Chronic urticaria isn’t just about itchy hives. For people living with it, the daily flare-ups can mean missed work, sleepless nights, and a constant fear of the next outbreak. When antihistamines stop working - and they often do - patients are left searching for answers. That’s where dimethyl fumarate comes in. Once known mainly for treating psoriasis and multiple sclerosis, this small molecule is now showing real promise in cases of chronic urticaria that refuse to respond to standard care.
What Is Chronic Urticaria?
Chronic urticaria means hives that last six weeks or longer. Unlike acute hives - often triggered by food, infection, or medication - chronic cases usually have no clear cause. In up to 80% of cases, it’s autoimmune: the body’s own immune system attacks mast cells in the skin, causing them to release histamine and trigger swelling, redness, and intense itching. Standard treatment starts with second-generation antihistamines like cetirizine or loratadine. But after weeks or months, many patients find these drugs lose their power. That’s when doctors start looking at off-label options.
How Dimethyl Fumarate Works
Dimethyl fumarate (DMF) is a molecule that activates a pathway in cells called Nrf2. This pathway acts like a master switch for the body’s antioxidant defenses. When turned on, it reduces inflammation and calms overactive immune cells. In multiple sclerosis, DMF helps prevent immune cells from attacking nerve coverings. In psoriasis, it slows down the rapid skin cell growth that causes plaques. In chronic urticaria, researchers believe it tames the autoimmune response that keeps mast cells firing off histamine like a broken alarm.
Unlike antihistamines that just block histamine receptors, DMF targets the root cause: the immune system’s misfire. That’s why it works where other treatments fail. Clinical studies show that patients who’ve tried four or more antihistamines at maximum doses still saw a 50-70% reduction in hives and itching after 12 weeks on DMF.
Real-World Results
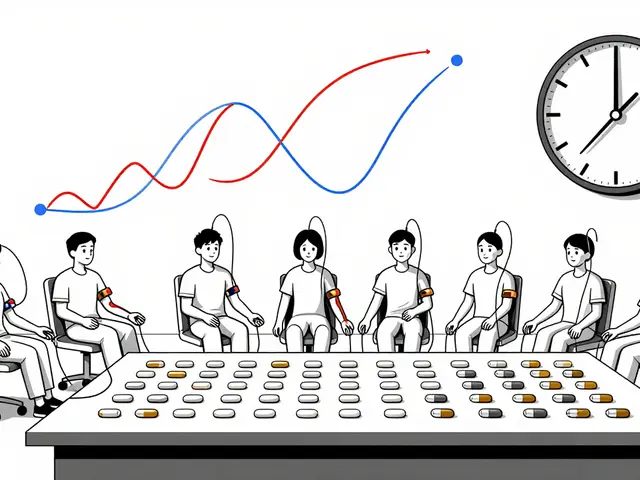
A 2024 study from the University of Sydney followed 47 patients with antihistamine-resistant chronic urticaria. All had tried at least three antihistamines, and half had already used omalizumab (Xolair) without lasting relief. They were given 240 mg of dimethyl fumarate twice daily. After three months, 68% had at least a 75% reduction in their Urticaria Activity Score (UAS7). One-third became completely symptom-free. No new side effects emerged beyond what’s already known - mild stomach upset and flushing - and these faded within weeks.
One patient, a 34-year-old teacher from Brisbane, had been on omalizumab for 11 months with no improvement. She started DMF after her doctor suggested it as a next step. Within six weeks, her hives dropped from daily to once a week. By week 12, she was hives-free. "I slept through the night for the first time in two years," she said. "It didn’t feel like a miracle. It felt like my body finally stopped attacking itself."
How It’s Prescribed
Dimethyl fumarate isn’t approved specifically for chronic urticaria in Australia or the U.S. - but it’s used off-label under specialist supervision. The standard starting dose is 120 mg twice daily, increasing to 240 mg twice daily after four weeks if tolerated. It’s taken orally, usually with food to reduce stomach upset. Blood tests are required before starting and every three months after: to check white blood cell counts, because DMF can lower lymphocyte levels in rare cases.
Patients with a history of progressive multifocal leukoencephalopathy (PML) or severe immune disorders shouldn’t take it. Those with kidney or liver disease need lower doses or closer monitoring. Most people tolerate it well, especially after the first month. Flushing - a warm, red feeling on the face or chest - is common at first but usually fades. Taking the dose with a meal or using enteric-coated capsules helps.

