When you’re on medication for osteoporosis, waiting a year or two to see if it’s working can feel like gambling with your bones. That’s where bone turnover markers come in-they give you real-time feedback on whether your treatment is actually doing its job, long before a DEXA scan can show any change.
Why Wait Two Years When You Can Know in Three Months?
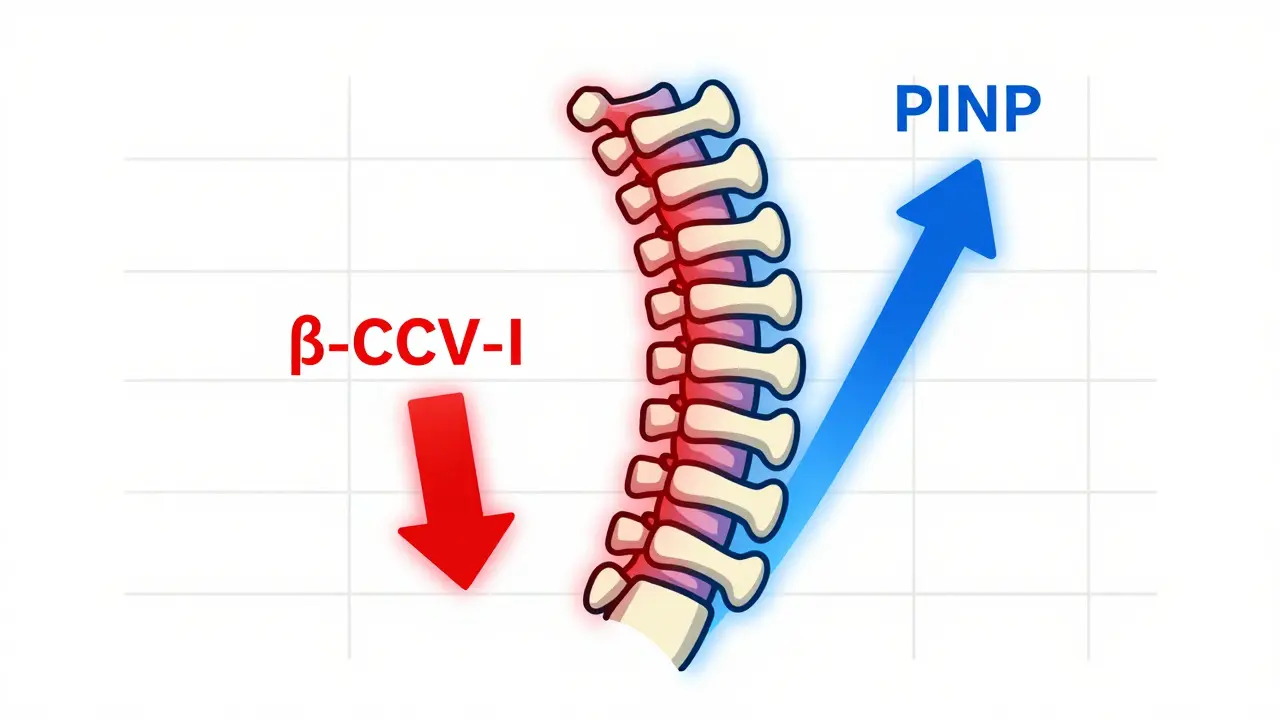
For decades, the only way to measure if osteoporosis treatment was working was to wait 12 to 24 months and get another bone density scan. But bone mineral density (BMD) changes slowly. A 1-3% improvement at the spine might not even be noticeable above the test’s natural error margin. Meanwhile, your bones could still be breaking. That’s where bone turnover markers (BTMs) change the game. These are proteins and fragments in your blood or urine that come straight from bone remodeling-either the breaking down of old bone (resorption) or building new bone (formation). Unlike BMD scans, BTMs respond fast. Within just 3 to 6 weeks of starting treatment, you’ll see measurable shifts. By 3 months, you’ll know if your body is responding. This isn’t theory. The International Osteoporosis Foundation and European Calcified Tissue Society confirmed in 2023 that serum PINP and plasma β-CTX-I are the gold-standard markers for clinical use. PINP reflects bone formation. β-CTX-I reflects bone resorption. Both are measured with simple blood tests.What the Numbers Actually Mean
If you’re on an anti-resorptive drug-like a bisphosphonate or denosumab-you want to see your β-CTX-I drop. A reduction of more than 30% at the 3-month mark is considered a strong sign the drug is working. For PINP, a drop of 35% or more signals the same. If you’re on an anabolic drug like teriparatide, you want the opposite: PINP should spike by 70-100% within 1-3 months, showing your body is building new bone. The least significant change (LSC) is key here. It’s the smallest change that’s real-not just lab noise. For PINP, it’s 20%. For β-CTX-I, it’s 25%. So if your β-CTX-I drops from 0.5 ng/mL to 0.4 ng/mL, that’s only a 20% change. That’s not enough. You need to drop below 0.375 ng/mL to cross the threshold. And here’s the kicker: patients who hit these targets at 3 months have a 1.6% lower fracture risk after just 22 weeks, according to the TRIO study. That’s not just statistical-it’s personal. It means fewer broken hips, fewer hospital stays, fewer lost months of independence.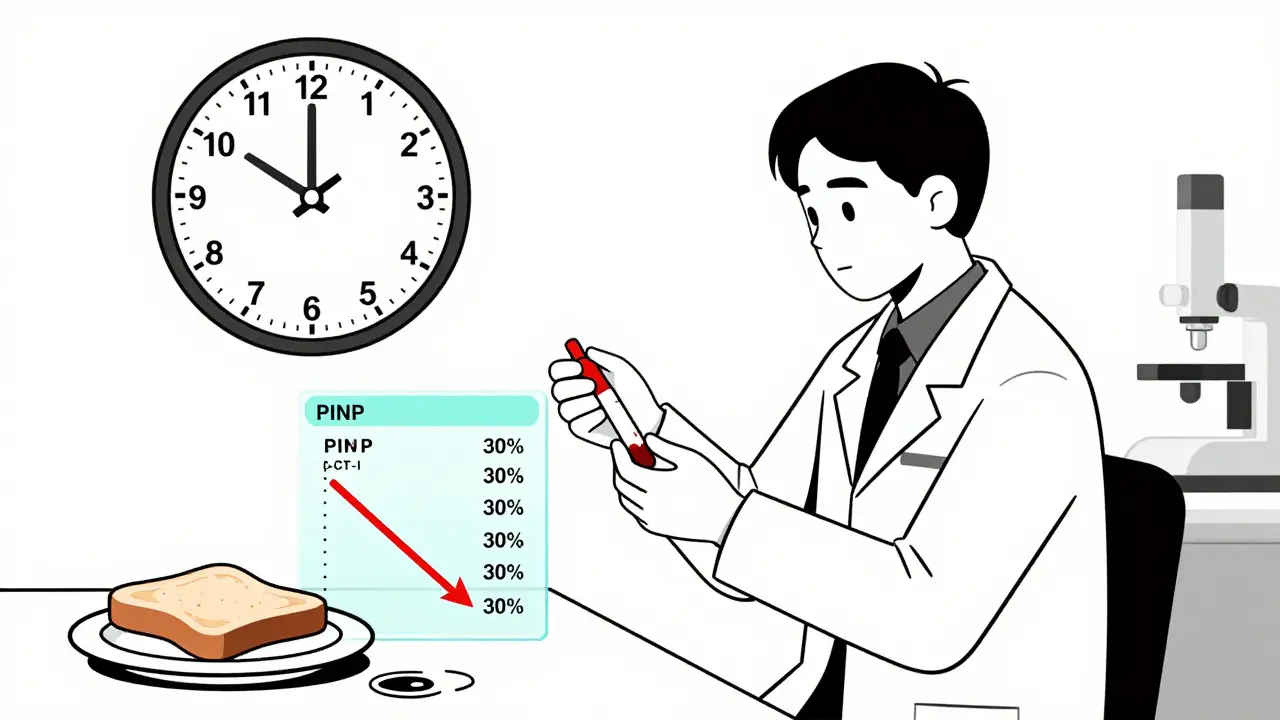
How to Get Accurate Results (And Why Most People Don’t)
