Blood Pressure & Atrial Fibrillation Risk Calculator
Blood Pressure Categories & AF Risk
| Category | Systolic (mmHg) | Diastolic (mmHg) | Relative AF Risk |
|---|---|---|---|
| Normal | <120 | <80 | Baseline |
| Elevated | 120–129 | <80 | +9% |
| Stage 1 Hypertension | 130–139 | 80–89 | +22% |
| Stage 2 Hypertension | ≥140 | ≥90 | +48% |
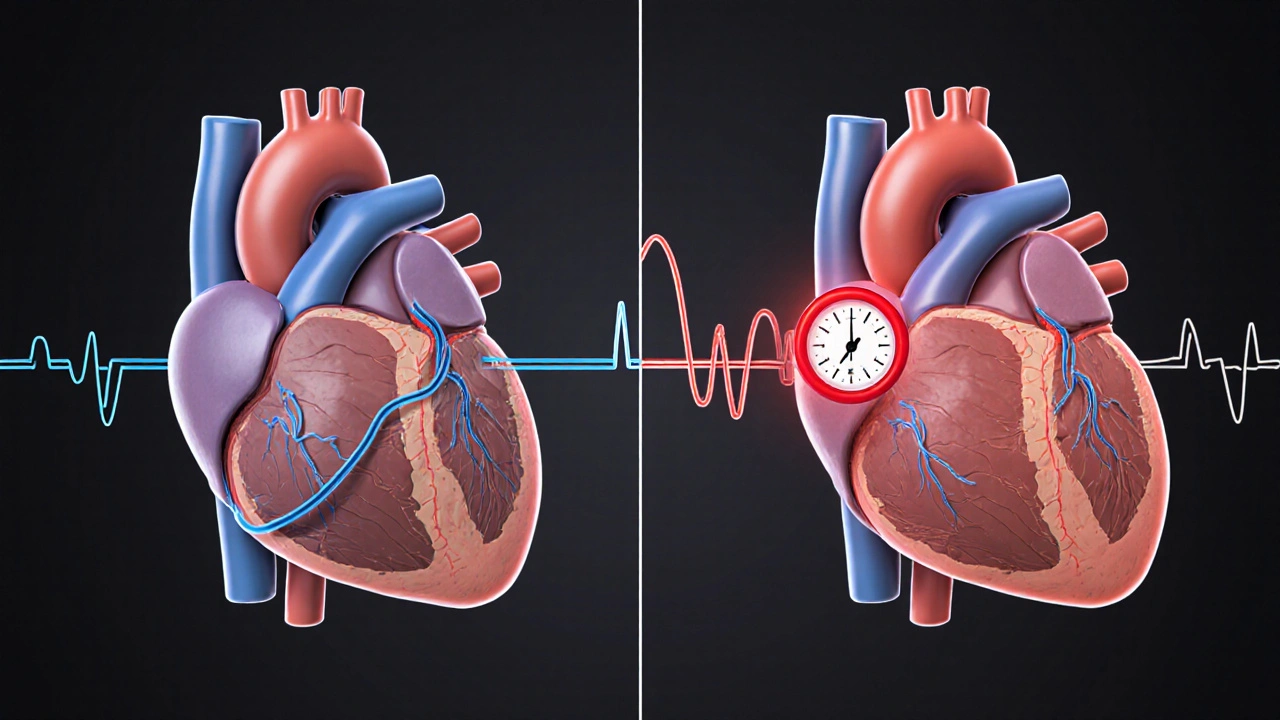
When you hear the terms atrial fibrillation a common heart rhythm disorder where the upper chambers quiver instead of beating in sync and blood pressure the force of blood pushing against artery walls during each heartbeat, it’s easy to think they belong to separate health conversations. In reality, they’re tightly linked, and the pressure you carry in your arteries can tip the balance toward irregular heartbeats, strokes, and a cascade of other problems. This guide untangles that connection, shows why it matters, and gives you clear steps to keep both numbers in check.
Why Blood Pressure and Atrial Fibrillation Talk to Each Other
High blood pressure, or hypertension a chronic condition where systolic or diastolic readings consistently exceed normal limits, forces the heart to work harder. Over time, the left atrium stretches, its electrical pathways become erratic, and the chance of developing atrial fibrillation (AF) climbs. Studies from the American Heart Association in 2023 showed that each 10‑mmHg rise in systolic pressure nudges AF risk up by about 12%.
Think of the heart as a rubber band. Normal pressure lets it snap back cleanly. Push the pressure too high, and the band loses its elasticity, leading to wobble-exactly what AF looks like on an ECG.
How AF Changes Blood Pressure (And Vice‑versa)
AF doesn’t just sit idle; it can cause blood pressure to swing wildly. When the atria fail to pump efficiently, blood pools, raising left‑ventricular filling pressures. The body reacts by sharpening the sympathetic nervous system, which spikes blood pressure. That spike can start a vicious loop: higher pressure → more atrial stretch → worse AF.
Conversely, controlling blood pressure can blunt that loop. Lowering systolic numbers reduces atrial wall stress, giving the electrical system a chance to re‑stabilize.
Key Numbers: Blood Pressure Categories and AF Risk
| Category | Systolic (mmHg) | Diastolic (mmHg) | Relative AF Risk* |
|---|---|---|---|
| Normal | <120 | <80 | Baseline |
| Elevated | 120‑129 | <80 | +9% |
| Stage1 Hypertension | 130‑139 | 80‑89 | +22% |
| Stage2 Hypertension | ≥140 | ≥90 | +48% |
*Relative risk compared to people with normal blood pressure, based on pooled cohort data from 2018‑2022.

