When you live with Borderline Personality Disorder (BPD), emotions don’t just come and go-they crash over you like a wave with no shore. One moment you’re fine, the next you’re drowning in shame, rage, or despair. And when that happens, the urge to hurt yourself, lash out, or disappear can feel unstoppable. That’s where DBT skills come in-not as a magic fix, but as a set of real, practical tools you can use when everything else feels like it’s falling apart.
What DBT Actually Does for BPD
Dialectical Behavior Therapy, or DBT, wasn’t created in a lab. It was built by Dr. Marsha Linehan out of necessity. In the 1980s, she noticed that people with BPD who were suicidal kept falling through the cracks of traditional therapy. They needed more than talk. They needed structure. They needed skills they could hold onto when their emotions were screaming. DBT works because it doesn’t fight your feelings. It doesn’t tell you to “calm down.” Instead, it teaches you how to ride the wave without drowning. It combines two opposing ideas: accepting yourself exactly as you are right now, while also believing you can change. That’s the “dialectic” part. And it’s why DBT is the most researched treatment for BPD. Studies show it cuts self-harm by nearly half and reduces suicide attempts by 50% over a year. The core of DBT isn’t therapy alone. It’s a four-part skill system designed to replace chaos with control. These aren’t abstract ideas-they’re actions you can take today, even when you’re shaking or crying.The Four Skill Modules: Your Emotional Toolkit
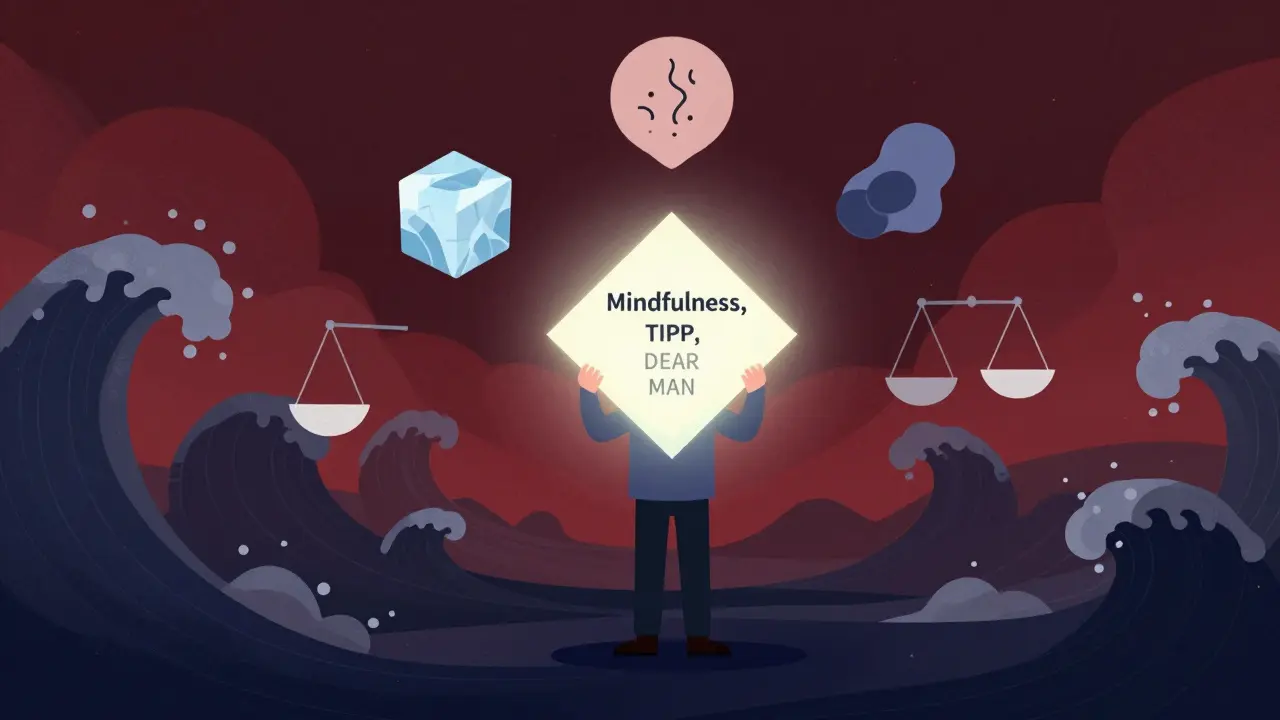
DBT breaks down emotional survival into four skill areas. Each one targets a different part of the crisis cycle. You don’t need to master them all at once. Start with one. Build from there.Mindfulness: Grounding Yourself in the Now
Mindfulness in DBT isn’t about meditation for hours. It’s about noticing what’s happening without getting lost in it. The “what” skills are simple: observe your thoughts, describe your feelings out loud, and participate fully in whatever you’re doing-even if it’s just washing dishes. The “how” skills are even more practical: do it non-judgmentally (no “I’m such a failure” thoughts), one-mindfully (focus on one thing at a time), and effectively (what works, not what feels fair). People who practice this for just eight weeks report a 32% increase in emotional control. That’s not hype. That’s science. When you’re in the middle of a meltdown, mindfulness doesn’t erase the pain. But it gives you space between the feeling and the reaction. And that space? That’s where you make a different choice.Distress Tolerance: Surviving the Unsurvivable
This is where DBT shines. When you’re in crisis-when thoughts of self-harm are loud, when you feel like you can’t take another minute-distress tolerance gives you tools to get through it without breaking. One of the most powerful sets is TIPP:- Temperature: Splash ice water on your face. Or hold an ice cube in your hand. The shock interrupts the panic response.
