Snoring isn’t just annoying-it can be a sign of something deeper. If you’ve tried everything from nasal strips to sleeping on your side and still wake up to the sound of your own breathing, you’re not alone. About 34.5 million American adults snore regularly, and for many, the solution isn’t a CPAP machine. Enter oral appliance therapy-specifically, mandibular advancement devices (MADs). These small, custom-fitted devices reposition your lower jaw slightly forward to keep your airway open while you sleep. No tubes. No masks. Just a quiet night and a partner who can finally sleep.
How Mandibular Advancement Devices Actually Work
MADs don’t just push your jaw forward-they change the physics of your airway. When you sleep, your tongue and soft tissues relax and can collapse into the back of your throat. This narrowing causes vibrations-the snoring sound. A mandibular advancement device gently pulls your lower jaw forward by 3 to 12 millimeters. That small movement tugs the base of your tongue and other tissues forward too, opening up space where air can flow freely.
It’s not guesswork. Studies show that 75% of maximum jaw advancement (usually around 8-10mm) gives the best results. That’s why custom devices, made by dentists using dental impressions or digital scans, work far better than over-the-counter boil-and-bite versions. A 2015 meta-analysis found custom MADs reduced snoring by 72.3%, while non-custom ones only managed 48.6%. The difference? Precision. Custom devices fit your teeth exactly and allow fine-tuning, often in 0.5mm increments, so you can find the sweet spot between comfort and effectiveness.
Who Benefits Most From This Treatment?
Mandibular advancement isn’t a magic fix for everyone. It works best for people with mild to moderate obstructive sleep apnea-or even just primary snoring without apnea. If your snoring is positional (worse when you sleep on your back), MADs can be especially helpful. They’re also ideal for people who travel often, hate the noise and bulk of CPAP machines, or find them unbearable.
But there are limits. If you have severe airway collapse (Mallampati Class IV), or if you’ve lost most of your back teeth, MADs won’t work. About 12.7% of snorers are ruled out because of dental or jaw issues. And if you have TMJ disorder, you need to be evaluated carefully-some devices can worsen jaw pain.
Patients with no teeth, severe gum disease, or only a few remaining teeth on one side of the mouth are generally not candidates. Your dentist will check your bite, jaw movement, and tooth health before even considering a device.
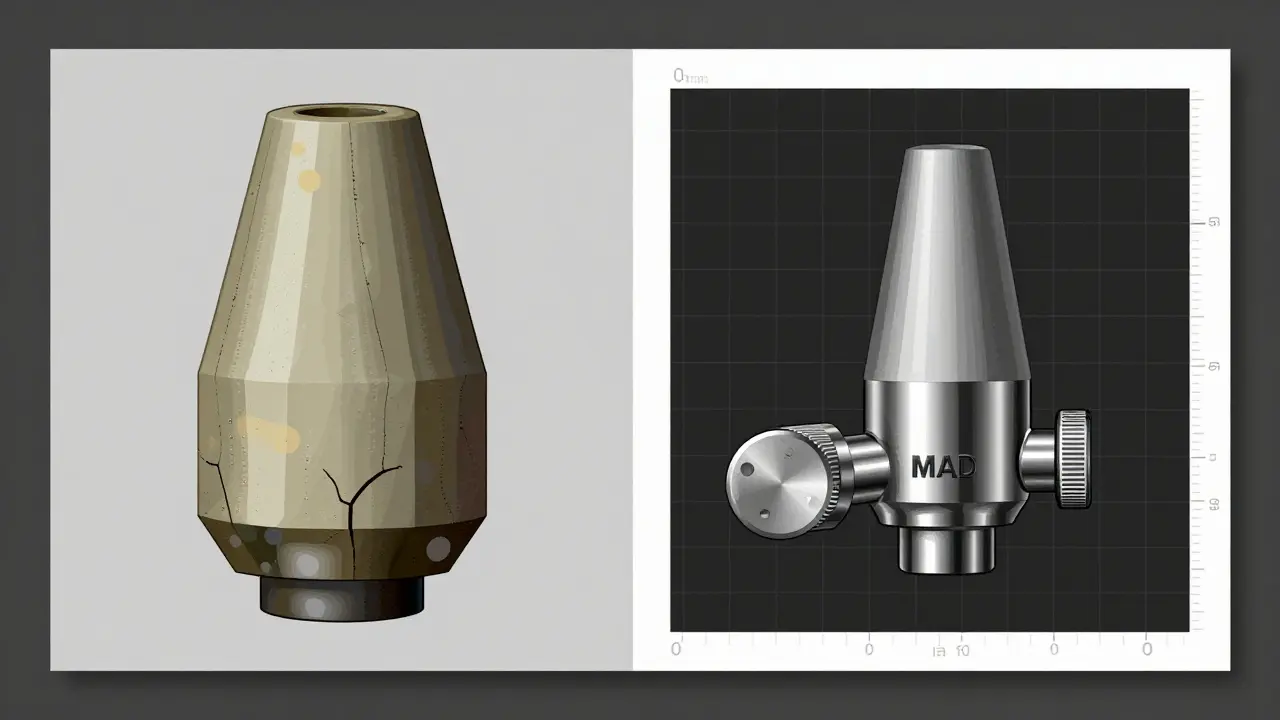
Custom vs. Over-the-Counter: The Real Difference
You’ll see ads for $99 snoring mouthpieces online. They look convincing. But here’s the truth: they’re not the same as what your dentist prescribes.
