Every year, thousands of people in hospitals and pharmacies around the world get the wrong medicine-not because of a careless mistake, but because two drugs look or sound too much alike. This isn’t rare. It’s common. And it’s mostly happening with generic drugs.
What Are Look-Alike, Sound-Alike (LASA) Drugs?
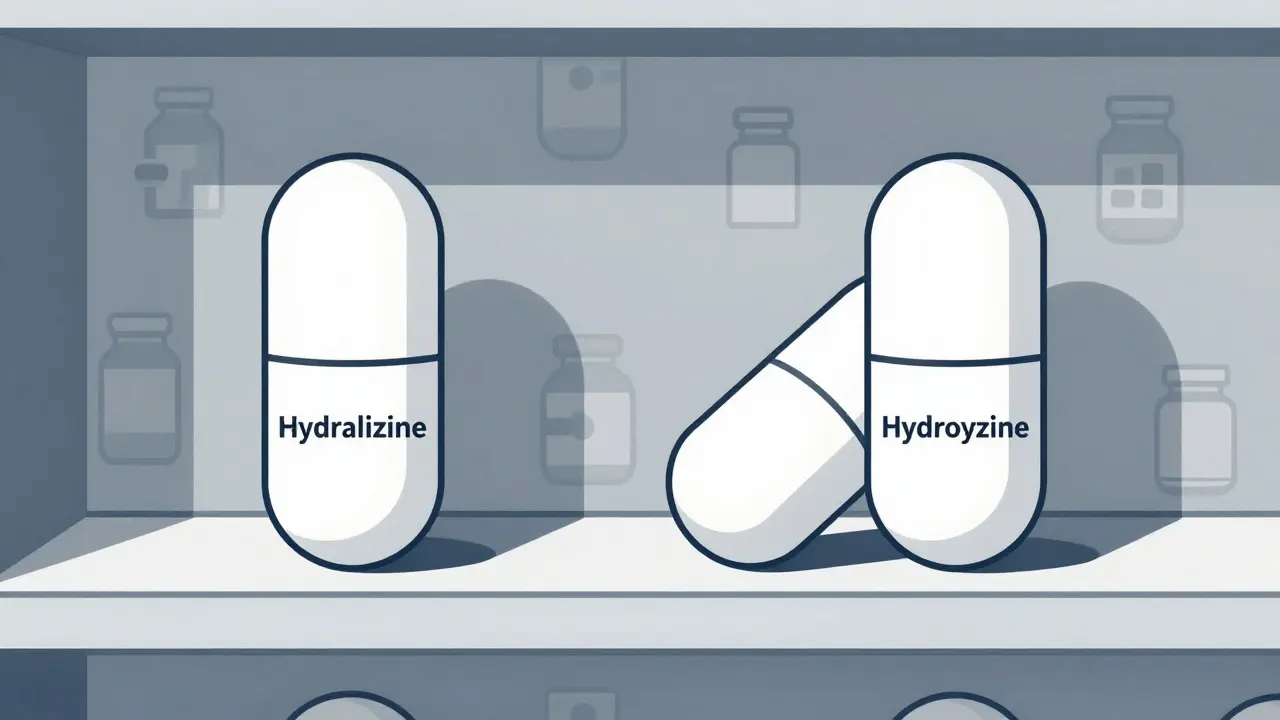
Look-alike, sound-alike (LASA) drugs are medications with names or packaging that are confusingly similar. One might be spelled almost the same as another-like hydralazine and hydroxyzine. Or they might sound identical when a nurse hears a doctor say them out loud-like dopamine and dobutamine. Both can be deadly.
Generic drugs make up over 90% of prescriptions filled in Australia and the U.S. But unlike brand-name drugs, generics aren’t required to have unique packaging or color schemes. So if two different companies make a 10 mg capsule of two different drugs, they might both look like plain white or blue pills. The labels? Nearly identical font size, layout, and spacing. One wrong pick-and a patient gets the wrong treatment.