- Intense exercise: Run in place for 60 seconds. Jump jacks. Anything that gets your heart racing.
- Paced breathing: Breathe in for 4 counts, hold for 4, out for 6. Repeat. This calms your nervous system fast.
- Paired muscle relaxation: Tense your fists, shoulders, legs-hold for 5 seconds. Then release. Feel the difference.
- Imagine a safe place
- Meaning: Ask yourself, “What’s the point of enduring this?”
- Pray: If you’re spiritual, say a prayer or a calming phrase
- Relaxation: Listen to music, take a warm shower
- One thing in the moment: Focus on your breath, the texture of your blanket, the sound of rain
- Vacation: Give yourself permission to pause-even for 10 minutes
- Encouragement: Say out loud, “I’m doing my best. That’s enough.”
Emotion Regulation: Understanding Your Feelings
BPD isn’t about having too many emotions. It’s about having emotions that hit like a freight train-and no brakes. The PLEASE skill helps you build a foundation so your emotions don’t spiral out of control:- Physical illness: Treat any medical issues. Pain and fatigue make emotions worse.
- Level of eating: Don’t skip meals. Blood sugar crashes = mood crashes.
- Evade mood-altering drugs: Alcohol, weed, stimulants-these make BPD symptoms worse.
- Abalanced sleep: Aim for 7-8 hours. Sleep deprivation = emotional chaos.
- Exercise: Even a 15-minute walk helps regulate your nervous system.
Interpersonal Effectiveness: Holding Boundaries Without Losing Relationships
People with BPD often live in a cycle of intense connection followed by sudden rejection. You crave closeness, but fear abandonment. So you push people away-or beg them not to leave. DEAR MAN helps you ask for what you need without blowing up:- Describe the situation
- Express how you feel
- Assert your request
- Reinforce why it matters
- Stay mindful
- Appear confident
- Negotiate if needed
- Gentle: Don’t attack, don’t blame
- Interest: Listen more than you speak
- Validate: Say, “I get why you’d feel that way.”
- Easy manner: Smile. Lighten your tone.
- Fair: Be fair to others, and to yourself
- No apologies: Don’t apologize for having needs
- Stick to values: Don’t compromise your core beliefs
- Truthful: Don’t lie to keep peace
Crisis Planning: What to Do When Everything Falls Apart
A crisis plan isn’t a nice-to-have. It’s your lifeline. And DBT gives you the structure to build one. Start with STOP:- Stop: Freeze. Don’t react.
- Take a step back: Breathe. Count to ten.
- Observe: What’s happening in your body? What thoughts are looping?
- Proceed mindfully: Choose your next move-not your emotion.
- Emergency contacts (therapist, crisis line, trusted friend)
- Skills you’ve practiced (TIPP, IMPROVE, etc.)