Health Consequences of the AF‑Blood Pressure Duo
- Stroke a sudden interruption of blood flow to the brain, often caused by clots that form in the atria during AF. High pressure speeds clot formation and makes emboli larger.
- Heart failure: Persistent high pressure and irregular rhythm weaken the pumping ability of the heart.
- Kidney damage: Both conditions strain the kidneys’ tiny filters, accelerating chronic kidney disease.
Managing Blood Pressure to Reduce AF Episodes
Below is a step‑by‑step plan that blends medication, lifestyle tweaks, and monitoring. Follow each step consistently, and you’ll give your heart a fighting chance.
- Get an accurate baseline. Use a validated home cuff, measure twice daily (morning & evening) for a week, and record the average.
- Beta blockers medications that slow heart rate and lower blood pressure by blocking adrenaline are often first‑line for AF patients with hypertension. Discuss dosage with your cardiologist a heart specialist trained to manage rhythm disorders.
- Anticoagulants drugs that thin the blood to prevent clot formation, crucial for AF patients. Blood pressure control lowers the dose needed for some newer agents.
- Adopt lifestyle modification dietary and activity changes shown to lower blood pressure and improve heart rhythm.
- Salt intake: Keep below 1,500mg per day.
- Potassium‑rich foods (bananas, spinach) help relax vessel walls.
- 30 minutes of moderate aerobic exercise most days - walking, cycling, swimming.
- Weight loss: Every 10lb dropped can shave 5‑mmHg off systolic pressure.
- Monitor heart rhythm. Wearable ECG patches or a handheld device can flag early AF episodes before they spike blood pressure.
- Follow up regularly. Quarterly visits allow your doctor to adjust meds based on the latest BP and rhythm readings.
Common Pitfalls and How to Avoid Them
- Skipping medication after feeling better - blood pressure can rise silently; keep the regimen even if numbers look fine.
- Relying on office measurements only - white‑coat effect can mask true pressure; home tracking is essential.
- Ignoring alcohol - even moderate drinking raises atrial pressure and can trigger AF.
- Over‑exercising without warm‑up - sudden spikes in heart rate may precipitate AF in hypertensive patients.

When to Seek Immediate Care
If you experience any of the following, call emergency services:
- Sudden, severe chest discomfort combined with a rapid, irregular heartbeat.
- Weakness or numbness on one side of the body - possible stroke.
- Shortness of breath that worsens quickly.
These signs suggest a clot may have escaped the heart or that blood pressure has surged to dangerous levels.
Bottom Line: Keep the Pressure Low, Keep the Rhythm Steady
Understanding the two‑way street between blood pressure and atrial fibrillation empowers you to act before complications arise. By measuring accurately, sticking to medication, and embracing heart‑healthy habits, you can lower your stroke risk, preserve heart function, and enjoy a more stable rhythm.
Frequently Asked Questions
Can normal blood pressure still lead to atrial fibrillation?
Yes, but the risk is much lower. Even people with "normal" readings can develop AF due to genetics, sleep apnea, or other factors. Maintaining the lower end of normal (e.g., 110/70mmHg) still offers protective benefits.
Do blood‑pressure‑lowering drugs automatically fix atrial fibrillation?
Not automatically. Medications like ACE inhibitors or diuretics reduce pressure, which can lessen AF episodes, but rhythm‑specific drugs (beta blockers, calcium‑channel blockers) or procedures (ablation) may still be needed.
Is it safe to exercise if I have both hypertension and AF?
Absolutely, as long as you follow a gradual plan. Start with 10‑minute walks, monitor heart rate, and avoid high‑intensity bursts until your doctor clears you. Regular aerobic activity actually improves both conditions.
How often should I check my blood pressure if I have AF?
Twice daily (morning and evening) for at least a week to get a reliable average. After stabilization, weekly checks are sufficient unless symptoms change.
Can diet alone lower my blood pressure enough to impact AF?
A DASH‑style diet (rich in fruits, veggies, low‑fat dairy, and low sodium) can drop systolic pressure by 8‑14mmHg, which translates into a noticeable reduction in AF triggers for many patients.

Write a comment