Deprescribing: How to Safely Reduce Unnecessary Medications
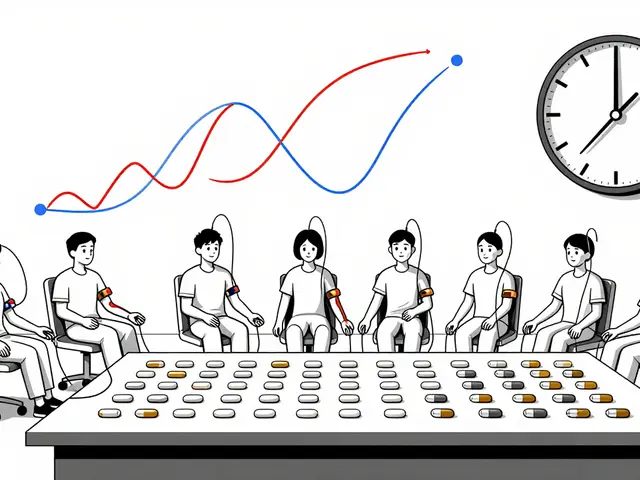
When you take too many pills, it’s not always helping—it might be hurting. Deprescribing, the planned and supervised process of reducing or stopping medications that are no longer beneficial or are causing harm. Also known as medication tapering, it’s not about quitting drugs cold turkey—it’s about making smart, step-by-step changes to protect your body and your quality of life. Many older adults, especially those on multiple prescriptions, are taking drugs that were meant for short-term use but kept going for years. This isn’t rare—it’s common. Doctors often add meds to treat side effects from other meds, creating a chain reaction called polypharmacy, the use of five or more medications at the same time. Also known as medication overload, it increases the risk of falls, confusion, kidney damage, and even hospital visits.
Deprescribing isn’t just for seniors. People on long-term painkillers, sleeping pills, or acid reducers often don’t realize their body has adapted—and now they need the drug just to feel normal. Stopping suddenly can be dangerous, which is why this process needs a plan. It’s not a one-size-fits-all fix. A drug that helped two years ago might now be doing more harm than good. That’s where medication reduction, the intentional lowering of drug doses or discontinuation based on current health needs. Also known as drug withdrawal management, it’s a key part of modern, patient-centered care. Think of it like cleaning out your medicine cabinet: keep what’s useful, toss what’s expired or unnecessary. The goal isn’t fewer pills for the sake of it—it’s better health, fewer side effects, and more energy to do the things you love.
Some of the most common meds targeted in deprescribing include proton pump inhibitors for heartburn, benzodiazepines for sleep, antipsychotics for behavioral issues in dementia, and blood pressure drugs that no longer match your current numbers. Each one has a safe way out, but it takes time, monitoring, and communication with your provider. You’re not alone in this. Pharmacists, nurses, and doctors are learning how to spot when a med is doing more harm than good. And now, with Medicare Annual Medication Reviews and Extra Help Programs, there’s more support than ever to review what you’re really taking.
What you’ll find in this collection are real stories and clear guides on how to talk to your doctor about cutting back, what to watch for when stopping a drug, and how to replace harmful habits with safer ones. From managing dry eyes caused by antidepressants to understanding how immunosuppressants affect vaccines, these posts show how medication decisions ripple through your whole health. Whether you’re a patient, caregiver, or healthcare worker, deprescribing isn’t a trend—it’s a necessary step toward smarter, safer care. Let’s look at what works, what doesn’t, and how to make the next move with confidence.
- By Percival Harrington
- /
- 18 Jan 2026
How to Work with Your Doctor to Deprescribe and Save Money
Learn how to safely stop unnecessary medications with your doctor to cut costs, reduce side effects, and avoid hospital visits. Deprescribing saves money and improves health-here's how to start.
- By Percival Harrington
- /
- 21 Nov 2025
Deprescribing Research: What Happens When You Reduce Medications in Older Adults
Deprescribing reduces unnecessary medications in older adults to improve safety and quality of life. Research shows it lowers pill burden, reduces falls and hospitalizations, and restores well-being-when done carefully with patient input.