COVID-19 Vaccine: What You Need to Know About Types, Effects, and Safety
When you get a COVID-19 vaccine, a medical product designed to teach your immune system to recognize and fight the SARS-CoV-2 virus without causing illness. Also known as SARS-CoV-2 vaccine, it’s the most effective tool we have to prevent severe illness, hospitalization, and death from the virus. It’s not magic—it’s science. Your body learns to spot the virus like a security system trained on a photo of a suspect. Once it knows what to look for, it reacts fast if the real thing shows up.
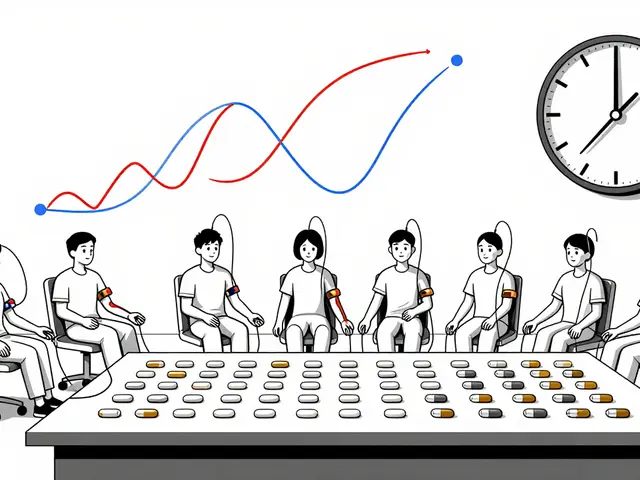
There are a few main types of COVID-19 vaccine, a biological preparation that triggers an immune response against the virus that causes COVID-19. One kind, the mRNA vaccine, a type of vaccine that uses genetic material to instruct cells to make a harmless piece of the virus spike protein. Also known as messenger RNA vaccine, it doesn’t contain the virus at all—just instructions. Your cells read those instructions, make the spike protein, and your immune system learns to attack it. Other vaccines use a harmless virus to deliver those same instructions, or just the spike protein itself. All of them aim for the same result: protection.
Side effects are real, but they’re usually short-lived. Sore arm, tiredness, headache, or fever after the shot? That’s not the virus—it’s your immune system doing its job. Most people feel fine within 48 hours. Serious reactions are rare. The CDC and WHO track every report, and millions of doses have been given worldwide. If you’ve had a severe allergic reaction to a vaccine before, talk to your doctor. Otherwise, the risks of getting COVID-19 far outweigh the risks of the vaccine.
Booster shots aren’t optional extras—they’re updates. Just like your phone gets software patches, your immunity needs refreshers. The virus changes, and the vaccine adapts. The latest boosters target newer strains, giving you better protection when cases rise. You don’t need to wait forever between doses. Timing depends on your age, health, and last shot. Check current guidelines. Delaying a booster doesn’t make you safer—it makes you more vulnerable.
What about long-term effects? We’ve been tracking people for years now. No hidden dangers have shown up. The science behind mRNA vaccines has been studied for decades. The speed of development came from global cooperation and existing research—not cutting corners. If you’re worried about fertility, heart issues, or DNA changes, the data says no link. These myths spread faster than the virus itself, but they’re not backed by science.
People with chronic conditions, older adults, and those with weakened immune systems benefit the most. If you’re on medication for heart disease, diabetes, or autoimmune issues, the vaccine doesn’t interfere with your treatment—it protects you from worse outcomes. Many of the posts below cover how vaccines interact with other drugs, what to watch for after getting them, and how to stay safe if you’re high-risk. You’ll find real stories, practical tips, and clear comparisons—not hype, not fear.
Whether you’re getting your first shot, a booster, or just trying to understand why it matters, this collection gives you the facts you need to make smart choices. No jargon. No fluff. Just what works, what doesn’t, and what you should do next.
- By Percival Harrington
- /
- 18 Nov 2025
Vaccinations While on Immunosuppressants: Live vs Inactivated Guidance 2025
Learn the 2025 guidelines for safe vaccination while on immunosuppressants. Know which vaccines to avoid, when to get them, and how to maximize protection without risking infection.