Formulary Placement: How Drug Coverage Decides What You Pay and Get
When your doctor writes a prescription, what happens next isn’t just about the pill—it’s about formulary placement, where a drug sits on your insurance plan’s approved list, determining cost and access. Also known as drug tiering, it’s the hidden system that decides if your medication is cheap, expensive, or not covered at all. This isn’t just paperwork—it’s the difference between paying $5 or $500 a month for the same drug.
Pharmacy benefits managers, the middlemen between insurers and drug makers, are the ones who decide PBMs where each drug lands on the formulary. They look at price, clinical evidence, and deals drug companies make. A drug with better formulary placement usually means lower co-pays, fewer prior authorizations, and less hassle. But if it’s on a higher tier—or not listed at all—you might need appeals, alternatives, or even pay full price. That’s why drug coverage, the list of medications an insurance plan agrees to pay for matters more than you think. It’s not random. It’s negotiated. And it changes often.
Look at the posts below. You’ll see real cases where formulary placement made a difference: someone on rosuvastatin needing to switch because their insurer moved it to a higher tier; a senior using the Extra Help Program to get Medicare Part D drugs at $0 co-pays; another person struggling to get dimethyl fumarate covered for hives because it’s off-label. These aren’t edge cases—they’re everyday battles shaped by formulary rules. Even Flonase and Astelin face tiering battles. And when you’re on immunosuppressants, your vaccine options can be limited by what’s on the formulary, not just medical need.
Formulary placement doesn’t care about your diagnosis. It cares about cost, contracts, and control. But you can fight back. Know your plan’s formulary. Ask your pharmacist which drugs are preferred. Compare alternatives before your doctor writes the script. The right move could save you hundreds. Below, you’ll find guides that show exactly how to navigate this system—whether you’re on Medicare, dealing with generics, or trying to get a specialty drug covered. This isn’t about luck. It’s about knowing how the system works—and using it to your advantage.
- By Percival Harrington
- /
- 16 Nov 2025
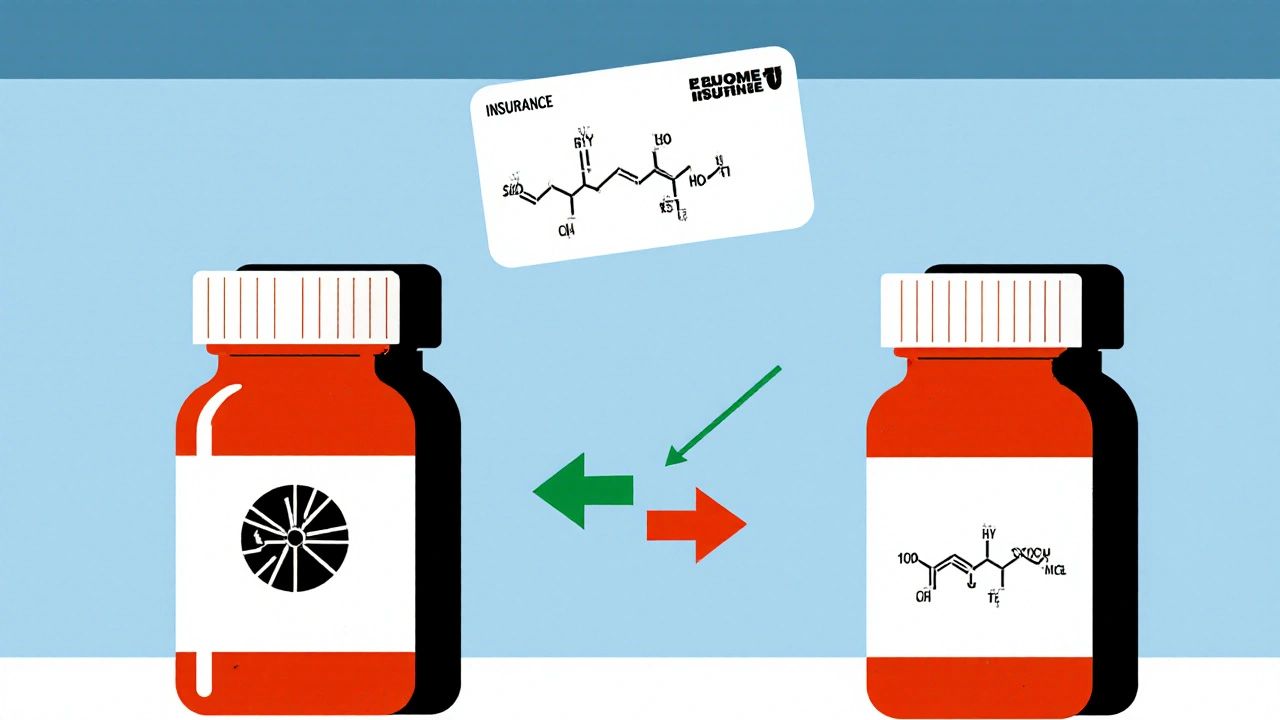
Insurance Coverage of Authorized Generics: How Formulary Placement Affects Your Prescription Costs
Authorized generics offer brand-name drug quality at generic prices, but insurance coverage varies. Learn how formulary placement affects your copays and how to ensure you get the best coverage.