Many people split pills to save money or ease side effects-but not all splitting is safe. In fact, what you think is a smart workaround might be putting your health at risk. The key isn’t just cutting a pill in half. It’s understanding when and how to adjust your dosing schedule to lower peak concentrations in your blood-and avoid dangerous spikes that cause nausea, dizziness, or worse.
Why Peak Concentrations Matter
When you take a pill, your body doesn’t absorb it all at once. The drug enters your bloodstream, reaches a high point (the peak), then slowly declines. For some medications, that peak is the problem. If it’s too high, you get side effects: nausea from metformin, dizziness from blood pressure meds, or jitteriness from stimulants. The goal isn’t to reduce the total daily dose-it’s to spread it out so your blood levels stay smoother.Think of it like pouring water into a cup. If you dump a full cup all at once, it overflows. But if you pour it slowly, drop by drop, the cup stays full without spilling. That’s what dose splitting does: it avoids the overflow.
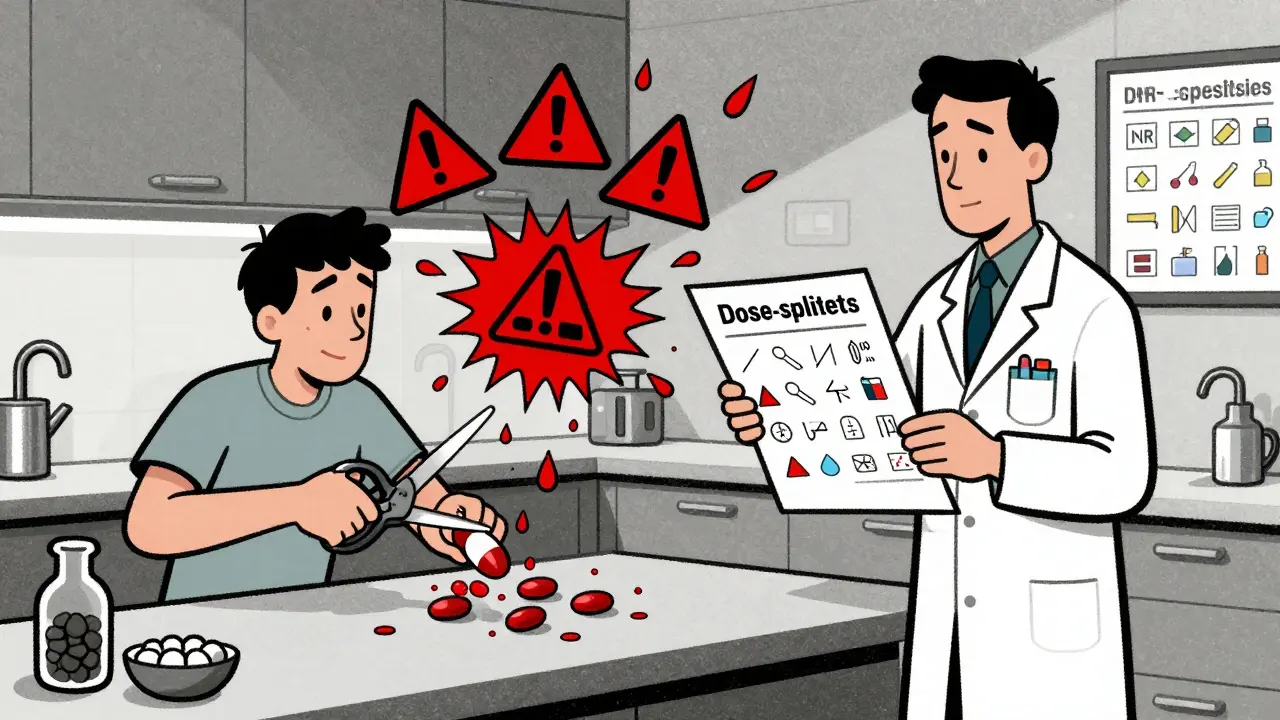
Not All Pills Can Be Split-Even If They’re Scored
Just because a pill has a line down the middle doesn’t mean it’s safe to split. Many extended-release, enteric-coated, or controlled-release pills are designed to release medicine slowly over hours. Cutting them open destroys that design.For example, splitting a 100mg extended-release oxycodone tablet can cause nearly all the drug to flood your system at once. That’s not just risky-it’s life-threatening. The same goes for enteric-coated aspirin. If you break the coating, the drug hits your stomach too fast, increasing irritation and bleeding risk.
On the flip side, immediate-release versions of drugs like lisinopril, metformin, or sertraline are often safe to split-if done correctly. These drugs are absorbed quickly, so splitting the daily dose into two or three smaller doses helps keep blood levels steady. A 2023 NIH case report showed that splitting 20mg of immediate-release lisinopril into two 10mg doses reduced cough side effects by 40% without losing blood pressure control.
What Makes a Drug Safe to Split?
Not every drug responds the same way. Three factors determine whether dose splitting will help:- Half-life: Drugs with short half-lives (under 6 hours) benefit most. If a drug clears from your system in 4-5 hours, taking it once a day means your levels crash and spike. Splitting into two doses keeps levels stable.
