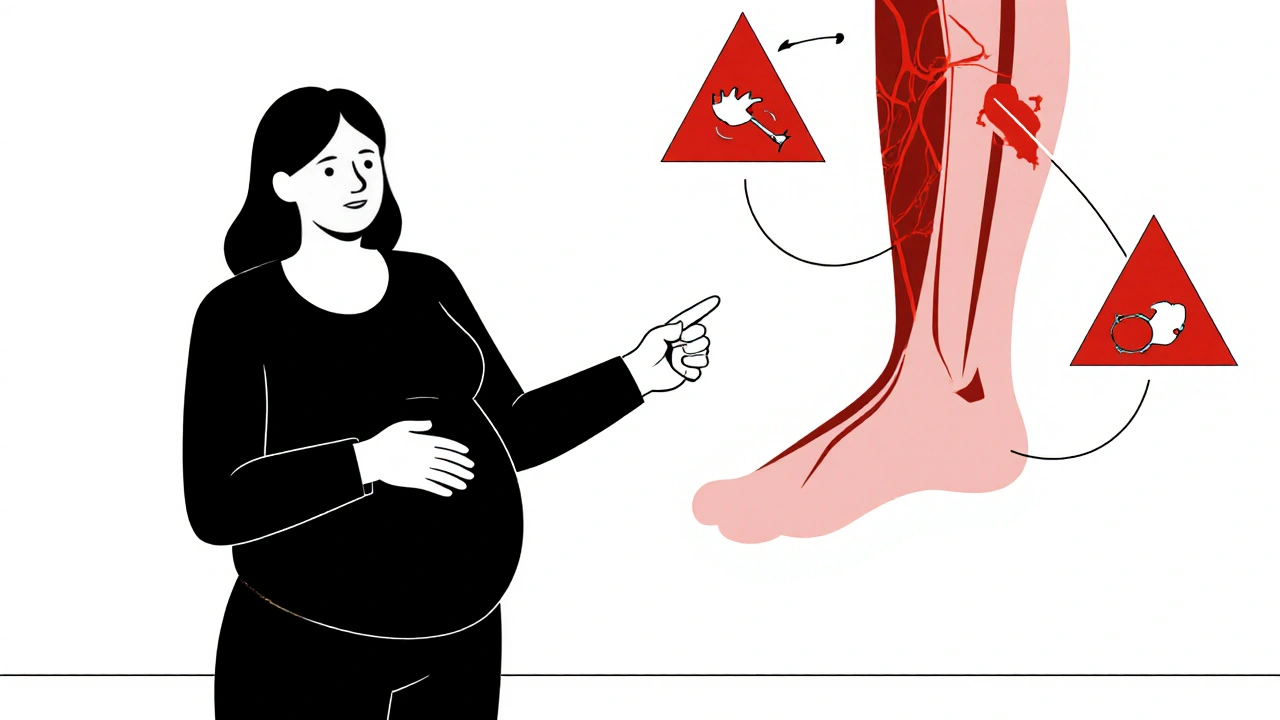
Pregnancy Blood Clot Risks: What You Need to Know
When you're pregnant, your body naturally becomes more prone to blood clots, abnormal clumping of blood that can block vessels and lead to serious complications. Also known as thrombosis, this is one of the leading causes of pregnancy-related deaths in the U.S. and Europe. The risk goes up because your blood clots faster to prevent excessive bleeding during delivery, and your growing uterus puts pressure on major veins, slowing circulation. This isn’t something that happens to everyone—but it’s serious enough that every pregnant person should understand the signs, causes, and how to reduce their chances.
One of the most common types of clot during pregnancy is deep vein thrombosis, a clot that forms in a deep vein, usually in the leg. It can cause swelling, pain, warmth, or redness in one leg—often mistaken for muscle cramps. If the clot breaks loose and travels to the lungs, it becomes a pulmonary embolism, a life-threatening blockage in the lung arteries. Symptoms include sudden shortness of breath, chest pain that gets worse when breathing, rapid heartbeat, or coughing up blood. These aren’t rare; about 1 in 1,000 pregnant women develop a clot, and the risk stays high for up to 6 weeks after giving birth.
Some women are at higher risk: those over 35, carrying multiples, on bed rest, with a history of clots, or who have genetic clotting disorders like Factor V Leiden. Even cesarean sections double the risk compared to vaginal birth. Medications like anticoagulants during pregnancy, blood thinners used to prevent or treat clots without harming the baby—such as heparin or low-molecular-weight heparin—are often prescribed for high-risk cases. These are safe in pregnancy because they don’t cross the placenta, unlike warfarin, which can cause birth defects. Lifestyle changes matter too: staying active, drinking plenty of water, wearing compression stockings, and avoiding long periods of sitting can lower your risk.
Many women don’t realize that the danger doesn’t end at delivery. The highest risk period is actually the first few weeks after birth. That’s why some doctors recommend continuing anticoagulant treatment for a month postpartum. If you’ve had a clot before, your doctor will likely monitor you closely during pregnancy and plan ahead for delivery. It’s not about fear—it’s about awareness. Knowing the warning signs can mean the difference between a routine checkup and an emergency.
Below, you’ll find real-world advice from posts that cover clot prevention, medication safety, and what to watch for during and after pregnancy. These aren’t theoretical guides—they’re practical, tested tips from women and clinicians who’ve dealt with this firsthand.
- By Percival Harrington
- /
- 18 Nov 2025
Blood Clots and Pregnancy: What Every Expectant Mother Should Know
Blood clots during pregnancy are rare but dangerous. Learn the real risks, warning signs, and what to do if you're at risk - so you can stay safe and informed.