G6PD Deficiency Risk Assessment Tool
This tool helps determine your risk of hemolytic anemia when taking nitrofurantoin. Based on your ancestry and medical history, it will recommend whether you should discuss G6PD testing with your doctor.
Every year, millions of people take nitrofurantoin to treat a simple urinary tract infection. It works. It’s cheap. And for most people, it’s safe. But for a significant number - especially those with an undiagnosed genetic condition - this common antibiotic can trigger a life-threatening reaction: hemolytic anemia.
What Happens When Nitrofurantoin Meets G6PD Deficiency?
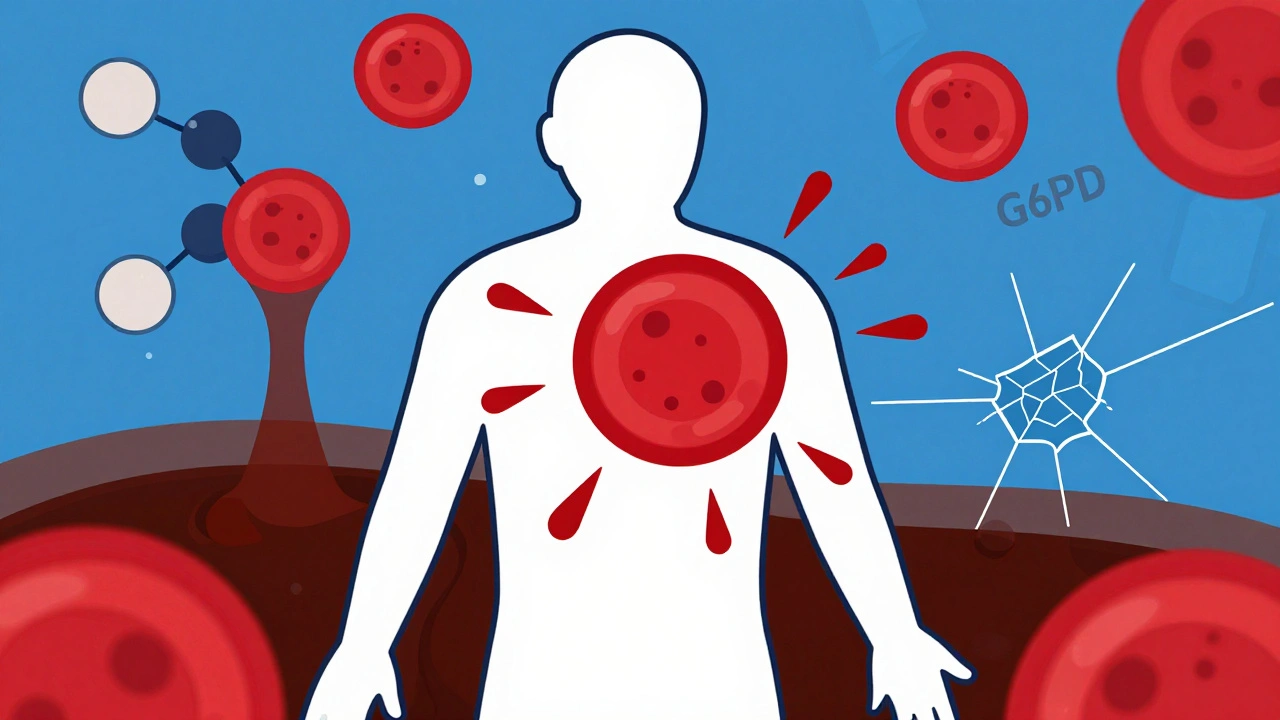
Nitrofurantoin isn’t just any antibiotic. It’s an oxidizing agent. In healthy people, red blood cells handle this just fine. They have a built-in defense system powered by an enzyme called glucose-6-phosphate dehydrogenase (G6PD). This enzyme keeps glutathione - the cell’s main antioxidant - in working order. Glutathione neutralizes harmful oxidants before they can damage hemoglobin and rupture red blood cells. But in people with G6PD deficiency, that defense system is broken. Their red blood cells can’t make enough glutathione. When nitrofurantoin enters the bloodstream, it floods the system with oxidative stress. Hemoglobin starts to clump. Red blood cells swell, become brittle, and burst. This is hemolytic anemia - the sudden, rapid destruction of red blood cells. Symptoms don’t wait. They show up fast: dark urine (like cola), extreme fatigue, jaundice (yellow skin or eyes), shortness of breath, rapid heartbeat, and sometimes fever or back pain. In severe cases, patients collapse from low blood pressure or kidney failure. A 2023 case report in the National Center for Biotechnology Information described a patient whose hemoglobin dropped from 13.2 g/dL to 6.8 g/dL in just 48 hours after starting nitrofurantoin. He was hospitalized. He didn’t need a transfusion. He just needed to stop the drug - and he recovered fully. But not everyone is that lucky.Who’s at Risk?
