Imagine this: You pick up your child’s liquid antibiotics, and the pharmacist hands you a syringe with 5 mL marked on it. The prescription says 0.5 mL. You don’t think twice. You give it to your kid. Within hours, they’re vomiting, lethargic, and rushed to the ER. That’s not a horror story-it’s a real event that happened in a Sydney pharmacy in 2022. The error? A simple failure to double-check the strength and quantity of the medication before handing it over.
This isn’t rare. Every year, thousands of patients in Australia and the U.S. suffer harm because someone skipped the last, critical step before dispensing: verifying the exact amount of drug in the container and whether it matches the prescription. It’s not about being lazy. It’s about workflow pressure, outdated labels, and assumptions that cost lives.
Why Strength and Quantity Are Not the Same Thing
Here’s where most mistakes happen: confusing strength with quantity. Let’s say a prescription reads: “Amoxicillin 125 mg/5 mL, dispense 10 mL.” The strength is 125 mg per 5 mL. The quantity dispensed is 10 mL total. That means the patient gets 250 mg total. If the pharmacist misreads the strength as the total amount-thinking “125 mg” means the whole bottle has only 125 mg-they’ll dispense half the dose. Or worse, if they think the strength is the total, they might give 125 mL instead of 10 mL. That’s a 12-fold overdose.
The FDA and USP made this crystal clear in 2019: “The total amount of drug in the container must be the most prominent number on the label.” That means if a bottle says “125 mg/5 mL,” the “10 mL” should be bigger, bolder, and easier to see than the “125 mg/5 mL.” But many pharmacies still use old labels. In fact, a 2022 study found that 64% of liquid medication labels in community pharmacies still buried the total quantity under smaller print. That’s a recipe for disaster.
The Three Steps That Stop Errors Before They Happen
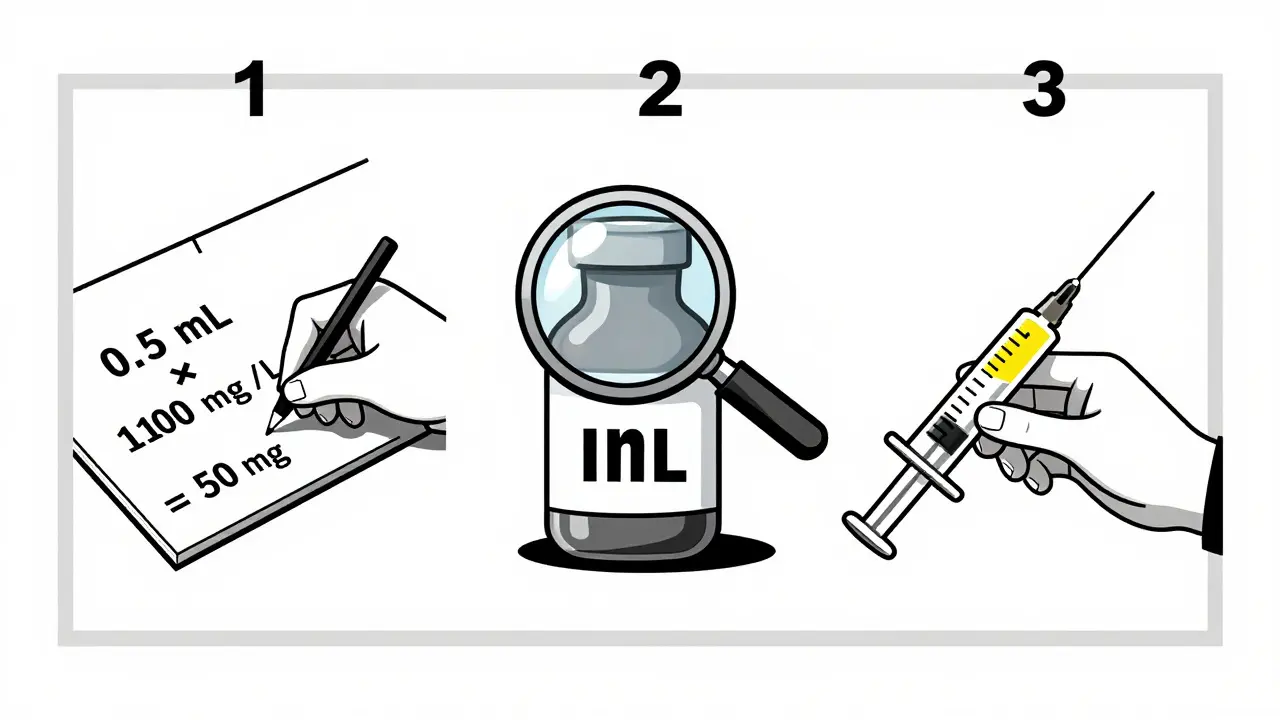
There’s no magic tool or app that replaces human verification. But there is a proven, three-step method used by top-performing pharmacies:
- Independent recalculation. Don’t just look. Do the math. If the prescription says “Take 0.5 mL twice daily,” and the bottle says “100 mg/mL,” calculate: 0.5 mL × 100 mg/mL = 50 mg per dose. Then check: does the total volume in the bottle match the total prescribed? If the prescription is for 10 days, total volume should be 10 mL. If you get a 20 mL bottle, ask why.
- Visual cross-check. Hold the bottle up. Look at the label. Is the total amount written in bold, large font? Is it the first thing you see? If not, it’s a red flag. The USP requires this font size to be at least 50% larger than the concentration. Many pharmacies still don’t comply.
