Medication Monitoring Calculator
Select Your Medication
Recommended Monitoring Schedule
How often should you monitor?
Important: Your doctor may adjust this based on your specific health status, other medications, and initial results.
Every year, millions of people take medications that help them live better, longer lives. But for many, those same drugs come with unexpected and sometimes dangerous side effects. The problem isn’t always the medicine itself-it’s that we wait too long to notice the warning signs. By the time a patient reports dizziness, rash, or fatigue to their doctor, the damage might already be done. The good news? We don’t have to wait. With the right routine monitoring, you can catch side effects early-before they become emergencies.
Why Waiting Is Dangerous
Clinical trials are the first place we learn about a drug’s safety. But here’s the catch: those trials involve a few hundred, maybe a few thousand people. Real life? Millions take the same drug, often with other medications, different diets, or underlying conditions the trials never tested. That’s why some side effects only show up after a drug hits the market. The FDA’s Adverse Event Reporting System (FAERS) has collected reports from over 11 million patients since 2019, but experts say less than 6% of serious reactions ever make it into the system. Most people don’t report them. They assume the nausea is just a stomach bug. Or the swelling is from standing too long. Or the mood swings are stress.That’s why routine monitoring isn’t optional-it’s essential. You can’t rely on patients to remember to call their doctor every time something feels off. You can’t wait for a doctor to spot a pattern in a 20-minute visit. You need systems that catch the early signals-before they turn into hospital visits.
What Tests and Checks Should You Be Doing?
Not every medication needs the same monitoring. But most long-term drugs require some form of tracking. Here’s what’s commonly used:- Blood tests for drugs like warfarin, lithium, or statins. These check how your body is processing the drug and whether levels are in the safe range. For example, lithium levels above 1.5 mmol/L can cause tremors, confusion, or even kidney damage.
- Liver function tests for medications like acetaminophen, certain antibiotics, or anticonvulsants. Elevated liver enzymes can signal trouble before you feel symptoms.
- Kidney function tests (creatinine, eGFR) for diabetes drugs, blood pressure meds, or NSAIDs. Poor kidney clearance can lead to drug buildup and toxicity.
- Electrocardiograms (ECGs) for drugs that affect heart rhythm, like some antidepressants or antipsychotics. QT prolongation can lead to dangerous arrhythmias.
- Blood pressure and heart rate checks for beta-blockers, stimulants, or decongestants. Small changes over time can signal intolerance.
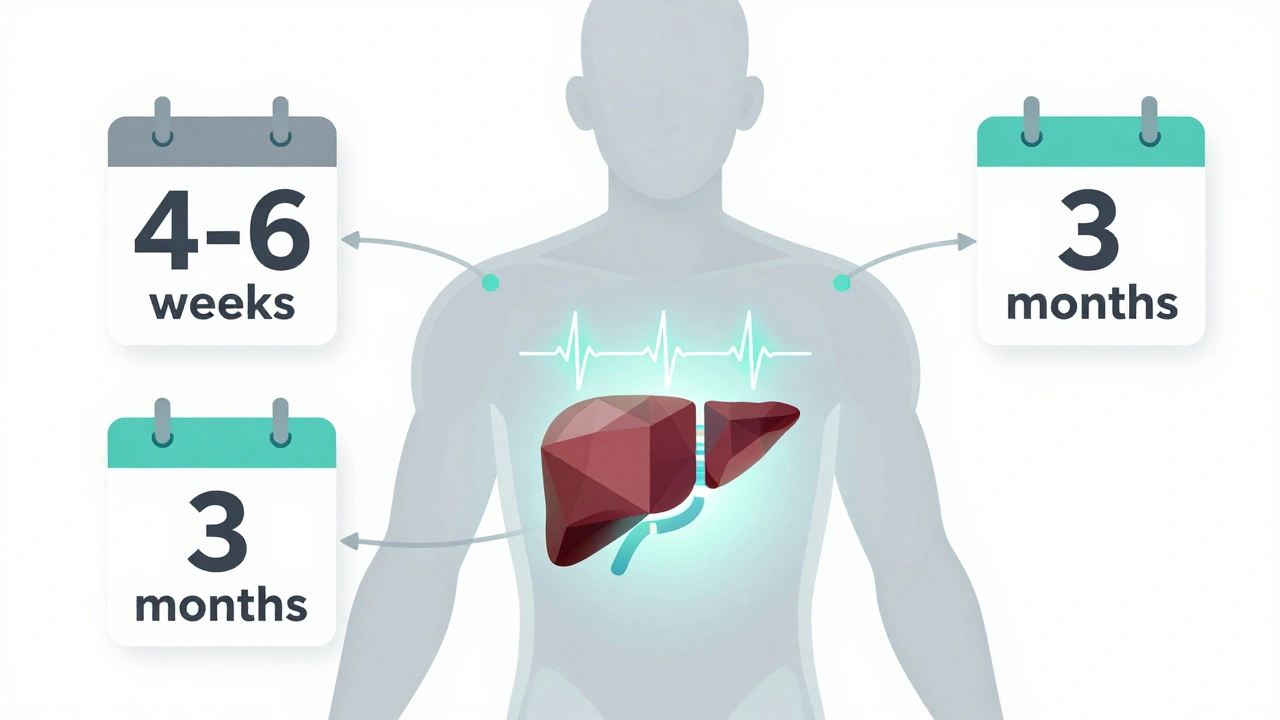
Timing matters. For example, if you start a new statin, your doctor might order a liver test after 4-6 weeks. For lithium, blood levels are checked every 3-6 months once stable. Some drugs, like methotrexate, require monthly blood counts because they can suppress bone marrow. Don’t assume your doctor will bring it up. Ask: “What tests should I be getting, and how often?”
