One in every 1,000 pregnant women in Australia will develop a dangerous blood clot during pregnancy or shortly after giving birth. That’s not rare. It’s not something that only happens to older moms or women with complicated histories. It can happen to you - even if you’re young, healthy, and active. And most women don’t know the signs until it’s too late.
Why Pregnancy Increases Your Risk
Your body changes in dozens of ways when you’re pregnant. One of the most important? Your blood starts clotting more easily. That’s not a bug - it’s a feature. During childbirth, your body needs to stop heavy bleeding fast. So nature turns up the clotting dial.
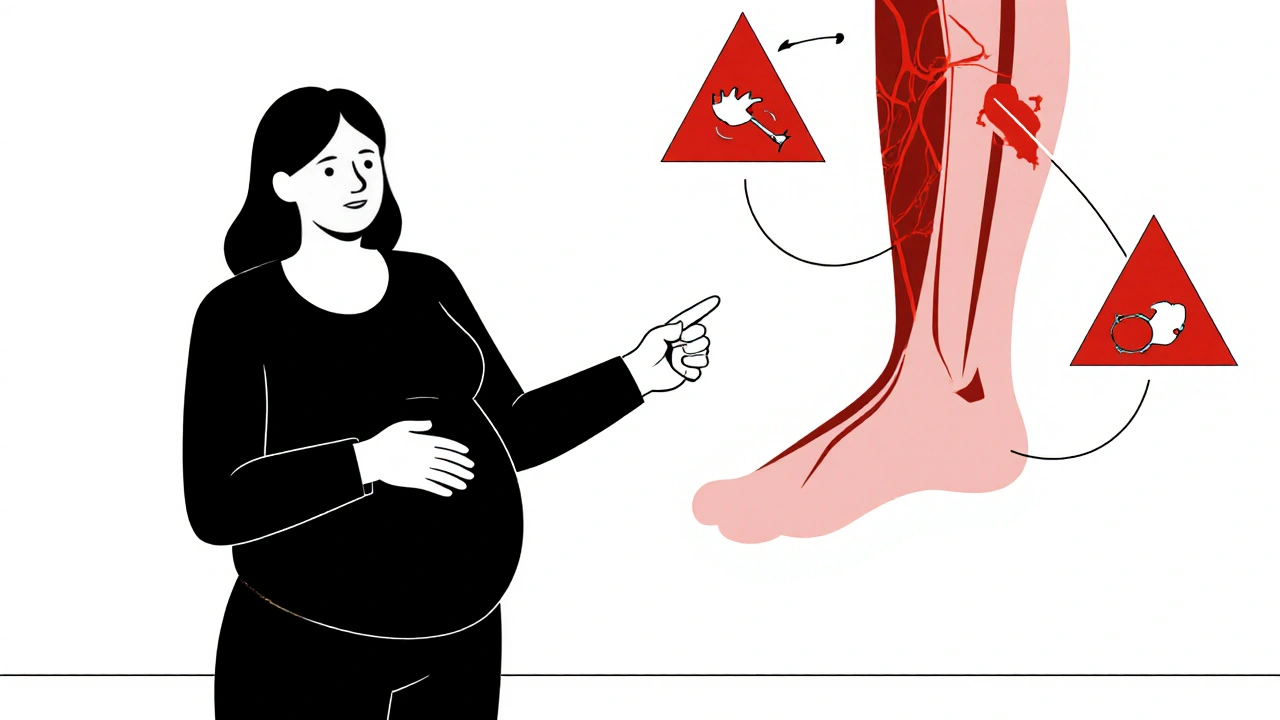
But that same mechanism can backfire. Blood flow slows down in your legs and pelvis as your growing uterus presses on major veins. Hormones like estrogen increase clotting proteins. And after delivery, your body stays in this high-clotting state for weeks. That’s why the highest risk isn’t during pregnancy - it’s in the first six weeks after birth.
Women with a personal or family history of blood clots, those carrying multiples, or those who have had a C-section are at higher risk. But even healthy first-time moms with no history can get them. That’s why everyone needs to know the warning signs.
What to Watch For: Symptoms You Can’t Ignore
Most dangerous clots form in the deep veins of the legs - called deep vein thrombosis, or DVT. The symptoms are simple, but easy to miss because they feel like normal pregnancy discomforts.
- Swelling in one leg (not both)
- Pain or tenderness in the calf or thigh, especially when standing or walking
- Warmth or redness in the affected area
- A visible vein that looks bulging or rope-like
If the clot breaks loose and travels to your lungs, it becomes a pulmonary embolism - a medical emergency. Symptoms include:
- Sudden shortness of breath, even when resting
- Chest pain that gets worse when you breathe deeply
- Rapid heartbeat or dizziness
- Coughing up blood
These symptoms don’t always come with warning. One woman I spoke with in Sydney thought her chest pain was just heartburn. She waited two days before going to the hospital. By then, the clot had blocked nearly half of her lung. She survived - but barely.
Who Needs Testing or Prevention?
