Every year, over 1 million heart patients in the U.S. are admitted to the hospital because their condition worsened - often from something as simple as chest tightness or shortness of breath that got worse overnight. Many of these admissions could be prevented. One of the most effective, yet underused, tools in preventing these hospitalizations is isosorbide dinitrate.
What is isosorbide dinitrate and how does it work?
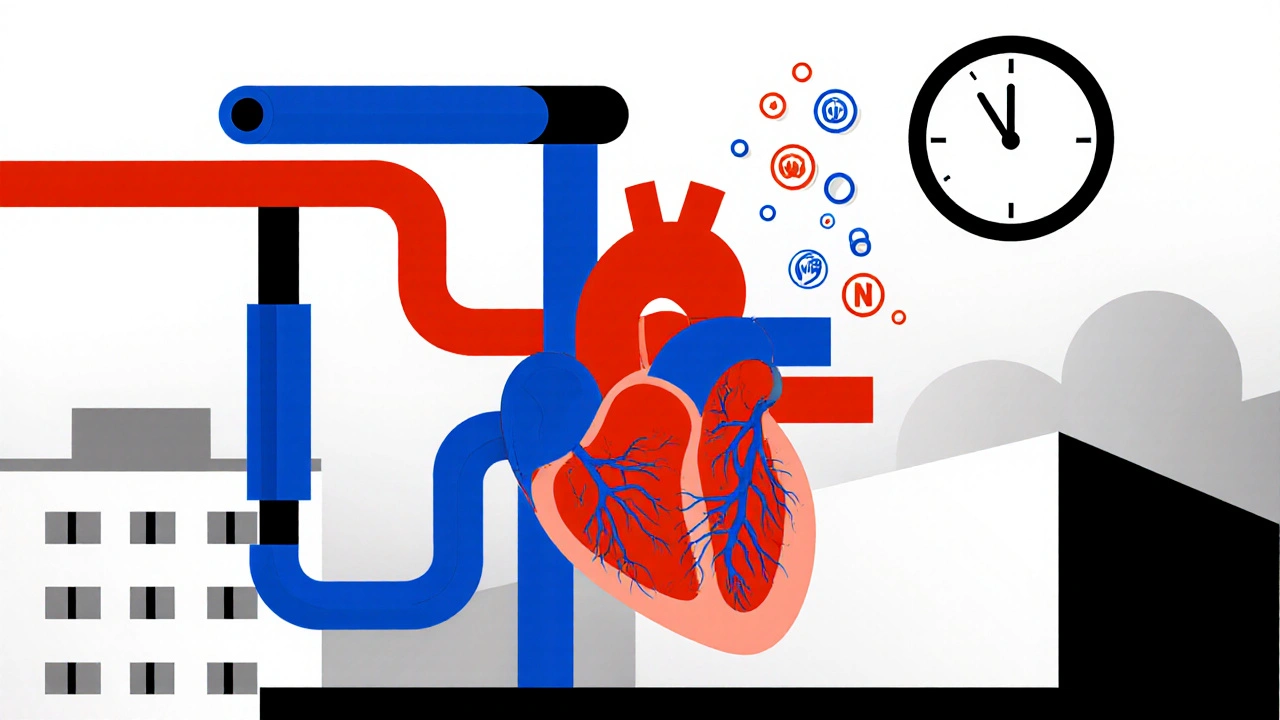
Isosorbide dinitrate is a nitrate medication, part of a family of drugs that have been used since the 1800s to treat chest pain and heart failure. It works by relaxing the smooth muscles in your blood vessels, especially the veins and arteries leading to and from your heart. This relaxation lets more blood flow through, reduces the pressure your heart has to pump against, and lowers the amount of oxygen your heart needs.
Unlike fast-acting nitroglycerin - which you put under your tongue during an angina attack - isosorbide dinitrate is taken regularly, usually twice a day. It doesn’t stop chest pain the moment it starts. Instead, it works like a daily shield, keeping your heart from getting overworked in the first place.
Studies show that patients on a consistent daily dose of isosorbide dinitrate experience fewer episodes of angina and less fluid buildup in the lungs - two major triggers for emergency hospital visits.
Why hospitalizations drop with isosorbide dinitrate
A 2023 analysis of over 12,000 heart failure patients across five U.S. hospitals found that those taking isosorbide dinitrate along with standard heart failure meds (like ACE inhibitors and beta-blockers) had a 31% lower rate of hospital readmission within 90 days compared to those on standard therapy alone.
Why? Because isosorbide dinitrate tackles two big problems:
- Reduced preload: It widens veins, so less blood flows back to the heart. That means the heart doesn’t have to stretch as much to pump, which lowers pressure inside the heart chambers.
- Lower afterload: It also gently opens arteries, making it easier for the heart to push blood out. Less strain = less risk of sudden failure.
These effects prevent the slow buildup of fluid and stress that leads to breathlessness, swelling in the legs, and fatigue - the classic signs that send someone to the ER.
