Diabetes Drug Selection Guide
Personalized Diabetes Medication Selection
Answer these questions to get tailored recommendations based on the latest clinical evidence for diabetes medications.
Your Recommendations
Primary Recommendation:
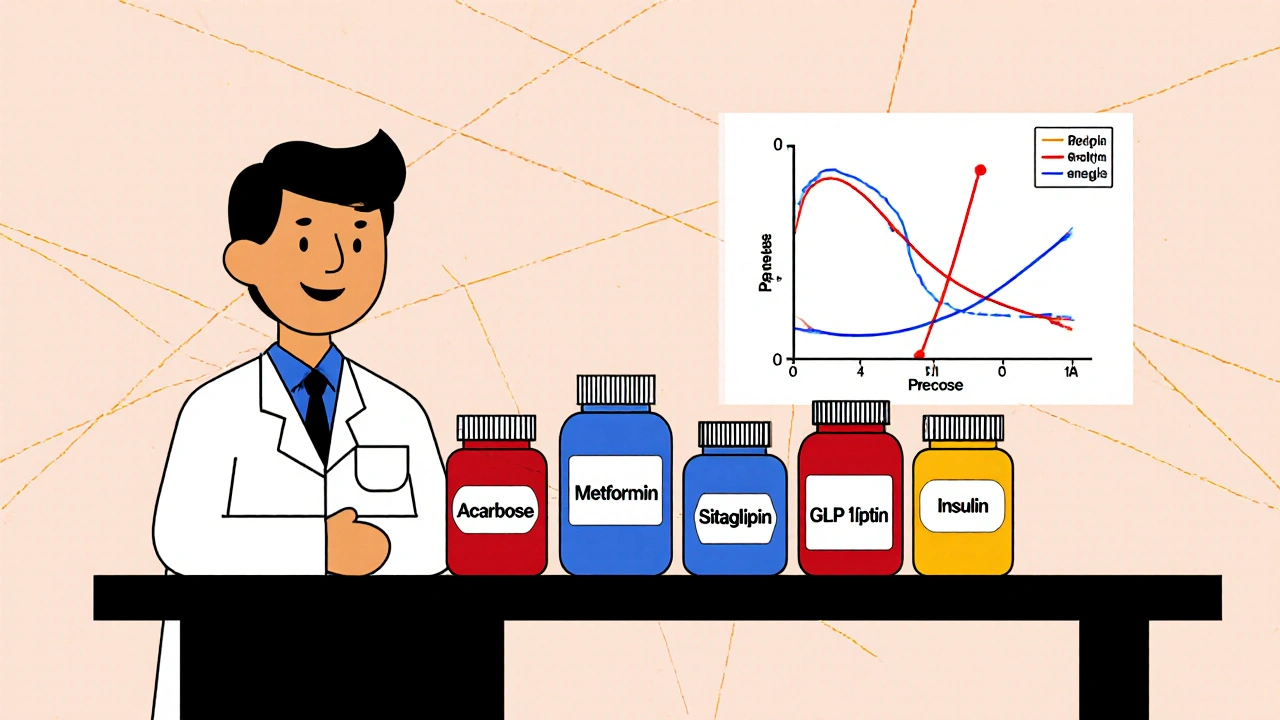
When you or a patient need tighter post‑meal blood‑sugar control, the first drug that often pops up is Precose. But the market is crowded with other options, and knowing which one fits best can feel like solving a puzzle. This guide breaks down Precose (Acarbose) and lines it up against the most common alternatives, so you can decide based on real‑world performance, side‑effect profiles, and practical considerations.
Key Takeaways
- Precose is an alpha‑glucosidase inhibitor that targets post‑prandial glucose spikes.
- Metformin remains the first‑line choice for most people with type 2 diabetes because of its cost, efficacy, and cardiovascular benefits.
- Miglitol and Voglibose are close cousins of Precose, sharing the same mechanism but differing in dosing frequency and tolerability.
- DPP‑4 inhibitors (e.g., Sitagliptin) and GLP‑1 receptor agonists work upstream in the incretin pathway, offering weight‑loss potential.
- Insulin is the most powerful option for severe hyperglycaemia but carries hypoglycaemia risk and requires injection.