G6PD deficiency isn’t rare. It affects an estimated 400 million people worldwide. But most don’t know they have it until they take a drug like nitrofurantoin, primaquine, or a sulfa antibiotic. The risk isn’t evenly spread. It’s tied to geography and ancestry:- 10-14% of people of African descent (including African Americans)
- 4-7% of people from the Mediterranean, Middle East, or North Africa
- 2-5% of people from Southeast Asia
Why Is This Still a Problem?
Nitrofurantoin is still widely used because it’s effective against common UTI bugs like E. coli. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), another first-line drug, is rising. Nitrofurantoin keeps working where others fail. That’s why it still makes up about 18% of UTI prescriptions in the U.S. But here’s the catch: the FDA label warns about hemolytic anemia in G6PD-deficient patients - but doesn’t require testing. No mandate. No checklist. No automated alert in most electronic health records. That’s a gap. Doctors often assume: “If they don’t say they have it, they don’t have it.” But 50-60% of people with G6PD deficiency are undiagnosed until they have a crisis. A woman from Sydney with ancestry from Sri Lanka gets a UTI. She’s never been tested. She’s given nitrofurantoin. Three days later, she’s in the ER. That’s not a rare event. It’s predictable.What Are the Alternatives?
You don’t need to risk it. There are safer options:- Fosfomycin - a single-dose pill, safe in G6PD deficiency, effective for uncomplicated UTIs
- Cephalexin - a first-generation cephalosporin, low risk of hemolysis
- Pivmecillinam - used in Europe and Canada, not yet widely available in the U.S., but low oxidative risk
- Trimethoprim-sulfamethoxazole - also risky in G6PD deficiency, so avoid if you’re unsure
What Should You Do?
If you’re prescribed nitrofurantoin, ask:- “Do I have G6PD deficiency?”
- “What’s my ancestry? Am I from Africa, the Mediterranean, or Southeast Asia?”
- “Is there a safer alternative?”
What If I’m Pregnant or Have a Baby?
Pregnant women are at higher risk - not because pregnancy causes G6PD deficiency, but because they’re often treated for UTIs, and the baby might inherit the gene. There are documented cases of newborns developing hemolytic anemia after exposure to nitrofurantoin through the placenta or breast milk. The CPIC guidelines say: avoid nitrofurantoin in pregnancy if G6PD status is unknown. Fosfomycin is the go-to alternative. Infants under one month shouldn’t get nitrofurantoin at all - their liver enzymes aren’t mature enough to handle it, even without G6PD deficiency. But if the mother has G6PD deficiency and takes nitrofurantoin while breastfeeding, the drug can pass into milk and trigger hemolysis in the baby.
What Do the Guidelines Really Say?
The most current guidance comes from the Clinical Pharmacogenetics Implementation Consortium (CPIC), updated in 2023:- Do not use nitrofurantoin in patients with G6PD deficiency and chronic non-spherocytic hemolytic anemia (CNSHA).
- Avoid nitrofurantoin in patients with G6PD deficiency without CNSHA - use alternatives.
- Consider testing before prescribing in high-risk populations.






Write a comment