tissue. It’s easily fixed with a quick, painless laser procedure called YAG capsulotomy. No incisions, no downtime. You’re back to normal in hours.
What’s Next for Cataract Treatment?
Technology keeps improving. New IOLs like Zeiss’s AT LISA tri 839MP, approved in early 2023, offer sharper intermediate vision-perfect for computer screens and dashboards. Researchers are testing accommodating IOLs that move like a natural lens, adjusting focus automatically. These are still in clinical trials but could be available within the next few years.The global market for cataract devices is projected to hit $6.32 billion by 2027. Aging populations and better technology are driving demand. But the core truth hasn’t changed: cataract surgery remains one of the safest, most effective procedures in all of medicine. A 2022 meta-analysis of 1.2 million surgeries found a 99.5% safety rate.
When to See a Doctor
If you’re having trouble with glare, colors seem dull, or reading is getting harder-even with glasses-it’s time for an eye exam. You don’t need to wait until you can’t see. Early diagnosis means you can plan surgery on your terms, not because you’re struggling. Most eye doctors recommend a comprehensive eye exam every one to two years after age 60, or more often if you have diabetes or a family history of eye disease.There’s no pill, drop, or diet that reverses cataracts. Surgery is the only proven solution. And it works-brilliantly.
Can cataracts come back after surgery?
No, cataracts cannot return because the natural lens is removed. But some patients develop posterior capsule opacification (PCO), a clouding of the membrane that holds the new lens. This happens in 20-30% of cases and is easily treated with a quick laser procedure called YAG capsulotomy. It takes less than five minutes and restores clear vision immediately.
Is cataract surgery painful?
Most patients feel little to no pain. The eye is numbed with topical anesthetic drops, and you may feel pressure or a slight tugging sensation during surgery. Afterward, your eye might feel scratchy, sticky, or mildly uncomfortable for a day or two. Over-the-counter pain relievers like acetaminophen are usually enough. Severe pain is rare and should be reported to your doctor right away.
How long does it take to recover from cataract surgery?
You’ll notice improved vision within 1 to 3 days, but full recovery takes 4 to 10 weeks. Your brain needs time to adapt to the new lens, especially if you’ve had cataracts for years. Vision therapy exercises can help. Avoid strenuous activity and water exposure for the first week. Most people return to normal daily activities within a few days, but full healing takes time.
Will I need glasses after cataract surgery?
It depends on the type of lens implanted. Standard monofocal IOLs correct distance vision, so you’ll likely still need reading glasses. Premium lenses-like multifocal or toric IOLs-are designed to reduce or eliminate the need for glasses. These cost more and aren’t covered by insurance, but many patients find the freedom from glasses worth the extra expense.
Can cataract surgery fix other vision problems?
Cataract surgery only removes the cloudy lens and replaces it with an artificial one. It doesn’t cure glaucoma, macular degeneration, or diabetic eye disease. If you have these conditions, your vision may improve after surgery but won’t return to perfect. Your doctor will assess your overall eye health before surgery to set realistic expectations.
Are there risks with cataract surgery?
Cataract surgery is very safe, with a 99.5% success rate. But like any surgery, risks exist. These include infection, bleeding, swelling, retinal detachment, or a dislocated lens implant. Complications occur in about 2-5% of cases. Most are treatable if caught early. Following post-op instructions-especially using eye drops and avoiding water and heavy lifting-significantly reduces risk.
How do I know if I’m a good candidate for surgery?
You’re a good candidate if cataracts are affecting your daily life-driving at night, reading, watching TV, or recognizing faces. Your eye doctor will measure your vision, check for other eye conditions, and discuss your lifestyle needs. There’s no need to wait until you’re “blind.” Surgery is recommended when vision loss interferes with your safety or quality of life.






Write a comment