Menopause Bone Loss Risk Calculator
This calculator estimates your risk of accelerated bone loss during menopause based on key factors. Understanding your risk helps you take proactive steps to protect your bone health.
Understanding Your Results
The calculator assesses multiple factors that influence bone health during menopause. A higher score indicates increased risk of accelerated bone loss and potential osteoporosis.
Risk Categories:
- High Risk - Significant bone loss expected; immediate action recommended
- Moderate Risk - Noticeable bone loss likely; preventive measures important
- Low Risk - Minimal bone loss expected; maintain healthy habits
When a woman hits her 50s, the conversation often shifts to hot flashes, mood swings, and sleep changes. What gets less attention is the silent erosion happening inside the skeleton. During menopause, declining estrogen levels tip the balance between bone breakdown and formation, leaving women vulnerable to fractures later in life. This guide breaks down what’s actually happening to your bones, why it matters, and what you can do right now to keep them strong.
Quick Take
- Estrogen loss after menopause speeds up bone loss by up to 2% per year.
- Bone mineral density (BMD) can drop enough to cause osteoporosis in 20‑30% of women by age 65.
- Calcium (1,200mg) and vitaminD (800‑1,000IU) are the nutritional basics.
- Weight‑bearing exercise (150min weekly) and HRT can slow loss dramatically.
- Regular DEXA scans starting at age 60 help catch problems early.
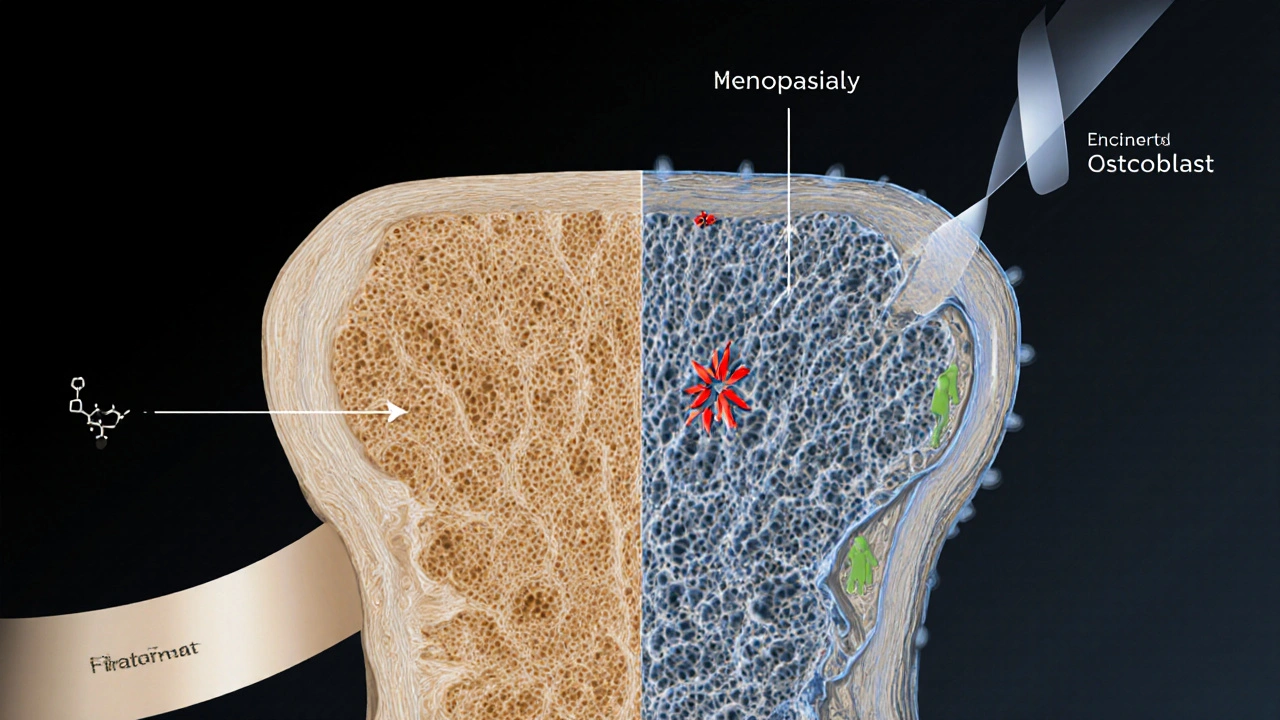
Understanding Bone Damage During Menopause
Menopause is the natural cessation of menstrual cycles, typically occurring between ages 45 and 55, and is marked by a sharp drop in estrogen production. Estrogen plays a key role in telling bone‑building cells (osteoblasts) to keep working while calming the bone‑breaking cells (osteoclasts). When estrogen falls, osteoclasts go into overdrive and bone loss accelerates.
Osteoporosis is a disease characterized by porous, fragile bones that increase the risk of fractures, especially in the hip, spine, and wrist. It’s the most common bone condition linked to menopause, and the World Health Organization estimates that one in three women over 50 will experience an osteoporotic fracture.
Why Bone Mineral Density Declines
Bone mineral density (BMD) is a measurement of the amount of mineral (mostly calcium) packed into a given area of bone, usually expressed in g/cm². During the first five years after menopause, women can lose up to 8‑10% of BMD at the spine and 6‑8% at the hip. The loss is fastest in the first two years because the body’s hormonal balance is still readjusting.
Key Risk Factors
- Family history of osteoporosis or hip fractures.
- Low body weight (BMI<18.5) or a very thin frame.
- Smoking and excessive alcohol (more than 2 drinks/day).
- Sedentary lifestyle with little or no weight‑bearing activity.