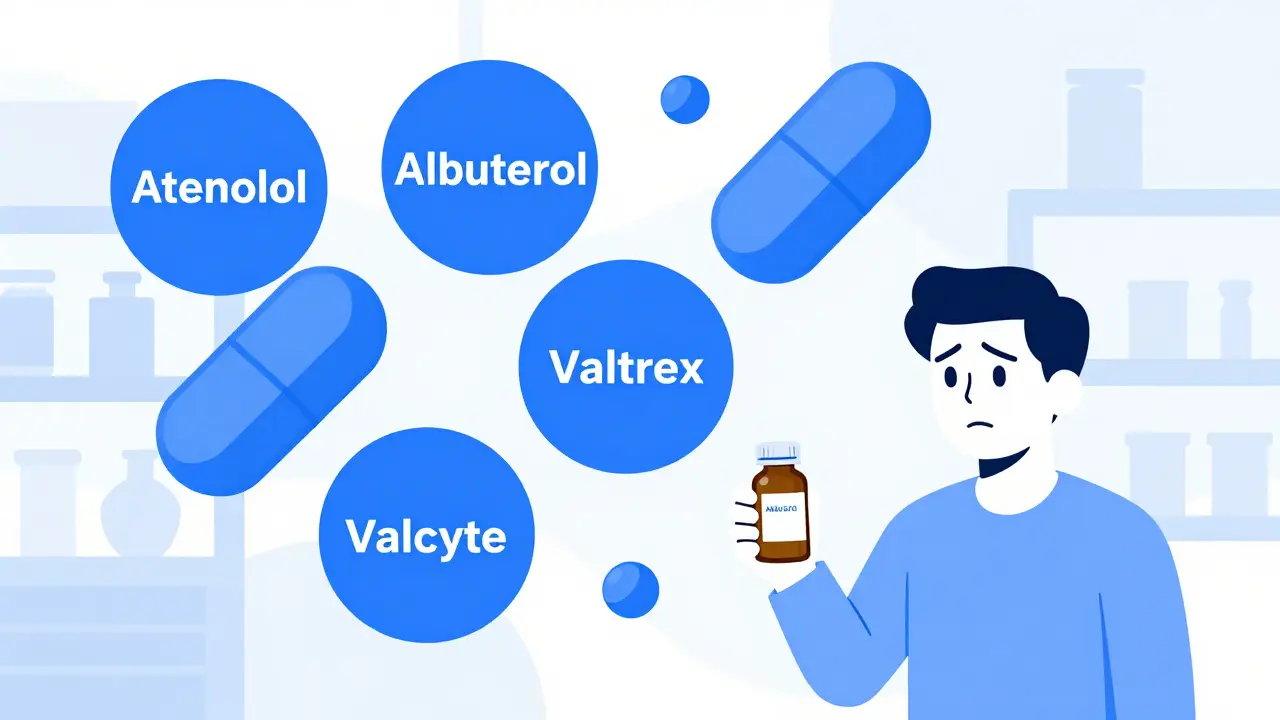
Take Valtrex (valacyclovir) and Valcyte (valganciclovir). Both start with “Val-,” both are used in transplant and HIV patients, and both come in tablet form. One treats herpes, the other prevents a deadly CMV infection. Mix them up? You could cause organ rejection or severe immune damage.
Why Generics Are the Biggest Problem
Brand-name drugs usually have distinct packaging. Think of the bright orange of Advil or the blue diamond of Viagra. But generics? They’re made by dozens of manufacturers. Each one picks their own color, shape, and label design. There’s no national standard.
Pharmacists in Sydney, Melbourne, and Brisbane report seeing the same issue: a patient walks in with a prescription for atenolol (a blood pressure drug), and the pharmacy pulls albuterol (an asthma inhaler) by accident. The names sound the same. The bottles look the same. The pills are both white and round.
According to the World Health Organization, LASA errors cause about 25% of all medication mistakes globally. That’s one in four. And nearly half of those involve generic drugs. Why? Because when a hospital switches from a brand-name drug to a cheaper generic, they don’t always check if the new version looks too much like another drug on the shelf.
How These Errors Happen
It’s not just one mistake. It’s a chain.
- Prescribing: A doctor writes “hydroxyzine” but the electronic system auto-fills “hydralazine” because the names are close.
- Dispensing: A pharmacist grabs the wrong bottle from a shelf where both drugs sit side-by-side.
- Administering: A nurse reads “prednisone” off a label but hears “prednisolone” because they sound alike-and gives the wrong dose.
And it’s not just handwritten prescriptions anymore. Even in digital systems, if two drug names appear next to each other in a dropdown menu, humans pick the wrong one. A 2023 study in the Journal of the American Medical Informatics Association found that AI-powered systems reduced these errors by 82%-but most hospitals still don’t use them.
Nurses in ICU units tell stories of nearly fatal mix-ups. One nurse gave quinidine (for heart rhythm) instead of quinine (for malaria). The patient went into cardiac arrest. Another gave epinephrine instead of epinephrine-wait, no, that’s the same drug. But in some hospitals, they stock epinephrine and epinephrine with different concentrations. One is for cardiac arrest. The other is for allergic reactions. Give the wrong one? Death.

What’s Being Done-And What’s Not
There are known fixes. But they’re not used everywhere.
Tall man lettering is one. It’s when you capitalize the different parts of similar names. So instead of “prednisone” and “prednisolone,” you write “predniSONE” and “predniSOLONE.” It’s simple. It works. A 2020 study showed it cut LASA errors by 67% in 12 hospitals.
Physical separation is another. Keep high-risk pairs far apart on the shelf. Don’t put hydroxyzine next to hydralazine. Don’t put atenolol next to albuterol. But many pharmacies still organize by alphabetical order-making it worse.
Barcode scanning helps too. When a nurse scans the drug and the patient’s wristband, the system checks if it matches. But if the barcode is wrong-or if the system doesn’t flag LASA pairs-it’s useless.
