Malaria Research Timeline Explorer
Select a year to see key events in malaria research.
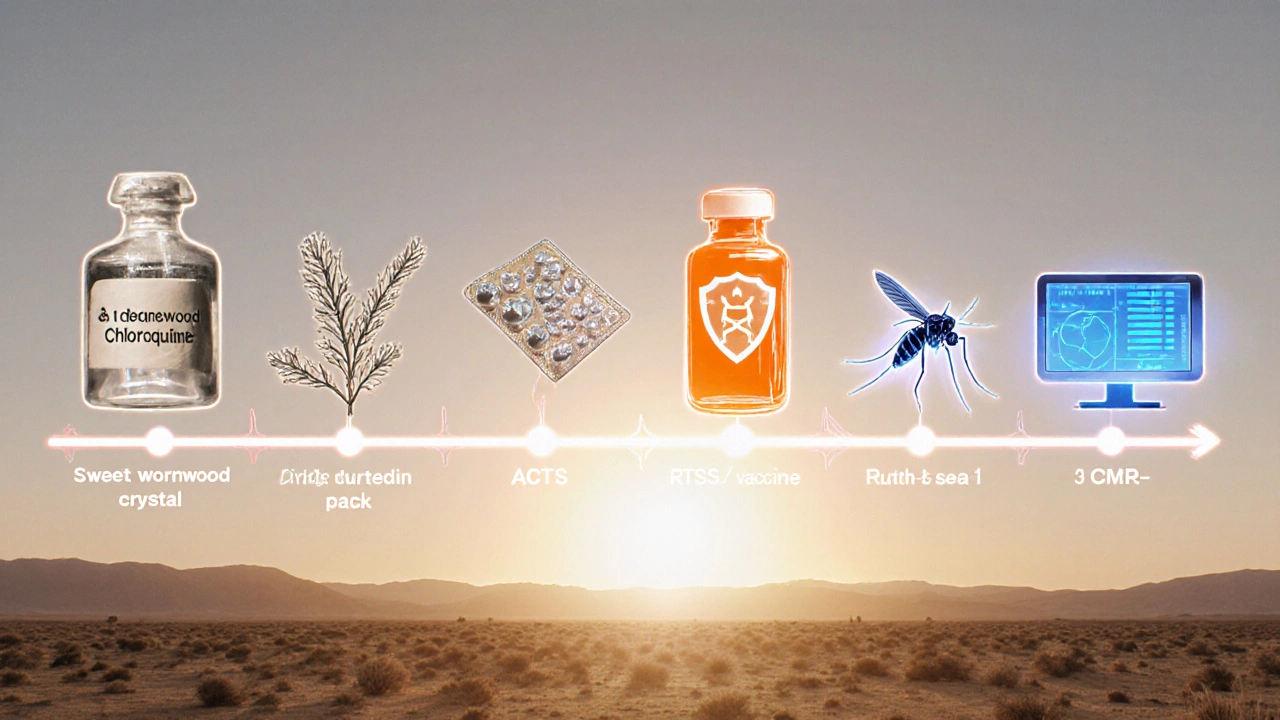
Key Milestones in Malaria Research
Chloroquine Introduced
Quickly became the frontline treatment for malaria.
Widespread Resistance Emerges
Resistance develops in Southeast Asia, prompting search for new treatments.
Artemisinin Isolated
Chinese scientists isolate artemisinin from sweet wormwood, saving millions of lives.
Combination Therapies
ACTs (Artemisinin-based Combination Therapies) pair artemisinin with partner drugs to delay resistance.
Gene Drive Trials Begin
First semi-field trials in Burkina Faso release modified Anopheles that cannot transmit the parasite.
Model Predictions
Ecological modeling predicts a 70% drop in transmission after three generations.