- Therapeutic index: This measures how close the effective dose is to the toxic dose. Drugs like warfarin and digoxin have narrow therapeutic indexes (below 2). Even a small dose error can cause bleeding or heart rhythm problems. Don’t split these unless under strict medical supervision.
- Formulation: Immediate-release tablets are the safest to split. Extended-release, delayed-release, or film-coated pills are not.
According to the Australian Prescriber, drugs with half-lives longer than 12 hours-like sertraline or atorvastatin-have a built-in buffer. Even if you split them unevenly, your body smooths out the differences. But for drugs with half-lives under 4 hours, a 10% dose error can cause a 40% drop in blood concentration. That’s why accuracy matters.
Tablet Splitting vs. Dose Splitting: The Big Difference
People often confuse these two things. Tablet splitting means cutting a pill to get a smaller dose-like splitting a 20mg pill to take 10mg. Dose splitting means taking the same total daily dose in smaller, more frequent amounts-like taking 10mg twice a day instead of 20mg once.Tablet splitting is risky if the pill isn’t designed for it. Dose splitting is a clinical strategy, used by doctors to reduce side effects. The difference? One is a physical act. The other is a pharmacological plan.
For example, a patient on 1000mg of immediate-release metformin daily might have severe diarrhea. Their doctor might suggest splitting the dose: 500mg four times a day. The total is still 2000mg-but now the peaks are lower. A Reddit user reported that this cut their diarrhea from 60% of doses down to 15%. That’s not luck-it’s pharmacokinetics.
When Splitting Is Dangerous
The FDA tracked over 1,200 adverse events from improper tablet splitting between 2015 and 2020. Nearly 40% involved blood thinners like warfarin. One patient split a 5mg warfarin tablet, accidentally took 2.5mg one day and 7.5mg the next. Their INR spiked to 8.0-more than triple the safe range. They ended up in the ER with internal bleeding.Another common mistake: splitting extended-release blood pressure pills. A 68-year-old woman split a 40mg lisinopril tablet, thinking she was getting two 20mg doses. She actually got 10mg and 30mg due to uneven breaking. One dose was too low. The other was too high. Her blood pressure spiked to 192/102. She needed emergency treatment.
Dr. Jerry Avorn of Harvard Medical School warns that elderly patients on multiple medications are especially vulnerable. A small dosing error can cascade into falls, confusion, or kidney damage.
How to Split Safely-If It’s Right for You
If your doctor says splitting is appropriate, follow these steps:- Use a dedicated pill splitter, not a knife or scissors. A good splitter reduces dose variation from 25% to under 8%.
- Only split immediate-release tablets with a clear score line.
- Split one pill at a time. Don’t pre-split a week’s supply-medication can degrade or lose potency.
- Store split pills in their original container, away from moisture and heat.
- Use within one week.
Studies show that without training, 65% of patients split pills with more than 15% error. With proper instruction from a pharmacist, that drops to 12%. That’s why a 15-minute consultation matters.
Cost Savings vs. Hidden Risks
Many people split pills to save money. GoodRx reports that splitting an 80mg atorvastatin tablet to get two 40mg doses can save $300 a year. That’s tempting. But here’s the catch: if you split a drug that shouldn’t be split, you could end up paying thousands in ER visits or hospital stays.Pharmaceutical companies are catching on. Pfizer introduced lower-dose rivaroxaban tablets (5mg, 10mg) after noticing 78% fewer splitting attempts. That’s not just business-it’s patient safety.
According to JMCP, inappropriate splitting could cost the U.S. healthcare system $12.3 billion annually in avoidable side effects. The potential savings from splitting? Only $8.9 billion. The math doesn’t add up if safety is ignored.
What’s Changing in 2025
The FDA is moving toward stricter standards. Their 2023 draft guidance requires all scored tablets to pass content uniformity testing before being labeled as splittable. Right now, about 22% of scored tablets fail this test. That means more pills will soon carry a “Do Not Split” warning-even if they look like they can be split.The American Society of Health-System Pharmacists now lists 14 drug classes where dose splitting can reduce side effects: immediate-release opioids (for nausea), stimulants (for jitteriness), and antipsychotics (for drowsiness). But they also list 11 classes where splitting is strictly off-limits: chemotherapy drugs, immunosuppressants, and antiarrhythmics.
A current NIH trial (NCT05521034) is testing whether splitting venlafaxine doses reduces nausea from 32% to 18%. Early results are promising. But until more data is in, stick to what’s proven.
Bottom Line: Talk to Your Pharmacist First
Never split a pill without checking with your doctor or pharmacist. Your medication’s formulation, your health condition, and your other drugs all matter. What works for metformin won’t work for warfarin. What saves money today could cost you dearly tomorrow.There’s no shame in asking: “Is this pill safe to split? Can we adjust the dosing schedule instead?” Most pharmacists are trained to help with this. They’ve seen the mistakes. They know what works.
Lowering peak concentrations can reduce side effects-but only when done right. Don’t guess. Don’t assume. Ask.






Write a comment