These tests are powerful-but only if done right. The biggest reason BTMs aren’t used more? Poor sample collection. For β-CTX-I, you must fast overnight. Eat breakfast, and your levels jump 20-30%. That’s not your body changing bone turnover-it’s your toast messing up the test. You also have to give blood between 8 and 10 a.m. CTX levels rise naturally throughout the day, with up to 40% variation by evening. PINP is more stable, but still best measured in the morning. Even the tube matters. Plasma (not serum) is required for β-CTX-I. If your lab uses the wrong tube, the result is garbage. And if your lab doesn’t use standardized assays? You’re getting numbers that can’t be compared to clinical guidelines. Only about 65% of U.S. labs follow the IFCC-recommended protocols. In Australia and Europe, adoption is higher, but inconsistent. That’s why your doctor needs to specify: "Plasma β-CTX-I, fasting, 8-10 a.m., Roche Elecsys assay." If they don’t, the result is meaningless.Who Should Get Tested-and Who Doesn’t Need It
BTMs aren’t for everyone. If you’ve just been diagnosed and are starting treatment, yes-baseline and 3-month tests are critical. They help confirm you’re taking your meds, and if you’re not responding, you can switch faster. They’re especially useful for people with:- High fracture risk despite normal BMD
- History of poor medication adherence
- Chronic kidney disease (CKD)-where traditional markers like PINP and CTX can be falsely elevated due to reduced clearance
- Unclear response to therapy after 12 months

What’s Next for Bone Turnover Markers
The field is moving fast. The American Association of Clinical Endocrinologists is expected to update its osteoporosis guidelines in mid-2024 to include BTMs as standard monitoring tools. Medicare has already been covering PINP (CPT 83970) and β-CTX-I (CPT 83935) since 2020, paying around $30 per test. New research is looking at using BTMs to personalize treatment duration. Right now, most people stay on bisphosphonates for 5-10 years, even if they’re doing great. But if your β-CTX-I stays low for 2 years, maybe you don’t need to keep taking it. Trials are underway to test "drug holidays" guided by BTMs. There’s also work on point-of-care tests-finger-prick versions that could give results in minutes. Not yet available, but in development. If they work, BTMs could become as routine as checking your blood pressure.The Bottom Line: Fast Feedback, Better Outcomes
Osteoporosis treatment isn’t about waiting. It’s about acting. Bone turnover markers give you the fastest, most direct window into whether your therapy is working. They cut through guesswork. They catch non-adherence before fractures happen. They help avoid years of unnecessary medication. If you’re on osteoporosis treatment, ask your doctor: "Can we check my PINP and β-CTX-I at baseline and again at 3 months?" If they say no, ask why. If they say it’s not covered, remind them Medicare pays for it. If they say it’s not standard, show them the 2023 IOF/ESCEO/IFCC consensus. This isn’t experimental. It’s evidence-based. And for anyone serious about protecting their bones, it’s the smartest next step.What are the best bone turnover markers for monitoring osteoporosis treatment?