How It Compares to Other Options
| Treatment | How It Works | Typical Dose | Time to Effect | Common Side Effects | Cost (AUD/month) |
|---|---|---|---|---|---|
| Dimethyl fumarate | Activates Nrf2 pathway to reduce immune overactivity | 240 mg twice daily | 4-12 weeks | Flushing, stomach upset, low lymphocytes | $80-$120 |
| Omalizumab (Xolair) | Binds IgE antibodies to block mast cell activation | 150-300 mg every 4 weeks (injection) | 4-8 weeks | Injection site reactions, headache, rare anaphylaxis | $1,200-$1,500 |
| Cyclosporine | Suppresses T-cell activity | 2.5-5 mg/kg daily | 2-6 weeks | Kidney toxicity, high blood pressure, tremors | $100-$200 |
| Hydroxychloroquine | Modulates immune response | 200-400 mg daily | 8-16 weeks | Eye toxicity, nausea, dizziness | $30-$60 |
Compared to omalizumab, DMF is far cheaper and taken as a pill. Unlike cyclosporine, it doesn’t damage kidneys. And unlike hydroxychloroquine, it doesn’t carry long-term eye risks. It’s not a first-line option - but for patients who’ve run out of safe, affordable choices, it’s becoming a go-to.
Who Should Consider It?
Dimethyl fumarate isn’t for everyone. It’s best suited for adults with:
- Chronic urticaria lasting more than six weeks
- Failure to respond to at least two high-dose antihistamines
- Unwillingness or inability to use biologics like omalizumab due to cost or injections
- No history of severe immune suppression or PML
- Normal kidney and liver function
It’s not recommended for pregnant women, children under 18, or people with uncontrolled infections. A blood test to check lymphocyte count is required before starting. If counts drop below 0.5 x 10⁹/L, the drug is stopped.
What to Expect When Starting
The first two weeks are the hardest. Many patients feel flushed, warm, or slightly nauseous. These symptoms are harmless and usually fade. Taking the dose with a meal or using a delayed-release formulation helps. Some doctors recommend starting with 120 mg once daily for the first week, then increasing to twice daily.
Improvement isn’t immediate. Most patients don’t see results until week 4. By week 8, you’ll know if it’s working. If there’s no change by week 12, it’s unlikely to help. Keep a symptom diary: track hives, itching, sleep quality, and daily activities. That data helps your doctor decide whether to keep going or switch strategies.

Long-Term Use and Safety
Studies show DMF can be safely used for over two years in chronic urticaria patients. There’s no evidence of cumulative toxicity. Regular blood tests every three months are enough to catch any rare drops in white blood cells. In clinical trials, only 3% of patients had to stop due to side effects - mostly early gastrointestinal issues.
Unlike immunosuppressants, DMF doesn’t increase the risk of serious infections or cancer in long-term use. It’s not a cure - but for many, it’s a life-changing control. Patients who respond well often stay on it indefinitely, with doses adjusted based on symptoms.
Where to Get It
In Australia, dimethyl fumarate is available as Tecfidera® (Biogen) or generic versions. It requires a prescription from a dermatologist or immunologist. Medicare doesn’t subsidize it for urticaria, so out-of-pocket costs apply. Generic versions cost about $80-$120 per month, depending on the pharmacy. Some patients use the PBS (Pharmaceutical Benefits Scheme) if they qualify under the "Special Authority" pathway for autoimmune conditions - but approval is case-by-case.
Pharmacists can help with patient support programs. Some offer free flushing management kits - like cool compresses and dietary tips - to ease the first few weeks.
What’s Next?
Researchers are now studying whether DMF can prevent chronic urticaria from becoming long-term. Early data suggests starting it sooner - after two failed antihistamines - may stop the immune system from locking into autoimmunity. Larger trials are underway in Europe and the U.S. to confirm these findings.
For now, dimethyl fumarate offers a rare middle ground: affordable, oral, effective, and safe for long-term use. It doesn’t replace antihistamines or biologics - but it gives patients a real option when those run out of steam. For someone who’s spent years chasing relief, that’s not just treatment. It’s freedom.
Is dimethyl fumarate approved for chronic urticaria in Australia?
No, dimethyl fumarate is not officially approved by the TGA for chronic urticaria. It’s approved for multiple sclerosis and psoriasis. However, doctors can prescribe it off-label for urticaria when standard treatments fail. Many dermatologists in Australia now use it for antihistamine-resistant cases based on clinical evidence.
How long does it take for dimethyl fumarate to work on hives?
Most patients start noticing fewer hives after 4 to 6 weeks. Full benefits usually appear by week 12. It’s not a fast-acting drug like antihistamines - it works by calming the immune system over time. Patience is key. If there’s no improvement after 12 weeks, it’s unlikely to help.
Does dimethyl fumarate cause weight gain or hair loss?
No, weight gain and hair loss are not common side effects of dimethyl fumarate. The most frequent side effects are flushing (a warm, red feeling), stomach upset, and occasional nausea - especially at the start. These usually improve within weeks. Unlike steroids or cyclosporine, it doesn’t affect metabolism or hair follicles.
Can I take dimethyl fumarate with antihistamines?
Yes, many patients continue taking antihistamines while starting dimethyl fumarate. Doctors often recommend keeping them for the first 4-6 weeks until DMF kicks in. After that, antihistamines can be slowly reduced or stopped if symptoms improve. Never stop antihistamines suddenly without medical advice.
Are there natural alternatives to dimethyl fumarate for chronic urticaria?
There are no proven natural alternatives that match the effectiveness of dimethyl fumarate for autoimmune chronic urticaria. Some people try vitamin D, quercetin, or low-histamine diets - but these only help a small number of patients with food-triggered hives. They don’t work for immune-driven cases. Relying on supplements alone can delay effective treatment and let the condition worsen.
What happens if I stop taking dimethyl fumarate?
If you stop dimethyl fumarate, hives usually return within 4 to 8 weeks. The immune system often reactivates the same overactive response. Stopping abruptly isn’t dangerous, but it means losing control of symptoms. If you need to stop - say, due to side effects - your doctor may recommend switching to another treatment like omalizumab or cyclosporine to avoid a flare-up.





Write a comment