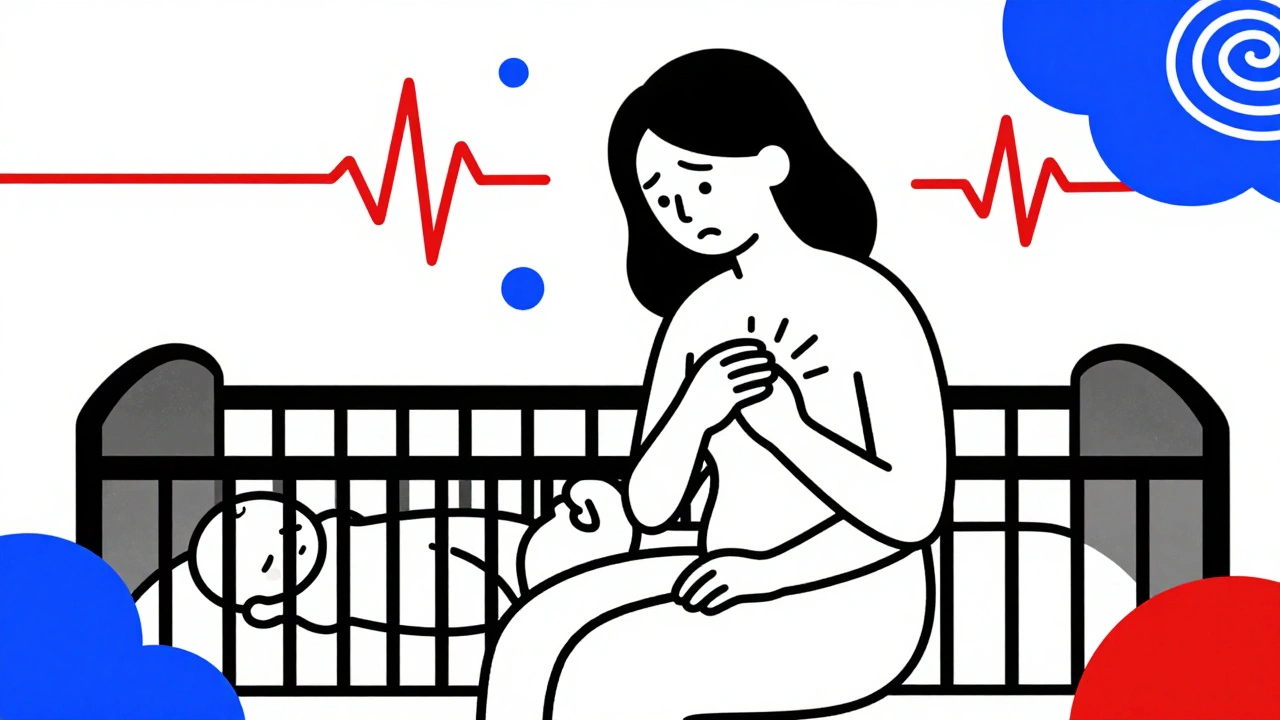
One in five new mothers experiences postpartum anxiety - not just stress, not just tiredness, but a deep, persistent wave of worry that doesn’t fade with sleep or time. It’s not the baby blues. Those pass in a couple of weeks. This lingers. It keeps you awake when the baby is sleeping. It makes your heart race for no reason. It turns everyday moments - a cry, a missed feeding, a dirty diaper - into catastrophes. And yet, most women don’t know what’s happening. They think they’re just failing at motherhood.
What Postpartum Anxiety Really Feels Like
Postpartum anxiety isn’t about being a nervous parent. It’s a clinical condition that can start anytime in the first year after birth - or even after adoption. The symptoms are physical, emotional, and mental, and they don’t match what most people expect from a new mom.
You might feel your chest tighten, your breath shorten, or your stomach churn - even when everything seems fine. Sixty-two percent of women with this condition report racing heartbeats. Nearly half feel nauseous. Four in ten lose their appetite. These aren’t side effects of sleep deprivation. They’re signs of an overactive nervous system stuck in fight-or-flight mode.
Then there’s the mental loop: endless worry about the baby’s breathing, getting sick, falling, choking. Intrusive thoughts - like imagining something terrible happening - show up in nearly 70% of cases. These aren’t signs you’re a bad mother. They’re symptoms of anxiety. The brain, under stress, starts scanning for danger everywhere - even where there is none.
And unlike depression, which pulls you down into sadness, anxiety pushes you into overdrive. You might be irritable, snapping at partners or family. You might feel guilty for not feeling joyful. You might hide it because you think you should be happy. But this isn’t weakness. It’s biology.
How It’s Different From Baby Blues and Postpartum Depression
Many women assume any emotional struggle after birth is just the baby blues. But those usually fade by day 14. If you’re still feeling overwhelmed, panicked, or consumed by worry after two weeks, it’s something else.
Postpartum depression often shows up as numbness, hopelessness, or crying for no reason. Postpartum anxiety is different. It’s the opposite: a constant hum of dread. Eighty-five percent of those with anxiety report obsessive worry, compared to just 31% with depression alone. Physical symptoms like heart palpitations and nausea are also far more common in anxiety - 76% versus 43% in depression.