The two most reliable markers are serum procollagen type I N propeptide (PINP) for bone formation and plasma β-isomerized C-terminal telopeptide of type I collagen (β-CTX-I) for bone resorption. These are recommended by the International Osteoporosis Foundation and European Calcified Tissue Society as the reference markers due to their precision, standardization, and strong correlation with treatment response.
When should bone turnover markers be tested during treatment?
Test at baseline before starting treatment, then again at 3 months. This gives you the clearest picture of early response. For anti-resorptive drugs, a 30%+ drop in β-CTX-I or 35%+ drop in PINP indicates good response. For anabolic drugs like teriparatide, a 70-100% rise in PINP is expected. A second test at 6 months can confirm stability.
Do I still need a DEXA scan if I’m using bone turnover markers?
Yes. Bone turnover markers show how active your bones are, but they don’t measure bone density. DEXA scans are still the gold standard for diagnosing osteoporosis and tracking long-term changes in bone mineral density. Use BTMs for early feedback and DEXA for definitive assessment-typically at 12 to 24 months.
Why do I have to fast and test in the morning for β-CTX-I?
β-CTX-I levels rise significantly after eating and throughout the day-up to 40% variation. Fasting overnight and testing between 8 and 10 a.m. minimizes this biological noise. If you eat before the test or have it in the afternoon, your result could look worse than it is, leading to unnecessary treatment changes.
Can bone turnover markers be used for people with kidney disease?
Standard markers like PINP and β-CTX-I can be falsely elevated in chronic kidney disease because the kidneys clear them slower. For these patients, bone alkaline phosphatase (BALP) and tartrate-resistant acid phosphatase 5b (TRACP5b) are preferred. Reference ranges also differ by kidney stage, so labs must adjust interpretation accordingly.
Are bone turnover marker tests covered by insurance?
In the U.S., Medicare covers both PINP (CPT 83970) and β-CTX-I (CPT 83935) for osteoporosis monitoring since 2020, with reimbursement around $30 per test. Coverage varies elsewhere, but in Australia and much of Europe, these tests are increasingly included in public health guidelines for high-risk patients.
What if my bone turnover marker results don’t improve after 3 months?
If your β-CTX-I or PINP doesn’t change by at least the least significant change (20-25%), you’re likely a non-responder. This could mean poor adherence, malabsorption (e.g., from GI issues), or a drug that doesn’t suit your biology. Your doctor may switch therapies, check vitamin D levels, or evaluate for secondary causes of bone loss like hyperparathyroidism.






Write a comment