Sodium Reduction Impact Calculator
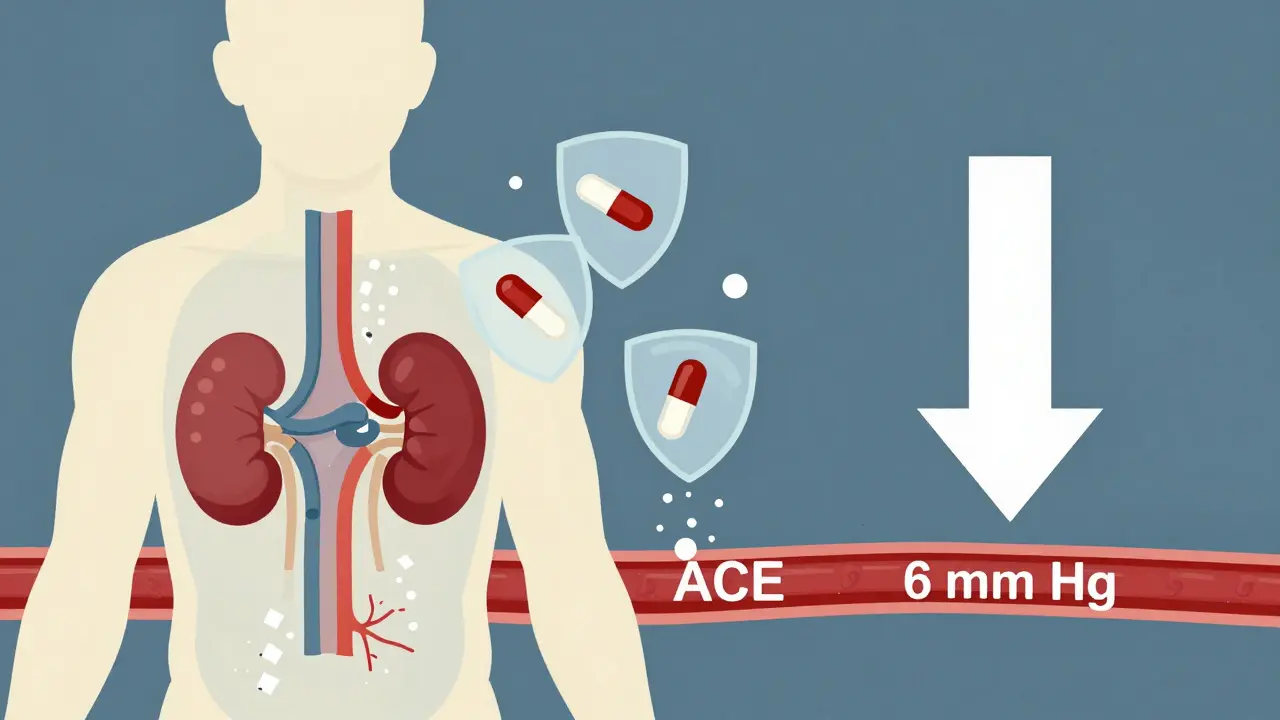
Discover how reducing sodium can boost your blood pressure medication effectiveness. Based on the 2023 JAMA study showing a 6 mm Hg drop in systolic blood pressure with 2,300 mg sodium reduction.
Many people take blood pressure medication and wonder why their numbers won’t drop - even when they’re doing everything right. The answer might be hiding in plain sight: salt. If you’re on medication for high blood pressure and still struggling to get your numbers under control, cutting back on sodium could be the missing piece - not just as a helper, but as a force multiplier for your drugs.