And here’s the catch: nearly half of women with postpartum anxiety also have depression. The two often travel together. That’s why screening tools need to catch both. If you’re only looking for sadness, you’ll miss the panic.
Screening: The Tools That Actually Work
The Edinburgh Postnatal Depression Scale (EPDS) is the most widely used tool in clinics. But it wasn’t built for anxiety. Still, it’s useful. Women with no mental health issues score around 6.2. Those with anxiety-only score about 9.8. Depression-only? Around 11.3. When both are present, scores jump to 14.7.
But here’s the problem: EPDS catches 92% of anxiety cases - but only 68% of the time, it’s right. That means nearly a third of the time, it flags anxiety when it’s not there. That’s why many providers now use the GAD-7, a seven-question scale made specifically for generalized anxiety. It’s more accurate: 89% sensitive, 84% specific.
And now, in 2023, the EPDS has been updated with a new anxiety subscale. In a study of over 1,200 women, this version correctly identified anxiety in 89% of cases - a big step forward.
Still, no blood test or scan can confirm this. Diagnosis is based on your story - what you feel, how long it’s lasted, and how much it’s disrupting your life. A doctor doesn’t need a machine. They need to listen.

Why So Many Cases Go Undetected
Sixty-three percent of women with postpartum anxiety are told they’re just “overwhelmed.” That’s not just misleading - it’s dangerous. On average, it takes 11.3 weeks before someone gets the right diagnosis. That’s nearly three months of suffering in silence.
Why? Because the symptoms look like parenting. You’re tired. You’re juggling. You’re worried. Who wouldn’t be? But when the worry is constant, irrational, and physically painful - it’s not normal. And it’s not something you should push through.
Even doctors sometimes miss it. A 2023 survey showed that while 67% of U.S. obstetric practices now screen for postpartum mental health, many still only ask about sadness. Anxiety doesn’t scream. It whispers. And too many clinicians aren’t trained to hear it.
How It’s Treated - Step by Step
Treatment isn’t one-size-fits-all. It’s based on severity, measured mostly by EPDS scores.
Mild cases (EPDS 10-12): Therapy and lifestyle changes are often enough. Daily 30-minute walks reduce anxiety scores by 28% in eight weeks. Yoga helps even more - 33% symptom reduction in clinical trials. Mindfulness practices, like five minutes of breathing each morning, can cut symptoms by 41% in just two weeks.
Moderate cases (EPDS 13-14): Cognitive Behavioral Therapy (CBT) is the gold standard. Twelve to sixteen structured sessions help 57% of women significantly reduce symptoms. CBT teaches you to challenge the thoughts that fuel panic - like “If the baby cries, something’s wrong” - and replace them with facts. It’s not about thinking positive. It’s about thinking accurate.
Severe cases (EPDS 15+): Medication becomes necessary. SSRIs like sertraline are first-line. They’re not FDA-approved specifically for postpartum anxiety - but they’re the most studied and safest option for breastfeeding mothers. Only 0.3% of the maternal dose passes into breastmilk. By eight weeks, 64% of women see real improvement.
Here’s the hard part: SSRIs take four to six weeks to kick in. That’s why therapy and mindfulness are used alongside them. You don’t wait for the pill to work. You start feeling better now.
What About Therapy and Support Groups?
CBT works best when combined with support. Women in structured new mothers’ groups are 58% more likely to stick with treatment. Isolation makes anxiety worse. Connection heals it.
Programs like The Women’s Place at Texas Children’s Pavilion for Women offer everything: psychiatric care, medication management, peer groups, and even babysitting so moms can attend sessions. These aren’t luxuries. They’re lifelines.
And digital tools are catching up. The FDA-cleared app MoodMission uses CBT-based exercises. In a trial of 328 postpartum women, it reduced anxiety by 53% over eight weeks. It’s not a replacement for a therapist - but for someone without access to one, it’s a game-changer.
The Big Gaps - And What’s Changing
Only 15% of women with postpartum anxiety get proper care. That’s the real crisis.
Why? Access. Rural hospitals? Only 17% offer perinatal mental health services. Insurance? Coverage jumped from 38% to 79% after new billing codes were added in 2021 - but not everywhere has caught up. Waitlists for therapists? Often months long.
But things are shifting. The American Psychiatric Association predicts a 25% increase in specialized services by 2027. New drugs like brexanolone (Zulresso), currently under FDA review, show promise - 72% response rate in early trials. And more OB-GYNs are being trained to spot the signs.
Still, progress won’t come from clinics alone. It comes from mothers speaking up. From partners asking, “Are you okay - really okay?” From friends saying, “I’ve been there too.”
You’re Not Alone - And Help Is Possible
If you’re reading this and your heart races every time the baby stirs - if you’ve been told you’re just tired, but you know it’s more - you’re not broken. You’re not failing. You’re experiencing a common, treatable condition.
Postpartum anxiety doesn’t mean you love your child less. It means your brain is overwhelmed. And like any injury, it needs care.
Start with one step: Tell someone. A partner. A friend. Your doctor. Say: “I’m not sleeping. I’m scared all the time. I think I might have postpartum anxiety.” That’s not weakness. That’s courage.
There are tools. There are treatments. There are people who know how to help. You don’t have to wait until you’re at your lowest point. You don’t have to suffer in silence. Help is closer than you think.

Write a comment