- Device match. Never hand out a teaspoon. Ever. A teaspoon holds 5 mL. A tablespoon holds 15 mL. Parents use them because they’re in the kitchen. But 93% of pediatric dosing errors come from this confusion. Use an oral syringe. Always. For doses under 10 mL, it’s the only safe option. The NCPDP says so. The FDA says so. Your patient’s life says so.
These steps aren’t optional. They’re the difference between a patient going home and a patient going to the ICU.
What Happens When You Skip the Check
Let’s look at real numbers. According to the Institute for Safe Medication Practices (ISMP), double-checking strength and quantity prevents 87% of errors involving high-alert drugs like insulin, opioids, and anticoagulants. These are the drugs that kill when dosed wrong.
In 2023, the FDA reported 37 cases of fatal overdoses linked to misreading strength vs. quantity. One involved a 78-year-old man who received 50 mL of a liquid morphine solution labeled “10 mg/mL.” The prescription was for 5 mL. He got 500 mg instead of 50 mg. He died within 12 hours.
And it’s not just hospitals. Community pharmacies in Australia and the U.S. see 6.2 errors per 10,000 prescriptions when they follow ISMP’s 2023 protocol. Without it? 28.7 errors per 10,000. That’s nearly five times more mistakes. And in independent pharmacies with fewer than five staff, 68% admit they skip the full check during rush hours. Why? Because corporate targets demand 35+ prescriptions per hour. That’s one every 1.7 minutes. There’s no time for math.

The Technology That Helps (But Doesn’t Replace) Human Judgment
Barcode scanning cuts dispensing errors by 83%. That sounds great. But here’s the catch: it only works if the barcode data is correct. If the label says “125 mg/5 mL” but the system thinks it’s “125 mg total,” the scanner will approve a wrong dose. Technology doesn’t fix bad labeling. It just makes bad labeling faster.
That’s why the best systems combine tech with human steps. A pharmacist scans the bottle. The system says “OK.” Then they do the math. Then they check the label font. Then they hand the patient an oral syringe. That’s the gold standard.
And here’s something most people don’t know: the DEA requires pharmacists to sign off on controlled substance verification. That means for opioids and sedatives, the second check isn’t just best practice-it’s the law. Skip it, and you’re not just risking a patient’s life. You’re risking your license.
What Patients Can Do to Protect Themselves
You don’t have to be a pharmacist to catch a mistake. Here’s what you can do:
- Ask: “How much total medicine is in this bottle?” If they say “125 mg,” they’re giving you the strength, not the quantity. Push back. Ask for the total volume.