- Places you can go (park, library, quiet room)
- Things you can do (listen to music, walk, write)
- What to say if you call for help

How DBT Compares to Other Treatments
There are other therapies for BPD. But DBT stands out. Mentalization-Based Therapy (MBT) helps you understand others’ minds-but doesn’t give you concrete tools to stop self-harm. Schema Therapy digs deep into childhood wounds-but takes years. STEPPS is a group program that helps with symptoms, but doesn’t handle acute crises like DBT does. DBT’s edge? It’s the only one with phone coaching. That means, at 2 a.m., when you’re terrified and alone, you can call your therapist and get real-time help applying TIPP or STOP. No waiting. No judgment. Just support. But DBT isn’t easy. It’s 6 to 12 months of weekly individual therapy, two-hour group sessions, and homework. It’s hard to stay consistent. One in three people drop out before finishing. Still, the ones who stick with it? They’re the ones who stop going to the ER. Who keep their jobs. Who rebuild relationships. Who survive.Real Stories: What Works and What Doesn’t
Reddit’s r/DBT community has over 100,000 members. Their stories are raw, honest, and full of hope. One user wrote: “I used DEAR MAN to tell my partner I needed space after a fight-not to leave, but to calm down. He listened. We didn’t break up.” Another said: “I kept the PLEASE worksheet on my fridge. Every morning, I checked off sleep, food, exercise. For the first time in years, I didn’t self-harm.” But others say: “The worksheets felt overwhelming.” “I couldn’t do the homework.” “My therapist didn’t get it.” That’s the reality. DBT works-but only if it’s done right. And only if you’re willing to show up, even when it’s hard.
Getting Started: What You Need to Know
If you’re thinking about DBT:- Find a therapist certified by the Linehan Board of Certification. There are only about 1,800 worldwide.
- Ask if they offer the full program: individual therapy, skills group, phone coaching, and therapist consultation team.
- Start with the distress tolerance skills. They’re the most urgent.
- Use the Dialectical Behavior Therapy Skills Workbook-it’s clear, practical, and full of worksheets.
- Don’t wait until you’re in crisis. Start learning before you need it.
The Long Game
DBT doesn’t promise you’ll never feel pain again. It promises you won’t have to destroy yourself to survive it. The skills take time. You’ll forget them. You’ll mess up. You’ll feel like giving up. But every time you use TIPP instead of cutting. Every time you say “I need space” instead of screaming. Every time you breathe through the rage instead of running away-you’re rewiring your brain. This isn’t about becoming someone else. It’s about becoming more of yourself. Calmer. Stronger. More in control. And that? That’s worth every hard day.Can DBT help if I don’t self-harm?
Yes. While DBT was originally designed for people with suicidal behaviors, its skills work for anyone struggling with emotional overwhelm, intense relationships, or impulsivity. Many people use DBT to manage anxiety, anger, or mood swings-even without a BPD diagnosis. The core skills-mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness-are useful for anyone trying to handle strong emotions better.
How long does it take to see results from DBT?
Most people notice small changes within 2-4 months, like fewer emotional outbursts or better sleep. Major improvements-like reduced self-harm or improved relationships-usually take 6-12 months of consistent practice. It’s not quick, but the changes are lasting. The key is showing up, even on days when you don’t feel like it.
Do I need to do group therapy for DBT to work?
Group skills training is a core part of standard DBT, but not the only path. Some people work with individual DBT therapists who teach the skills one-on-one. However, group settings offer peer support and accountability, which many find essential. If group therapy isn’t available, look for a therapist trained in individual DBT adaptations. The skills still work-but you might miss out on the shared learning experience.
Can I use DBT skills on my own without a therapist?
You can learn and apply DBT skills independently using workbooks, apps, or online videos. Many people do. But DBT was designed as a full treatment system-with therapist support, phone coaching, and team consultation. Without a therapist, you might miss feedback, struggle to stay consistent, or misapply skills during intense crises. If you’re in severe distress, working with a trained DBT therapist is strongly recommended.
Is DBT covered by insurance?
In the U.S., most private insurers and Medicare cover DBT when delivered by certified providers, typically for 12-20 sessions per year. Coverage varies by plan and state. In Australia, some private health funds cover DBT under mental health rebates. Always check with your provider and ask if the therapist is certified by the Linehan Board of Certification-this often affects reimbursement.
What if I can’t find a DBT therapist near me?
Telehealth has made DBT more accessible than ever. Many certified therapists offer sessions online. Look for providers through the Linehan Institute’s directory or Psychology Today’s therapist filter (search “DBT”). If in-person options are limited, combine self-guided learning with occasional check-ins with a therapist. Even one session a month can help you stay on track. Don’t wait for the perfect setup-start where you are.
Next Steps: What to Do Today
If you’re reading this and thinking, “This could help me,” here’s what to do right now:- Write down one emotion you’ve struggled with this week.
- Choose one DBT skill from this article that might help with it.
- Practice it once today-even if it feels silly.
- Text a friend: “I’m trying something new to handle my emotions. Want to check in?”






Write a comment