How Technology Is Changing the Game
For years, monitoring relied on patients remembering symptoms and doctors spotting patterns. Now, technology is stepping in. Stanford University researchers found that by analyzing unstructured notes in electronic health records-things like “patient says dizzy since starting new pill”-they could detect side effects nearly two years before the FDA issued official warnings. This isn’t science fiction. It’s happening in hospitals right now.These systems use natural language processing to scan thousands of clinical notes for keywords like “nausea,” “rash,” or “fatigue” linked to specific drugs. They don’t wait for someone to file a report. They look at what’s already being written during routine visits. This method caught rare side effects of drugs like Semagacestat before they were even officially recognized in clinical trials.
Another tool, called Clinical Decision Support Systems (CDSS), pops up alerts when a doctor prescribes a new drug that might interact with something the patient is already taking. For older adults on five or more medications, this isn’t a luxury-it’s a lifesaver. One study showed CDSS reduced potentially dangerous drug interactions by 30% in just six months.
What You Can Do at Home
You don’t need a hospital to start monitoring. Simple habits make a huge difference:- Keep a symptom log. Write down when you feel off: date, time, what you took, how bad it is (use a 1-10 scale), how long it lasted, and anything else going on-did you drink alcohol? Skip a meal? Sleep poorly?
- Track changes. Did your sleep get worse after starting a new blood pressure pill? Did your appetite drop after a new antidepressant? These aren’t random. They’re signals.
- Don’t ignore “weird” symptoms. A metallic taste, sudden weight gain, or blurred vision might not seem like a big deal. But if they started after a new drug, they could be the first sign of a side effect.
- Use a pill organizer with reminders. Taking meds at the wrong time can increase side effects. Consistency helps your body adjust.
Patients who kept detailed logs were 40% more likely to catch side effects early, according to a study by Bocapharmacygroup. That’s not because they were paranoid-it’s because they had data. When they went to the doctor, they didn’t say, “I think something’s wrong.” They said, “Here’s what happened, when, and how often.” That changes everything.
Why Polypharmacy Makes Monitoring Crucial
As we age, we often need more medications. One for blood pressure. One for cholesterol. One for arthritis. One for sleep. One for depression. That’s called polypharmacy. And it’s the biggest hidden risk in modern medicine.Drug interactions don’t always show up in trials. Two drugs that are safe alone can be dangerous together. For example, combining a statin with certain antibiotics can cause muscle damage. Mixing blood thinners with NSAIDs increases bleeding risk. These aren’t rare. They’re common. And they’re often missed because doctors focus on one condition at a time.
That’s why regular medication reviews are non-negotiable. Every six months, ask your doctor or pharmacist: “Do I still need all these? Could any be causing my symptoms?” Many older adults are on drugs they haven’t needed for years. Stopping one can eliminate multiple side effects at once.
What’s Next? The Future of Monitoring
The next wave of monitoring is already here. Wearables can track heart rate variability, sleep quality, and activity levels-changes that might signal a drug’s effect before you even feel it. Apps that let you log symptoms in real time are becoming more accurate. AI tools are learning to predict side effects based on your genetics, age, and other meds-even before you start the drug.The goal isn’t to scare you. It’s to empower you. Medications save lives. But they’re not harmless. The key is catching problems early, before they spiral. That means trusting your body, tracking your symptoms, asking questions, and using the tools available-whether it’s a blood test, a symptom log, or an AI alert from your doctor’s system.
You don’t have to be a scientist to do this. You just have to be consistent. Because when it comes to your health, the best early warning system isn’t a machine. It’s you-with your eyes open and your notebook ready.
How often should I get blood tests when taking medication?
It depends on the drug. For example, lithium and warfarin usually need blood tests every 3-6 months once stable. Statins often require a liver test after 4-6 weeks, then annually. Anticonvulsants like valproate may need monthly checks at first, then every 3-6 months. Always ask your doctor for the specific schedule tied to your medication.
Can I rely on my doctor to catch side effects during visits?
Not always. Doctors have 15-20 minutes per visit and are often focused on managing your main condition. Side effects can be subtle or mistaken for other issues. If you feel something’s off, don’t wait for them to ask. Bring your symptom log and say, “I’ve noticed this since starting the new med-could it be related?”
Are side effects always a sign I should stop the medication?
No. Some side effects are mild and go away as your body adjusts-like nausea from metformin or drowsiness from certain antidepressants. But others, like swelling, chest pain, or unusual bleeding, need immediate attention. Never stop a medication without talking to your doctor. They can adjust the dose, switch drugs, or add a counter-treatment.
What’s the biggest mistake people make with medication monitoring?
Waiting until symptoms are severe before saying anything. Many people think side effects mean they’re doing something wrong. They don’t realize it’s a normal part of medication use. The best approach is to track early, even if it’s just a mild headache or dry mouth. Small patterns matter.
Can technology really predict side effects before they happen?
Yes, in some cases. AI models trained on millions of patient records can predict which patients are more likely to develop side effects based on their age, other meds, genetics, and medical history. For example, Stanford’s system flagged rare reactions to Semagacestat before clinical trials even confirmed them. These tools aren’t perfect, but they’re getting better-and they’re already helping doctors make safer decisions.
What to Do Next
Start today. Grab a notebook or open a notes app. Write down every medication you’re taking-name, dose, time of day. Then, for the next two weeks, note any changes in how you feel: sleep, energy, digestion, mood, skin, or pain. Bring it to your next appointment. Ask: “Could any of these be side effects?” That simple step could prevent a hospital visit down the line.Medication isn’t magic. It’s chemistry. And chemistry has rules. The more you understand those rules-and how your body responds-the safer you’ll be. You’re not just taking pills. You’re managing your health. And that starts with paying attention.






Write a comment