- Ask: “Do you have an oral syringe?” If they say “Here’s a spoon,” say no. Walk out. Come back later. Find another pharmacy.
- Check the label. Is the total amount bigger than the concentration? If not, ask why.
- For children: Always ask for the syringe. Never trust a teaspoon.
One mother in Melbourne told her pharmacist: “I don’t understand this. The label says 5 mL, but the prescription says 0.5 mL.” The pharmacist paused. Ran the numbers. Realized they’d dispensed 10 times too much. They recalled the medication. The child was fine. That’s what happens when someone asks.
The Future Is Clear: Standardized Labels, Standardized Devices
The FDA’s 2023 draft guidance requires all injectable and liquid medications to display total drug amount in bold, 50% larger font by Q3 2025. That’s huge. It means the problem is being addressed at the source.
Meanwhile, the National Coordinating Council for Medication Error Reporting (NCCMERP) is pushing for all e-prescribing systems to show total quantity first. That’s a game-changer. If your doctor’s software prints “10 mL” before “125 mg/mL,” the pharmacist sees it immediately.
And it’s working. Pharmacies that implemented full double-check protocols saw a 78% drop in strength-related errors. One independent pharmacy in Perth cut their errors from 1.2% to 0.15% in six months. All they did was add a checklist. Train their techs. And refuse to rush.
This isn’t about perfection. It’s about consistency. One extra 45 seconds per prescription. One extra question. One extra syringe. That’s all it takes.
Why is the total amount of medication more important than the strength per mL?
The strength per mL (like 10 mg/mL) tells you how concentrated the drug is. But the total amount (like 50 mL) tells you exactly how much the patient gets. If you give someone 50 mL of a 10 mg/mL solution, they get 500 mg total. If you mistakenly think the strength is the total, you might give them 10 mg instead of 500 mg-or worse, 500 mg when they only needed 50 mg. Confusing the two has led to fatal overdoses and underdoses. That’s why labeling rules now require the total amount to be the biggest, boldest number on the bottle.
Can barcode scanning prevent all medication errors?
No. Barcode scanning only checks if the bottle matches the prescription in the system. If the system has the wrong data-like listing 125 mg as the total instead of 125 mg per mL-the barcode will still scan as correct. That’s why independent verification is still required. Technology helps, but it doesn’t replace human judgment. The best systems use barcodes as a first step, then add manual math and label checks.
Why shouldn’t I use a teaspoon to give liquid medicine to my child?
A household teaspoon holds anywhere from 3 mL to 7 mL-it’s not standardized. A tablespoon holds even more. But oral syringes are calibrated in precise 0.1 mL increments. Studies show 93% of pediatric dosing errors happen because parents use spoons. One study found a parent gave 5 mL thinking it was 0.5 mL because they used a teaspoon. The child ended up in the hospital with liver damage. Always use the syringe the pharmacy gives you.
Is double-checking required by law in Australia?
While not written into federal law, double-checking medication strength and quantity is required under the Therapeutic Goods Administration’s (TGA) Code of Good Pharmacy Practice. Pharmacists must ensure prescriptions are accurately dispensed. Failure to verify can lead to disciplinary action, loss of license, or liability in court if harm occurs. Many Australian pharmacies follow ISMP’s 2023 guidelines as best practice, and insurers require it.
What should I do if I think the pharmacy gave me the wrong amount?
Stop. Don’t take it. Call the pharmacy back. Ask them to recheck the prescription, the bottle label, and the total volume. If they dismiss you, go to another pharmacy and ask them to verify. You have the right to ask. In fact, asking could save a life-your own or someone else’s. Document what you were told. If harm occurs, that record matters.
Final Thought: It’s Not Just a Step. It’s a Lifeline.
Medication errors don’t happen because someone is evil. They happen because systems are rushed, labels are confusing, and people are tired. But every time a pharmacist stops, looks, calculates, and hands over a syringe instead of a spoon-they’re not just following procedure. They’re choosing to protect someone. And that choice? It’s the most powerful one in healthcare.