Understanding Precose (Acarbose)
Precose (Acarbose) is an oral alpha‑glucosidase inhibitor that slows carbohydrate breakdown in the intestine, reducing the rise in blood glucose after meals. It is usually prescribed at a dose of 25‑100 mg taken three times daily with the first bite of each meal.
The drug’s strength lies in its ability to blunt post‑prandial glucose without causing hypoglycaemia, because it does not increase insulin secretion. However, the very same mechanism can lead to gastrointestinal discomfort, especially when the dose is uptitrated too quickly.
How Alpha‑Glucosidase Inhibitors Work
Alpha‑glucosidase enzymes line the brush border of the small intestine and are responsible for breaking complex carbs into absorbable sugars. By competitively inhibiting these enzymes, drugs like Precose, Miglitol, and Voglibose delay carbohydrate absorption, flattening the post‑meal glucose curve.
This approach is useful for patients whose primary problem is high post‑prandial glucose rather than fasting glucose. It also complements drugs that act on fasting glucose, such as Metformin or insulin.
Major Alternatives - What They Are and When to Use Them
Metformin
Metformin belongs to the biguanide class and works by decreasing hepatic glucose production and improving peripheral insulin sensitivity. It is taken once or twice daily, usually 500‑2000 mg, and is the first‑line therapy for most adults with type 2 diabetes. Its benefits include modest weight loss, low cost, and proven cardiovascular protection.
Miglitol
Miglitol is another alpha‑glucosidase inhibitor, chemically distinct from Acarbose but sharing the same gut‑based mechanism. Typical dosing is 25‑100 mg three times daily with meals. Some patients tolerate Miglitol better because it is less likely to cause flatulence, though it still carries the usual GI side‑effects.
Voglibose
Voglibose is popular in East Asian markets. It is taken at 0.2‑0.3 mg three times daily and has a shorter half‑life than Acarbose, which can make dose timing more forgiving. Its efficacy in lowering post‑prandial glucose is comparable, but data outside Asian populations are limited.
Sitagliptin
Sitagliptin is a DPP‑4 inhibitor that boosts endogenous incretin hormones, increasing insulin secretion only when glucose is high. It is taken once daily at 100 mg and has a very low risk of hypoglycaemia. Weight impact is neutral, and gastrointestinal side‑effects are uncommon.
GLP‑1 Receptor Agonists
Drugs in this class (e.g., exenatide, liraglutide) mimic the action of the incretin GLP‑1, slowing gastric emptying, enhancing insulin release, and promoting satiety. They are administered subcutaneously once daily or weekly. Apart from excellent glucose control, they often lead to weight loss, but they can cause nausea and are pricier.
Insulin
Insulin remains the most potent glucose‑lowering therapy. Basal insulins (e.g., glargine) provide a steady background level, while rapid‑acting analogues (e.g., lispro) cover meals. They are essential when oral agents no longer achieve targets, but they require injection training and carry a risk of hypoglycaemia.
Side‑Effect Profiles at a Glance
| Drug | Class | Key Mechanism | Typical Dose | Main Benefit | Common Side Effects |
|---|---|---|---|---|---|
| Precose (Acarbose) | Alpha‑glucosidase inhibitor | Delays carb absorption | 25‑100 mg TID with meals | Reduces post‑prandial glucose | Flatulence, abdominal pain, diarrhea |
| Metformin | Biguanide | Decreases hepatic glucose output | 500‑2000 mg daily | Lowers fasting & post‑prandial glucose, weight neutral/ loss | GI upset, lactic acidosis (rare) |
| Miglitol | Alpha‑glucosidase inhibitor | Delays carb absorption | 25‑100 mg TID with meals | Post‑prandial control, similar to Acarbose | Flatulence, diarrhea |
| Voglibose | Alpha‑glucosidase inhibitor | Delays carb absorption | 0.2‑0.3 mg TID with meals | Post‑prandial control, shorter half‑life | GI discomfort, less flatulence than Acarbose |
| Sitagliptin | DPP‑4 inhibitor | Increases incretin levels | 100 mg daily | Low hypoglycaemia risk, neutral weight | Headache, nasopharyngitis |
| GLP‑1 agonist (exenatide) | GLP‑1 receptor agonist | Mimics incretin hormone | 5‑10 µg BID (exenatide) | Weight loss, strong HbA1c reduction | Nausea, vomiting, injection site reactions |
| Insulin (glargine) | Long‑acting insulin | Provides basal insulin coverage | 0.1‑0.5 U/kg daily (adjusted) | Potent glucose lowering | Hypoglycaemia, weight gain |
Choosing the Right Drug: Decision Factors
- Efficacy for fasting vs post‑prandial glucose: Metformin excels at fasting glucose; Precose, Miglitol, and Voglibose specialize in post‑meal spikes.