- Medications such as corticosteroids, certain anti‑seizure drugs, or aromatase inhibitors.
Prevention Strategies
There’s no single magic bullet, but a combo of nutrition, movement, and, when appropriate, medication can keep bone loss at bay.
Nutrition Matters
Calcium is the primary mineral that provides structural strength to bone, with an adult daily recommendation of 1,200mg for post‑menopausal women. Good sources include dairy (milk, yogurt, cheese), fortified plant milks, leafy greens (kale, bokchoy), and almonds. If you struggle to meet the target through food, a calcium supplement can fill the gap, but stay under 2,000mg to avoid kidney stones.
Vitamin D is a fat‑soluble vitamin that enhances calcium absorption in the gut and supports bone remodeling, with a recommended intake of 800‑1,000IU daily for adults over 50. Sunlight, fatty fish (salmon, mackerel), egg yolks, and fortified cereals are natural sources. Many doctors advise a supplement during winter months when sun exposure drops.
Move to Strengthen
Weight‑bearing exercise-think brisk walking, jogging, dancing, or stair climbing-applies mechanical stress that signals osteoblasts to lay down new bone. Aim for at least 150minutes of moderate activity each week, plus two sessions of resistance training (lifting light weights or using resistance bands).
Balance and flexibility drills (yoga, tai chi) don’t directly boost BMD, but they reduce fall risk, which matters because most fractures happen when a fall occurs.
Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy is a medical treatment that supplies estrogen (sometimes combined with progesterone) to counteract menopausal hormone decline. When started early (within 10 years of menopause) and used for a limited period (3‑5years), HRT can preserve BMD at a rate comparable to pre‑menopausal levels. Women must discuss personal risk factors (breast cancer, blood clots) with their doctor before starting.
Medication Options
For women who already show low BMD or have a fracture history, doctors may prescribe anti‑resorptive drugs. Bisphosphonates are a class of medications (e.g., alendronate, risedronate) that bind to bone and inhibit osteoclast activity, reducing bone loss by 40‑50% over 3‑5years. Side effects can include mild stomach irritation and, rarely, atypical femur fractures. Newer agents like denosumab (a monoclonal antibody) offer alternatives for those who can’t tolerate bisphosphonates.
Quick Comparison of Lifestyle vs. Medication
| Approach | Primary Benefit | Typical Cost | Key Considerations |
|---|---|---|---|
| Calcium & VitaminD intake | Supports mineralization | Low‑to‑moderate (food+supplements) | Need consistent daily dosing; watch for excess calcium. |
| Weight‑bearing exercise | Stimulates new bone formation | Free‑to‑low (gym membership optional) | Requires regular schedule; joint issues may limit intensity. |
| Hormone Replacement Therapy | Restores estrogen, slows loss | Moderate (prescription cost) | Not suitable for all; monitor for cardiovascular risks. |
| Bisphosphonates | Strongly reduces fracture risk | Moderate‑high (prescription) | Potential GI side effects; rare atypical fractures. |
Monitoring Your Bone Health
The gold standard test is a DEXA (dual‑energy X‑ray absorptiometry) scan, which measures BMD at the spine and hip. Guidelines suggest a baseline scan at menopause onset (or by age 60) and a follow‑up every 2‑3years if results are normal. Scores are reported as T‑scores:‑1.0 or above is normal, between‑1.0 and‑2.5 indicates osteopenia, and‑2.5 or lower confirms osteoporosis.
Common Myths Debunked
- Myth: “Only skinny women get osteoporosis.” Fact: Even women with higher BMI can lose bone if they’re inactive or calcium‑deficient.
- Myth: “Supplements alone fix bone loss.” Fact: Supplements work best when paired with diet, exercise, and medical guidance.
- Myth: “If I feel fine, my bones are fine.” Fact: Bone loss is silent; you can fracture a hip from a minor stumble.
When to Seek Professional Help
If you have any of the following, schedule a bone health assessment promptly:
- History of a fracture after age40.
- Persistent back pain that worsens at night (possible vertebral compression fracture).
- Family history of early osteoporosis.
- Use of long‑term steroids or other bone‑weakening medications.
Your doctor can order a DEXA scan, review blood work (calcium, vitaminD, thyroid function), and discuss whether HRT or prescription meds are right for you.
Frequently Asked Questions
Can diet alone prevent osteoporosis after menopause?
A balanced diet rich in calcium and vitaminD is essential, but on its own it rarely stops bone loss. Pairing nutrition with regular weight‑bearing exercise and, if needed, medical therapy gives the best protection.
How soon after menopause do I need a DEXA scan?
Many experts recommend a baseline DEXA at the start of menopause (around age50) or by age60 if you haven’t had one earlier. If you have risk factors, your doctor may order it earlier.
Is hormone replacement therapy safe for bone health?
When started within ten years of menopause and used for a limited period, HRT can significantly preserve bone density. However, it isn’t suitable for everyone; discuss personal risks such as breast cancer or clotting disorders with your physician.
What exercises are most effective for strengthening bones?
Activities that load the skeleton against gravity work best: walking, jogging, dancing, stair climbing, and resistance training with weights or bands. Aim for at least 150minutes of moderate activity weekly, plus two strength sessions.
Can I take calcium supplements if I already eat dairy?
If your total dietary calcium falls short of the 1,200mg daily goal, a supplement can help. Avoid exceeding 2,000mg per day to reduce the risk of kidney stones.
Understanding the link between menopause and bone damage equips you to act before a fracture happens. By tracking your BMD, eating the right nutrients, staying active, and discussing medical options with a healthcare professional, you can keep your skeleton strong well into later years.







Write a comment