Why Salt Undermines Your Blood Pressure Pills
Blood pressure medications work by targeting specific systems in your body - relaxing blood vessels, helping your kidneys flush out fluid, or blocking hormones that tighten arteries. But when you eat too much salt, your body holds onto water. That extra fluid increases pressure inside your blood vessels, making your heart work harder. And here’s the key: that extra pressure can cancel out the effects of your medication. A major 2023 study published in JAMA showed that people who reduced their daily sodium intake by about one teaspoon (2,300 mg) saw their systolic blood pressure drop by 6 mm Hg - the same drop you’d get from starting a first-line blood pressure pill like an ACE inhibitor. That’s not a small improvement. That’s the kind of change that can move you from high-risk to moderate-risk for heart attack or stroke. What’s even more surprising? This effect happened even in people already taking medication. Many assume that if you’re on pills, diet doesn’t matter as much. But the research says otherwise. When sodium is high, drugs like ACE inhibitors, ARBs, and diuretics simply don’t work as well. Dr. Egan from the American Medical Association put it bluntly: “When they eat more sodium, a lot of their blood pressure medications don’t work as well.”The Science Behind the Numbers
Let’s break down what the numbers actually mean. In the same JAMA study, participants eating their usual diet (about 4,500 mg of sodium a day) had an average systolic blood pressure of 125 mm Hg. When they cut sodium down to just 500 mg a day - roughly a quarter teaspoon - their average pressure dropped to 119 mm Hg. That’s a 6-point drop just from eating less salt. And it wasn’t slow. Most people saw changes within one week. That’s faster than waiting for a new medication to kick in. The effect isn’t the same for everyone. About 25-30% of people are “salt resistant” - their blood pressure barely budges when they cut back. But here’s the catch: even those people benefit in other ways. Less salt means less strain on kidneys, less protein leaking into urine (a sign of kidney damage), and less inflammation in blood vessels. For people with diabetes or kidney disease, this matters just as much as the number on the monitor. For the rest - about 70% of people - sodium reduction is a game-changer. The American Heart Association found that 46% of participants were “salt sensitive,” meaning their blood pressure dropped 5 mm Hg or more when sodium was lowered. That’s not just a statistic. That’s someone who might be able to reduce their pill dosage, avoid side effects, or prevent future complications.Where Your Salt Is Really Coming From
Most people think they’re eating too much salt because they add it at the table or cook with extra seasoning. That’s not the real problem. About 70% of the sodium in the average diet comes from packaged, processed, and restaurant food. Think canned soups, frozen meals, bread, deli meats, soy sauce, salad dressings, and even breakfast cereals. One slice of store-bought bread can have 230 mg of sodium. Two slices? That’s already over 10% of your daily limit before you’ve even eaten anything else. Restaurant meals are even worse. A single serving of spaghetti with meat sauce at a chain restaurant can contain over 2,000 mg of sodium - more than the entire daily recommendation. You can’t just stop using the salt shaker and call it a day. You have to change where you shop and what you buy.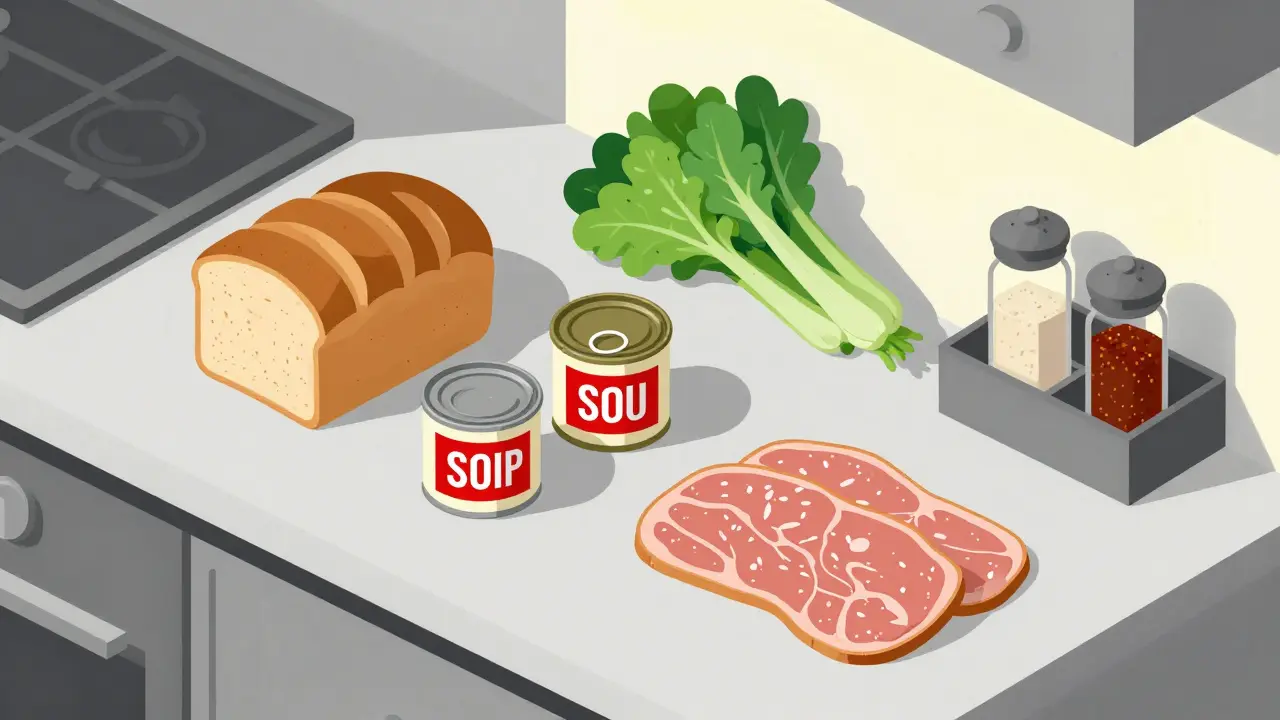
How to Actually Reduce Sodium - Without Giving Up Flavor
You don’t need to eat bland food. You just need to know what to look for.- Read labels like a detective. Look for “sodium” in milligrams (mg), not just % Daily Value. A product with less than 140 mg per serving is considered low-sodium.