Over-the-counter MADs are made from soft thermoplastic that you soften in hot water and bite into. They’re one-size-fits-none. Most only advance the jaw 3-5mm-too little for many people. They also wear out quickly, don’t adjust well, and can cause uneven pressure on your teeth.
Prescription MADs, like the SomnoDent MAS or TAP 3, are made from durable acrylic with titanium connectors. They’re designed for long-term use, last 3-5 years, and allow precise adjustments. The cost? $1,800 to $2,500. That’s expensive, but it’s a medical device, not a gadget. And unlike OTC versions, they’re built to meet FDA Class II standards and have been tested in clinical trials.
Here’s what the numbers say: custom MADs reduce snoring by 65-75% in compliant users. OTC devices? More like 20-40%. If your goal is real, lasting relief-not just a temporary fix-custom is the only option that delivers consistent results.

What to Expect When You Start Using One
Getting a MAD isn’t a one-time visit. It’s a process.
First, you’ll need a sleep study-either at a clinic or at home-to confirm you don’t have severe sleep apnea. If you do, CPAP is still the gold standard. But if your apnea is mild or you just snore, then a dental sleep specialist will take impressions of your teeth. Digital scans are now faster and more accurate than traditional molds.
Once your device is ready, you’ll start wearing it nightly. The first week? Expect some discomfort. Jaw soreness, increased saliva, and even minor tooth sensitivity are common. Most people adapt within 10-14 days. Your dentist will likely recommend wearing it for an hour or two during the day to get used to the feel before sleeping with it.
Then comes titration-adjusting the device. You’ll increase the jaw advancement by 1mm every 3-5 days until snoring stops or you hit your comfort limit. This can take 4-6 weeks. Some devices have built-in dials. Others require a visit to the dentist to make small adjustments. Don’t rush this step. Pushing too far too fast can cause lasting jaw problems.
Follow-up appointments are non-negotiable. You’ll need check-ups every 6 months to monitor your bite and jaw joint. Long-term use can change your tooth alignment-about 25% of users develop minor occlusal shifts that may need orthodontic correction later.
Side Effects and Risks: The Hidden Costs
Yes, MADs work. But they’re not risk-free.
The most common side effect? Morning jaw pain. About 68% of users report it in the first few weeks. Most of it fades as you adjust. Excessive drooling? That happens to 43% of people-especially early on. It usually improves after a month.
The bigger concern is long-term dental changes. A 2023 study from SUNY found that 25% of users who wore MADs for 5+ years developed irreversible changes in their bite. Some needed crowns, braces, or even extractions. That’s why regular dental visits are critical. Catching changes early can prevent major damage.
Also, MADs don’t cure sleep apnea-they manage it. If you stop wearing the device, snoring typically returns within 48 hours. That means lifelong use. And if you’re not consistent, the benefits vanish.
How MADs Compare to Other Treatments
Let’s put MADs in context.
- CPAP: More effective-85-95% snoring elimination. But 55% of users quit within a year because of discomfort, noise, or claustrophobia.