Not every pregnant woman needs blood thinners. But if you have certain risk factors, your doctor should talk to you about prevention.
High-risk factors include:
- A personal history of DVT or pulmonary embolism
- A close relative (parent or sibling) who had a clot before age 45
- Known clotting disorders like Factor V Leiden or antiphospholipid syndrome
- Being over 35 and carrying twins or more
- Having a C-section, especially if it was unplanned or complicated
- Being on bed rest for more than three days
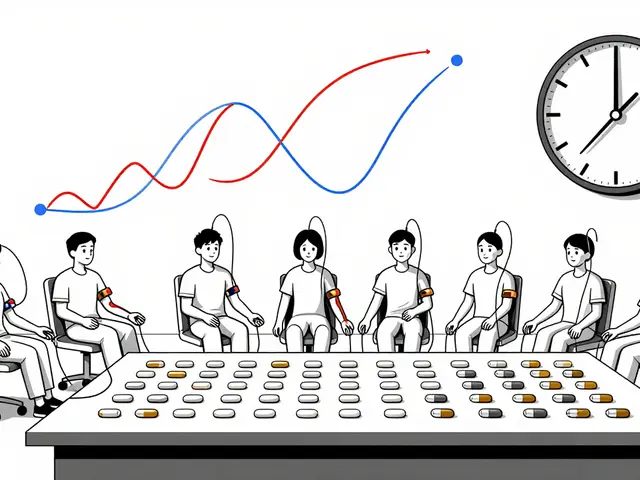
If you have one or more of these, your doctor may recommend low-dose heparin injections during pregnancy and after birth. These are safe for the baby and very effective at preventing clots.
Even if you don’t have risk factors, moving your legs often helps. Walk daily. Do simple ankle circles while sitting. Avoid crossing your legs for long periods. If you’re flying after 28 weeks, wear compression stockings and get up to walk every hour.

What About Birth Control and Clotting?
Many women stop taking hormonal birth control when they get pregnant - good. But some don’t realize that certain pills, patches, or rings can increase clotting risk even before conception.
Combined hormonal contraceptives (those with estrogen and progestin) are linked to a 3 to 4 times higher risk of clots than non-users. If you’ve had a clot before, you should never take these again. Even if you’re planning to get pregnant, talk to your doctor about switching to progestin-only options or an IUD.
And here’s something most women don’t know: if you’ve had a clot during a previous pregnancy, your chance of having another one is about 1 in 5. That’s not a small number. It means your next pregnancy needs a different plan.
What Happens If You Get a Clot?
If you’re diagnosed with a blood clot during pregnancy, you won’t be sent home with a warning and a prayer. Treatment is well-established and safe.
The standard is low-molecular-weight heparin (LMWH), given as daily injections under the skin. It doesn’t cross the placenta, so it doesn’t affect the baby. You’ll usually keep taking it through delivery and for at least six weeks after.
Warfarin - a common blood thinner for non-pregnant people - is dangerous during pregnancy. It can cause birth defects. So don’t assume your old prescription still works. Always tell any doctor you’re pregnant before taking anything.
Most women on treatment go on to deliver healthy babies. The key is early detection. Delaying care increases the risk of complications - for both you and your baby.
Myths That Put Women at Risk
There are dangerous myths floating around about blood clots and pregnancy.
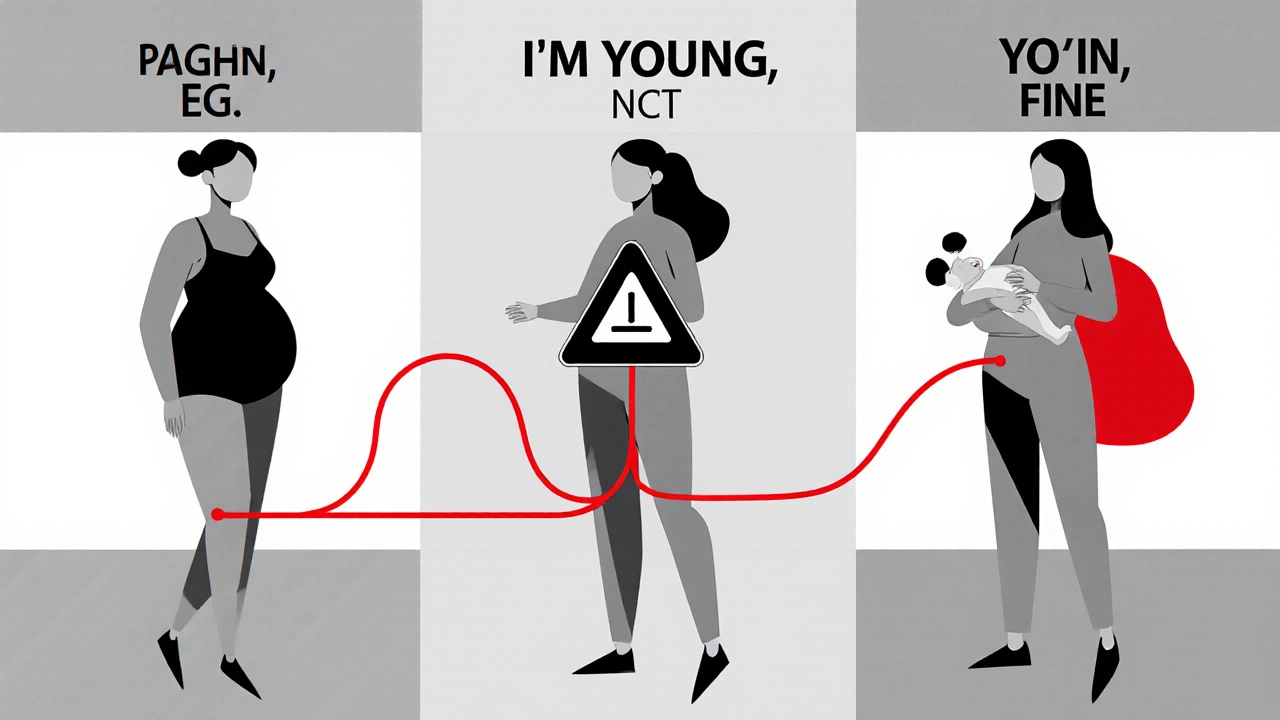
Myth: "Only older moms get clots. I’m 24, I’m fine."