And then there’s the biggest gap: no global standard for generic packaging. The FDA in the U.S. and the TGA in Australia can reject drug names that are too similar-but they can’t control how a generic drug looks once it’s made. A generic version of a blood pressure pill might be blue. Another generic for a sedative might be blue too. No rules. No warnings. Just risk.
Who’s at Risk?
It’s not just the elderly. It’s kids. It’s pregnant women. It’s people with chronic illnesses taking multiple drugs.
Children are especially vulnerable. A study found that even though LASA errors are rare in pediatrics-fewer than 1 per 1,000 prescriptions-they’re more likely to cause serious harm. Why? Because kids’ doses are tiny. A 10 mg error isn’t a mistake. It’s a overdose.
And it’s not just the patient. Pharmacists and nurses are drowning in pressure. One pharmacist told me: “I’ve had to pull a drug off the shelf 12 times in one shift just to check the label. I’m not stupid. I’m tired.”
What You Can Do
You don’t need to be a doctor to help prevent these errors.
- Know your meds. If you’re prescribed a generic, ask: “What’s the brand name? What’s this for?” Don’t assume the pill looks the same as last time.
- Check the label. Compare the name on the bottle to the prescription. If it says “hydroxyzine” but you were told it’s for anxiety, and you have high blood pressure? Ask.
- Use one pharmacy. If you fill all your scripts at one place, they’ll spot if you’re getting two similar drugs.
- Speak up. If a nurse gives you a pill that looks different, ask why. Don’t take it just because they say it’s “the same.”
And if you’re a healthcare worker? Push for tall man lettering. Push for barcode scanning. Push for separation on the shelves. Don’t wait for someone else to fix it.
The Future: Tech Can Help-If We Let It
Artificial intelligence is now good enough to catch 98% of LASA errors before they happen. Systems can flag a prescription for “valacyclovir” and warn the doctor: “You’re prescribing this for a transplant patient. Did you mean valganciclovir?”
But only a few hospitals in Australia use them. Most still rely on human memory. And memory fails.
The WHO’s “Medication Without Harm” campaign wants to cut severe medication errors by 50% by 2025. But without fixing LASA errors, that goal won’t happen. The FDA has already rejected 34 drug names in 2021 just because they were too similar. The European Medicines Agency now requires all new drugs to pass a name-similarity test. Australia’s TGA is starting to pay attention-but slowly.
Change is possible. It’s just not happening fast enough.
Final Thought: It’s Not Your Fault
When a patient gets the wrong drug, we blame the nurse. The pharmacist. The doctor. But the real problem? A system that lets two drugs look and sound the same.
It’s like having two keys that open different doors-but they’re shaped almost exactly the same. You wouldn’t blame someone for grabbing the wrong one. You’d fix the keys.
Medication safety isn’t about being perfect. It’s about designing systems that don’t let humans fail.
What are look-alike, sound-alike (LASA) drugs?
Look-alike, sound-alike (LASA) drugs are medications with names or packaging that are visually or phonetically similar, causing confusion during prescribing, dispensing, or administration. Examples include hydralazine and hydroxyzine (look-alike) or dopamine and dobutamine (sound-alike). These errors are especially common with generic drugs due to inconsistent packaging and naming.
Why are generic drugs more likely to cause LASA errors?
Generic drugs are made by multiple manufacturers, each using different colors, shapes, and label designs. Unlike brand-name drugs, there’s no standard for how generics should look. This means two different drugs can end up looking nearly identical-making it easy to grab the wrong one. Plus, generic names often share prefixes or suffixes (like “val-” in Valtrex and Valcyte), increasing confusion.
How common are LASA medication errors?
About 25% of all medication errors worldwide are caused by look-alike or sound-alike drug names, according to the World Health Organization. In Australia and the U.S., pharmacists report encountering LASA errors at least once a month, with over a third reporting near-misses weekly. These errors can lead to death, organ failure, or severe harm-especially in children and elderly patients.
What’s tall man lettering, and does it work?
Tall man lettering is when the differing parts of similar drug names are capitalized-for example, predniSONE vs. predniSOLONE. This visual cue helps distinguish between look-alike names. Studies show it reduces LASA errors by up to 67% in hospitals that use it. It’s simple, low-cost, and highly effective-but still not widely adopted.
Can technology prevent LASA errors?
Yes. AI-powered clinical decision support systems embedded in electronic health records can flag potential LASA errors before they happen. One 2023 study found these systems reduced errors by 82% and caught 98.7% of risky matches. Barcode scanning and smart dispensing systems also help. But most clinics and pharmacies still rely on manual checks, leaving patients vulnerable.
What can patients do to avoid LASA errors?
Always ask: What is this medicine for? What’s the brand name? Does it look different from your last refill? Check the label against your prescription. Use one pharmacy so your records are centralized. If something seems off-speak up. You’re the last line of defense.
Medication safety isn’t about blaming individuals. It’s about fixing systems. And right now, the system is still letting too many people get the wrong pill-because two names looked too similar, or sounded too much alike. It doesn’t have to be this way.






Write a comment