- Weight impact: GLP‑1 agonists promote loss; insulin and some sulfonylureas may cause gain; most others are weight neutral.
- Side‑effect tolerance: Patients with sensitive GI tracts may avoid alpha‑glucosidase inhibitors.
- Cost and access: Metformin and Precose are generic and inexpensive; GLP‑1 agonists and some DPP‑4 inhibitors can be pricey.
- Renal function: Metformin requires dose adjustment below eGFR 30 mL/min; Precose is safe down to eGFR 25 mL/min but watch for hypoglycaemia if combined with sulfonylureas.
- Patient lifestyle: Multiple daily doses (Precose, Miglitol) demand meal timing discipline, whereas once‑daily agents (Metformin XR, Sitagliptin) are simpler.

Practical Tips for Clinicians and Patients
- Start low, go slow with Precose: 25 mg with the first bite, then increase weekly if tolerated.
- Advise patients to spread carbohydrate intake evenly across meals to maximize the drug’s effect.
- Consider adding a probiotic if GI side‑effects become bothersome; evidence shows it can reduce flatulence.
- Monitor HbA1c and 2‑hour post‑prandial glucose together; a drop of 0.5‑1.0% in HbA1c is typical for well‑tolerated Precose.
- When combination therapy is needed, avoid pairing two alpha‑glucosidase inhibitors-no added benefit, just more gut upset.
- Educate patients on recognizing hypoglycaemia signs; although Precose itself doesn’t cause low blood sugar, adding insulin or sulfonylureas does.
Potential Pitfalls and Safety Concerns
Precise dosing is crucial. Taking Acarbose without food defeats its purpose and raises the risk of severe diarrhoea. Also, in patients with pancreatic insufficiency, the slowed carbohydrate breakdown can lead to malabsorption of nutrients.
Renal dosing is an often‑missed detail: if eGFR drops below 30 mL/min, some clinicians discontinue Precose because of limited data on accumulation, even though it isn’t cleared renally. Always check labs before initiating or escalating the dose.
Drug interactions are relatively few, but alpha‑glucosidase inhibitors can blunt the absorption of certain oral antibiotics (e.g., tetracycline) if taken simultaneously. Space them 1‑2 hours apart.
Frequently Asked Questions
Can Precose replace Metformin?
No. Metformin addresses fasting glucose and insulin resistance, while Precose only targets post‑meal spikes. Most guidelines recommend using them together if additional control is needed.
Why do I get gas on Precose?
Acarbose blocks carbohydrate breakdown, leaving more undigested carbs to ferment in the colon. This fermentation produces gas and bloating. Starting with a low dose and gradually increasing helps the gut adapt.
Is Precose safe for people with kidney disease?
It can be used down to an eGFR of about 25 mL/min, but many clinicians stop it below 30 mL/min because data are limited. Always check renal function before prescribing.
How does Precose compare to Miglitol?
Both are alpha‑glucosidase inhibitors with similar efficacy. Miglitol is absorbed systemically and may cause slightly less flatulence, but it also has a shorter half‑life, requiring strict timing with each meal.
When should I consider switching from Precose to a DPP‑4 inhibitor?
If gastrointestinal side‑effects limit adherence or if HbA1c remains above target despite maximized Precose, a DPP‑4 inhibitor like Sitagliptin offers similar glucose control without GI trouble.
Choosing the best diabetes regimen is rarely a one‑size‑fits‑all decision. By understanding how Precose stacks up against its peers, you can match the drug’s strengths to the patient’s profile and avoid unnecessary side‑effects. Keep monitoring, stay flexible, and adjust the plan as the disease evolves.





Write a comment