Malaria still kills over 600,000 people a year, most of them children under five. The disease’s stubborn grip isn’t just a matter of tropical climate or poverty; it’s a moving target that evolves faster than many health programs can keep up. That’s why malaria research matters more than any single intervention - it supplies the data, tools, and breakthroughs that let us stay ahead of the parasite, the mosquito, and the social factors that keep the cycle turning.
What is Malaria? The Biology Behind the Outbreak
Malaria is a mosquito‑borne disease caused by single‑celled parasites of the genus Plasmodium. The most lethal species, P. falciparum, multiplies inside human red blood cells and triggers fever, chills, and, in severe cases, organ failure. The parasite’s life cycle depends on the Anopheles mosquito, which picks up gametocytes from an infected human, lets them develop inside its gut, and then injects sporozoites when it bites another person.
Understanding this biology is the first step for any research program-without a clear map of how the parasite moves, it’s impossible to interrupt it effectively.
From Chloroquine to Artemisinin: A Brief History of Drug Discovery
- 1929 - Chloroquine introduced; quickly became the frontline treatment.
- 1970s - Widespread resistance emerges in Southeast Asia, forcing a search for new compounds.
- 1972 - Chinese scientists isolate artemisinin from sweet wormwood, a breakthrough that saved millions of lives.
- 2000s - Combination therapies (ACTs) pair artemisinin with partner drugs to delay resistance.
Each drug milestone stemmed from laboratory work, field trials, and the continual monitoring of parasite sensitivity. Today, artemisinin‑based combination therapies (ACTs) are the gold standard, but research shows resistance is creeping into the Greater Mekong Subregion, prompting urgent calls for the next generation of medicines.
Vaccines Rise: The Story of RTS,S
RTS,S is the world’s first approved malaria vaccine, targeting the circumsporozoite protein of P. falciparum. Clinical trials spanning three continents showed a 30% reduction in severe malaria among African children, enough for the WHO to endorse pilot implementations in Ghana, Kenya, and Malawi.
Research didn’t stop at the trial stage. Post‑licensure studies are measuring real‑world effectiveness, looking at how seasonal delivery, booster doses, and co‑administration with other vaccines affect outcomes. Early data suggest that when combined with insecticide‑treated nets, RTS,S can cut overall case numbers by up to 45% in high‑transmission zones.
Gene Drive and CRISPR: Re‑Engineering Mosquitoes
Gene‑drive technology uses CRISPR to bias inheritance of a specific gene, spreading it through a population faster than normal Mendelian laws. Scientists are designing drives that either render mosquitoes unable to host Plasmodium or skew sex ratios toward males, collapsing local mosquito populations.
- 2022 - First semi‑field trials in Burkina Faso release modified Anopheles that cannot transmit the parasite.
- 2024 - Ecological modelling predicts a 70% drop in transmission after three generations, if community acceptance is secured.
These advances are still experimental, but the rigorous risk assessments and community‑engagement studies being conducted now will determine whether gene drives become a mainstream tool.

Surveillance, Diagnostics, and WHO Guidelines
Accurate case detection is a research‑driven necessity. Rapid diagnostic tests (RDTs) using histidine‑rich protein 2 (HRP2) antigens have become the backbone of field surveillance, but recent reports of HRP2‑negative parasites in the Amazon show that diagnostic research must keep pace.
The World Health Organization (WHO) publishes the Global Malaria Programme guidelines that integrate drug policy, vector control, and surveillance data into a unified strategy. Each annual revision reflects new evidence from clinical trials, entomological studies, and economic analyses, ensuring national malaria control programs operate on the latest science.
Funding and Global Partnerships
Large‑scale research requires deep pockets. The Bill & Melinda Gates Foundation has pledged $1.5billion for malaria innovation since 2000, supporting everything from vaccine pipelines to gene‑drive modeling. The US President’s Malaria Initiative (PMI) contributes over $1billion annually to procurement, training, and research coordination. These funders often require grantees to publish open‑access data, creating a virtuous cycle where findings fuel new projects worldwide.
