Blood Clots During Pregnancy: Risks, Signs, and What You Need to Know
When you’re pregnant, your body changes in ways that help support a growing baby—but some of those changes also raise the risk of blood clots during pregnancy, abnormal clots that form in veins and can block blood flow, posing serious risks to both mother and baby. Also known as venous thromboembolism, this condition is one of the top causes of pregnancy-related deaths in the U.S. and Europe. You’re up to five times more likely to develop a clot while pregnant than when you’re not, and the risk stays high for weeks after delivery. It’s not something you should panic about, but it’s something you absolutely should understand.
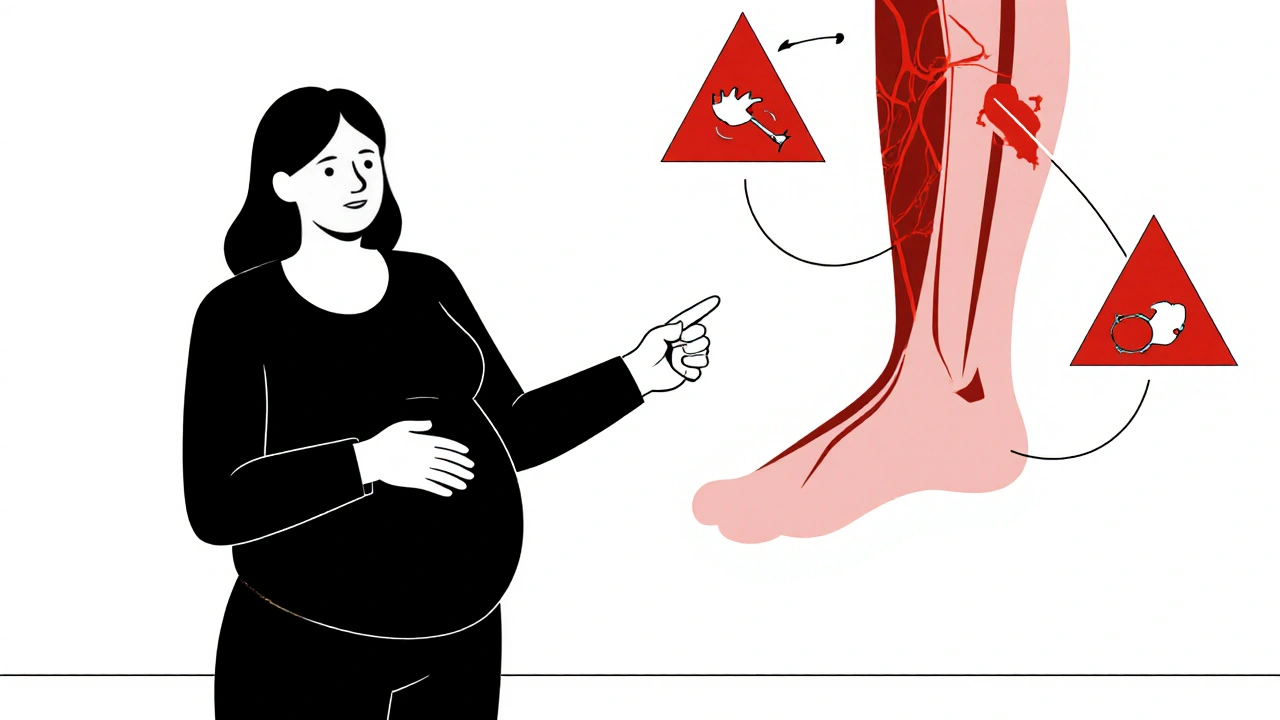
Most clots happen in the legs, especially the deep veins—this is called deep vein thrombosis, a condition where a clot forms in a deep vein, usually in the lower leg or thigh. If that clot breaks loose and travels to the lungs, it becomes a pulmonary embolism, a life-threatening blockage in the arteries of the lungs. Symptoms like sudden swelling, warmth, or pain in one leg, shortness of breath, chest pain, or a rapid heartbeat aren’t normal during pregnancy. They’re red flags. Many women dismiss them as normal swelling or fatigue, but waiting too long can be deadly.
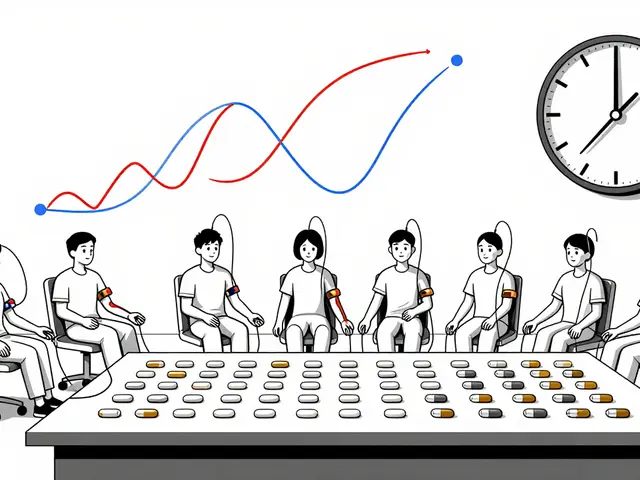
Why does this happen? Pregnancy increases clotting factors in your blood to prevent excessive bleeding during delivery. That’s helpful—until it’s not. Your growing uterus also presses on major veins, slowing blood flow. Add in long periods of sitting (like on flights or during bed rest), obesity, a history of clots, or genetic conditions like Factor V Leiden, and your risk climbs even higher. Some women need low-dose blood thinners like heparin during pregnancy because they’re safe for the baby and effective at preventing clots. Warfarin? Not so much—it can harm the fetus. That’s why knowing your personal risk factors matters before and during pregnancy.
Doctors don’t test everyone for clotting risks unless there’s a history or warning signs. But if you’ve had a clot before, or if someone in your family has a known clotting disorder, talk to your provider early. Simple steps—like staying active, drinking water, avoiding long flights without movement, and wearing compression socks—can cut your risk significantly. And if you feel something off, don’t wait. Call your doctor. A quick ultrasound can rule out a clot in minutes.
The posts below cover real cases, treatment options, medication safety during pregnancy, and how to recognize warning signs before it’s too late. You’ll find clear advice on what to ask your OB-GYN, which blood thinners are safe, and how to spot trouble before it becomes an emergency. This isn’t just about avoiding complications—it’s about knowing when to act, so you and your baby stay safe.
- By Percival Harrington
- /
- 18 Nov 2025
Blood Clots and Pregnancy: What Every Expectant Mother Should Know
Blood clots during pregnancy are rare but dangerous. Learn the real risks, warning signs, and what to do if you're at risk - so you can stay safe and informed.