- Positional Therapy: Sleeping on your side helps, but only cuts snoring by 35-45%. Hard to maintain.
- Nasal Dilators: Reduce snoring by 20-30%. Often useless for people with throat-based snoring.
- Surgery (UPPP): Can help, but recovery is long, success rates vary, and complications are common.
MADs sit in the middle: less effective than CPAP, but far more tolerable. Adherence rates? 76.4% after 12 months for MADs versus 45.2% for CPAP. That’s the real advantage. If you don’t use it, it doesn’t work. MADs win on compliance.
Cost, Insurance, and Getting Started
The out-of-pocket cost for a custom MAD is $1,800-$2,500. That’s steep. But here’s the twist: only 38% of U.S. private insurance plans cover them. Medicare rarely does. Some HSA or FSA accounts will let you use pre-tax dollars, though.
That’s why many people go the OTC route. But as we’ve seen, they rarely deliver. If you’re serious about stopping snoring, spending the money on a custom device is the only way to get reliable, lasting results.
To start, talk to your primary care doctor about a sleep study. If you’re a candidate, they’ll refer you to a dentist trained in dental sleep medicine. Look for someone certified by the American Academy of Dental Sleep Medicine. Don’t just go to any general dentist-they need special training to fit these devices properly.
What’s Next for Oral Appliance Therapy?
The field is evolving fast. In 2023, the FDA cleared the SomnoDent EVO 3-the first MAD with built-in sensors that track your jaw position and snoring levels via a smartphone app. Soon, AI will help predict the ideal jaw advancement for your anatomy. Researchers are even exploring genetic markers to determine who will respond best to MADs.
By 2027, experts predict MAD adoption will grow 40%. As more people reject CPAP and demand quieter, simpler solutions, these devices will become mainstream. But they’re not for everyone. They require commitment, dental health, and patience.
If you’re tired of being the reason your partner sleeps in another room-if you’re ready to try something that actually works without a mask or hose-then oral appliance therapy might be your answer. Just make sure you do it right: get evaluated, get custom, and get monitored.
Are mandibular advancement devices safe for long-term use?
Yes, when used correctly and monitored by a dental sleep specialist. Long-term use (5+ years) can cause minor changes in tooth alignment or jaw position in about 25% of users. Regular check-ups every 6 months help catch these early. Most users experience no serious issues if they follow follow-up protocols and avoid over-advancing the jaw.
Can I use an over-the-counter MAD instead of a custom one?
You can, but you’ll get significantly less benefit. OTC devices reduce snoring by only 20-48%, while custom MADs achieve 65-75%. They’re also less durable, harder to adjust, and more likely to cause uneven pressure on your teeth. If you’re serious about stopping snoring, custom is the only option with proven, reliable results.
Do I need a sleep study before getting a MAD?
Yes. A sleep study (home or clinic-based) is required to rule out moderate-to-severe obstructive sleep apnea. MADs are not recommended for severe OSA-CPAP is still the standard. Even if you think you just snore, undiagnosed apnea can be dangerous. Your doctor or dentist will need those results before proceeding.
How long does it take to get used to wearing a MAD?
Most people adapt within 10-14 days. Initial discomfort-jaw soreness, excess saliva, or pressure on teeth-is normal. Many dentists recommend wearing the device for 1-2 hours during the day to get used to the feel before sleeping with it. Don’t rush the adjustment. Gradual titration (increasing jaw position slowly) reduces side effects.
Will my insurance cover a mandibular advancement device?
Sometimes. Only about 38% of private insurance plans in the U.S. cover custom MADs. Medicare rarely does. Some HSA or FSA accounts allow you to pay with pre-tax dollars. Always check with your insurer before proceeding. Your dentist’s office can often help you submit a pre-authorization request.
What happens if I stop using my MAD?
Snoring typically returns within 48 hours. MADs don’t cure the underlying cause-they manage it by keeping your airway open. If you stop wearing the device, your jaw and tongue return to their relaxed position, and airway narrowing resumes. Consistency is key. This isn’t a one-time fix-it’s a long-term solution.
If you’ve tried everything else and still can’t sleep through the night, mandibular advancement therapy offers a real, evidence-based alternative. It’s not perfect. It’s not cheap. But for many, it’s the only thing that finally lets them-and their partner-get a good night’s rest.




Write a comment