Key Challenges: Resistance, Climate, and Equity
- Drug resistance: Molecular studies show mutations in the kelch13 gene reduce artemisinin efficacy, demanding new drug candidates.
- Insecticide resistance: Over 80% of African Anopheles populations now survive pyrethroid exposure, pushing research toward next‑generation nets treated with chlorfenapyr or pyriproxyfen.
- Climate change: Rising temperatures expand the geographic range of Anopheles vectors into highland regions, as climate‑modeling research predicts.
- Health‑system gaps: Rural clinics often lack trained personnel to interpret RDTs, a problem being addressed by mobile‑health research platforms.
Each obstacle is a research question waiting for a data‑driven answer.
Comparison of Core Malaria‑Control Strategies
| Intervention | Primary Mechanism | Typical Efficacy | Deployment Stage (2025) | Main Challenges |
|---|---|---|---|---|
| RTS,S Vaccine | Induces antibodies against sporozoite surface protein | ~30% reduction in severe cases | Pilot rollout in 3 African countries | Need for multiple booster doses; limited coverage |
| ACTs (Artemisinin‑based Combination Therapies) | Rapid parasite clearance + partner‑drug protection | 90‑95% cure rate when adherence is good | Standard first‑line treatment worldwide | Emerging kelch13 resistance in SE Asia |
| Insecticide‑Treated Nets (ITNs) | Physical barrier + insecticide killing mosquitoes | ~50% reduction in child mortality | Universal coverage targets met in 70% of endemic households | Pyrethroid resistance; durability issues |
| Gene‑Drive Mosquitoes | Genetic alteration to block parasite development | Modelled 60‑70% transmission drop | Controlled field trials, regulatory review pending | Ethical concerns; ecological risk assessments |
Practical Checklist for Policymakers and Program Managers
- Verify current drug‑resistance maps; allocate ACTs accordingly.
- Ensure >80% of at‑risk households own and correctly use ITNs; schedule net replacement every three years.
- Integrate RTS,S vaccination into existing child‑immunization schedules where pilot data show impact.
- Invest in local laboratory capacity for molecular surveillance of kelch13 and HRP2 deletions.
- Engage community leaders early when considering gene‑drive releases; conduct transparent risk‑benefit workshops.
- Leverage mobile‑health tools to capture real‑time case data, feeding it back into WHO’s Global Malaria Programme updates.
Following these steps keeps the research loop closed: data informs action, action generates data, and the cycle repeats.

Frequently Asked Questions
Why is a malaria vaccine needed when we have drugs?
Drugs treat infection after it occurs, but a vaccine can prevent the parasite from establishing itself in the first place. In high‑transmission settings, reducing new infections cuts the overall burden faster than treatment alone, especially when drug resistance threatens existing therapies.
How does gene‑drive technology differ from traditional insecticide use?
Traditional insecticides kill mosquitoes on contact, creating selection pressure that breeds resistance. Gene drives edit the mosquito’s genome so that a protective trait (e.g., inability to host Plasmodium) spreads through the population automatically, reducing reliance on chemicals.
What are the biggest obstacles to scaling up RTS,S vaccination?
Key hurdles include the need for four doses (three primary plus a booster), cold‑chain requirements in remote areas, and relatively modest efficacy compared with other childhood vaccines. Ongoing research aims to improve formulation and simplify the schedule.
Can climate change reverse the gains made in malaria control?
Rising temperatures can expand the habitable range of Anopheles mosquitoes, introducing malaria to previously low‑risk highland zones. Models predict a potential 10‑15% increase in global cases by 2050 if no adaptive measures are taken, making climate‑focused research urgent.
How do funding agencies decide which malaria projects to support?
They look for evidence of scientific rigor, clear pathways to impact, and alignment with WHO’s strategic pillars. Proposals that include data‑sharing plans and capacity‑building components receive higher scores, ensuring results benefit the broader research community.






Write a comment