- Choose fresh or frozen without sauce. Frozen vegetables without butter or salt, plain chicken or fish, fresh fruit and vegetables - these are your allies.
- Switch to herbs and spices. Garlic powder, smoked paprika, cumin, lemon zest, and black pepper add flavor without sodium. Try no-salt seasoning blends - they’re widely available now.
- Be careful with salt substitutes. Some use potassium chloride instead of sodium. That’s great for most people, but if you have kidney disease or take certain blood pressure meds like ACE inhibitors or ARBs, too much potassium can be dangerous. Talk to your doctor before switching.
- Ask for no salt when ordering out. Most restaurants will accommodate. Say “no added salt” - not “less salt.” The difference matters.
How Sodium Reduction Helps Your Medications Work Better
Here’s the science made simple: salt makes your body hold onto fluid. That fluid increases pressure in your arteries. Blood pressure meds try to fix that - but if you keep flooding your system with sodium, they’re fighting a losing battle. Reducing sodium helps in three key ways:- Reduces plasma volume. Less fluid in your bloodstream means less pressure on artery walls.
- Lowers vascular resistance. Your blood vessels relax more easily, making it easier for blood to flow.
- Improves endothelial function. The lining of your blood vessels works better, which helps medications like ACE inhibitors do their job.
Who Benefits the Most?
Not everyone responds the same. But certain groups see the biggest improvements:- Older adults. As you age, your kidneys become less efficient at flushing sodium.
- Black adults. Studies consistently show higher salt sensitivity in this group, which may partly explain higher rates of hypertension.
- People with diabetes or kidney disease. High sodium worsens protein in urine and accelerates kidney damage.
- Those with higher starting blood pressure. The higher your baseline, the more you stand to gain.
What Experts Are Saying Now
Guidelines have changed. The American Heart Association still recommends 1,500 mg of sodium per day as ideal, with 2,300 mg as the absolute maximum. The Joint National Committee now lists sodium reduction as a Class I recommendation - the strongest possible - for all hypertensive patients, alongside medication. The FDA has set voluntary targets for food companies to reduce sodium in packaged foods by 2026, aiming to bring average intake down to 3,000 mg. But experts say that’s still too high. The real goal? Getting the average American under 2,000 mg. Dr. Thomas Wang, one of the study authors, called integrating sodium control with medication “the most significant advance in hypertension control since combination drug therapy.” That’s not hype. That’s data.What to Do Next
If you’re on blood pressure medication:- Track your sodium for a week. Use a free app like MyFitnessPal or Cronometer. Write down everything you eat and drink.
- Identify your top three sodium sources. Is it bread? Soup? Deli meat? Swap one out this week.
- Ask your doctor about potassium substitutes. Only if your kidneys are healthy.
- Recheck your blood pressure in 7-10 days. You might be surprised.
Can I stop my blood pressure medication if I eat less salt?
No - never stop or change your medication without talking to your doctor. Reducing salt can improve how well your meds work, and in some cases, it may allow your doctor to lower your dose. But stopping medication on your own can be dangerous. Always work with your healthcare provider to adjust treatment safely.
Is sea salt or Himalayan salt better than table salt?
No. All types of salt - including sea salt, kosher salt, and Himalayan pink salt - are made of sodium chloride. They may have different textures or trace minerals, but they contain the same amount of sodium per gram. Switching salt types won’t help your blood pressure. What matters is how much you use.
How long does it take to see results from cutting salt?
Most people see a drop in blood pressure within 1 to 2 weeks. In the 2023 JAMA study, participants showed measurable changes in just seven days. The longer you stick with it, the more stable your numbers become.
Can low sodium cause problems?
For most people, eating less than 2,300 mg of sodium per day is safe and beneficial. Very low sodium (below 1,500 mg) is only recommended for those with high blood pressure or heart failure, and even then, under medical supervision. Extremely low sodium (under 1,000 mg) can rarely cause issues like dizziness or low blood pressure in older adults or those on multiple medications - but this is uncommon. The bigger risk is eating too much, not too little.
Do salt substitutes work, and are they safe?
Salt substitutes that use potassium chloride can help lower sodium intake and may even help lower blood pressure further. But they’re not safe for everyone. If you have kidney disease, diabetes, or take certain blood pressure meds like ACE inhibitors or ARBs, potassium can build up in your blood and become dangerous. Always check with your doctor before using them.
What’s the best way to track my sodium intake?
Use a free app like MyFitnessPal or Cronometer. Scan barcodes on packaged foods or search for meals in their database. Focus on the actual milligrams of sodium, not the % Daily Value. Keep a log for at least 3-5 days to see your patterns. After that, aim to stay under 2,300 mg daily - and ideally under 1,500 mg if your doctor recommends it.







Write a comment