Truth: The average age of women who get pregnancy-related clots is 28. Younger women are just as likely - they’re just less likely to be warned.
Myth: "If I’m active, I won’t get one."
Truth: Athletes and yoga instructors get clots too. Activity helps, but doesn’t eliminate risk.
Myth: "I had a clot before, but I’m healthy now. It won’t happen again."
Truth: Once you’ve had one, your body remembers. Recurrence risk stays high for years.
Myth: "My doctor didn’t mention it, so I must be low risk."
Truth: Many doctors still don’t screen for clotting risk unless you’ve had a prior event. Don’t wait for them to bring it up. Ask.
What You Can Do Right Now
You don’t need to live in fear. But you do need to be informed.
Here’s what to do today:
- Write down your family history: Did any parent, sibling, or grandparent have a clot before age 50? Did anyone have unexplained miscarriages or stillbirths? That’s a red flag.
- Ask your midwife or OB: "Am I at risk for blood clots? Should I be tested for clotting disorders?" Don’t let them brush you off.
- If you’re over 35, carrying twins, or had a C-section last time - bring it up even if you feel fine.
- Learn the symptoms. Print them out. Put them on your fridge. Share them with your partner.
- If you notice swelling, pain, or sudden breathing trouble - don’t wait. Go to the emergency room. Say: "I’m pregnant and I think I might have a blood clot."
There’s no magic pill to prevent every clot. But knowledge? That’s power. And in pregnancy, power can mean the difference between a healthy birth and a life-threatening emergency.
Frequently Asked Questions
Can I still have a natural birth if I’m on blood thinners?
Yes. Most women on low-molecular-weight heparin can have a vaginal delivery. Your doctor will time your last injection carefully - usually 24 hours before labor starts - to reduce bleeding risk. Epidurals are also safe if you follow the timing guidelines. Always discuss your birth plan with your care team early.
Are blood clots more common in C-sections or vaginal births?
C-sections carry a higher risk - about 4 to 10 times higher than vaginal births. That’s why women who have planned or emergency C-sections are often given blood thinners after delivery, even if they had no prior risk factors. The surgery, immobility, and tissue trauma all increase clotting.
Can I breastfeed while taking blood thinners?
Absolutely. Low-molecular-weight heparin doesn’t enter breast milk in meaningful amounts. It’s considered safe for nursing. Warfarin is also generally safe in small doses. But always confirm with your doctor - never assume.
What are clotting disorders, and how are they tested?
Clotting disorders are inherited or acquired conditions that make your blood clot too easily. Common ones include Factor V Leiden, prothrombin gene mutation, and antiphospholipid syndrome. Testing involves a simple blood draw. But doctors usually only test if you’ve had a clot, a family history, or multiple miscarriages. If you’re unsure, ask your doctor: "Should I be tested?"
Is it safe to fly during pregnancy if I’m worried about clots?
Flying increases risk slightly - especially flights longer than four hours. But for most healthy pregnant women, the risk is low. Wear compression stockings, drink water, and walk the aisle every hour. If you have risk factors, talk to your doctor about whether you need a heparin shot before flying. Don’t avoid travel - just plan it smartly.
Next Steps for Every Expectant Mother
Don’t wait for symptoms. Don’t wait for your doctor to mention it. Blood clots during pregnancy are preventable - but only if you act.
Start by writing down your family’s medical history. Then, schedule a quick chat with your midwife or OB. Ask: "Based on my health and history, am I at risk? What should I watch for?"
And if you ever feel something’s off - swelling, pain, trouble breathing - trust your gut. Go to the hospital. Say the words: "I’m pregnant and I think I have a blood clot."
That one conversation could save your life - and your baby’s.




Write a comment