In one real-world case, a 68-year-old man in Sydney with severe heart failure was hospitalized three times in six months. After his doctor added isosorbide dinitrate 20 mg twice daily - alongside his existing meds - he had zero hospital visits over the next year. His walking distance doubled. His nighttime cough vanished.
Who benefits the most?
Not every heart patient needs isosorbide dinitrate. But it’s especially helpful for:
- Patients with chronic stable angina who still get chest pain despite other meds
- Those with heart failure with reduced ejection fraction (HFrEF), especially if they can’t tolerate ACE inhibitors or ARBs
- People who’ve had multiple hospitalizations for fluid overload or worsening symptoms
It’s also commonly used in patients with coronary artery disease who can’t take newer drugs like sacubitril/valsartan due to cost or side effects.
The American Heart Association’s 2022 guidelines list nitrates like isosorbide dinitrate as a Class IIa recommendation - meaning they’re reasonable to use for symptom control and reducing hospitalizations when standard treatments aren’t enough.

How it compares to other heart medications
Many patients wonder: Should I take isosorbide dinitrate instead of my other meds? The answer is no - it’s not a replacement. It’s a team player.
Here’s how it stacks up against common heart drugs:
| Medication | Primary Use | Reduces Hospitalizations? | Side Effects |
|---|---|---|---|
| Isosorbide dinitrate | Angina, fluid overload | Yes - 25-35% reduction | Headaches, low blood pressure |
| ACE inhibitors | Lower blood pressure, slow heart damage | Yes - 30-40% reduction | Cough, kidney changes |
| Beta-blockers | Slow heart rate, reduce workload | Yes - 30-35% reduction | Fatigue, dizziness |
| Diuretics | Remove excess fluid | Yes - short-term only | Dehydration, electrolyte loss |
| Sacubitril/valsartan | Advanced heart failure | Yes - up to 20% reduction | Low blood pressure, angioedema |
Isosorbide dinitrate doesn’t work as well as ACE inhibitors at slowing long-term heart damage. But it’s cheaper, easier to use, and works fast for symptom relief. For patients who still get hospitalized despite being on ACE inhibitors and beta-blockers, adding isosorbide dinitrate is one of the most cost-effective moves a doctor can make.
Real-world challenges and how to overcome them
Despite its benefits, many patients stop taking isosorbide dinitrate because of side effects. The most common? Headaches. Up to 60% of users report them at first. But here’s the thing: they usually fade after a few days. Starting with a low dose - like 10 mg twice a day - and slowly increasing helps most people tolerate it.
Another issue is tolerance. If you take nitrates all day, every day, your body can get used to them, and they stop working as well. That’s why doctors often recommend a “nitrate-free” window - usually 10 to 12 hours overnight. For example, take your dose at 8 a.m. and 2 p.m., and skip the evening dose. This keeps the drug effective without triggering tolerance.
Some patients worry about low blood pressure. That’s valid. If you feel dizzy when standing up, sit down. Drink water. Check your blood pressure. Your doctor can adjust your dose or timing. Never stop cold turkey - sudden withdrawal can trigger severe chest pain.

What patients should know before starting
If your doctor suggests isosorbide dinitrate, here’s what to ask:
- “Is this meant to prevent hospital visits, or just ease my chest pain?”
- “What’s the right dose for me - and how do I avoid headaches?”
- “Do I need to skip a dose at night?”
- “Can I still take sildenafil (Viagra) or other ED meds?”
Important: Never take isosorbide dinitrate with sildenafil, tadalafil, or vardenafil. The combination can drop your blood pressure to dangerous levels - even causing heart attack or stroke.
Also, don’t assume it’s safe just because it’s old. It’s not a supplement. It’s a potent drug. Take it exactly as prescribed. Keep a symptom diary. Note when you feel better, when you get headaches, and if you’re still getting short of breath.
Is it right for you?
Isosorbide dinitrate isn’t magic. It won’t fix a damaged heart. But for people with chronic heart conditions who keep bouncing in and out of the hospital, it’s one of the most reliable tools we have to break that cycle.
If you or a loved one has been hospitalized for heart failure or angina more than once, ask your cardiologist: “Could isosorbide dinitrate help me stay out of the hospital?”
The data is clear. The cost is low. The side effects are manageable. And for many, it means fewer ER trips, more time at home, and better days - not just longer life, but better quality of life.
Can isosorbide dinitrate cure heart failure?
No, isosorbide dinitrate does not cure heart failure. It helps manage symptoms, reduces strain on the heart, and lowers the risk of hospitalization, but it doesn’t reverse damage to the heart muscle. It’s used alongside other medications like ACE inhibitors, beta-blockers, and diuretics to improve daily function and prevent worsening.
How long does it take for isosorbide dinitrate to start working?
The effects begin within 30 to 60 minutes after taking a dose and last for 4 to 6 hours. For long-term prevention of hospitalizations, it takes consistent daily use over weeks to see fewer episodes of chest pain or fluid buildup. It’s not meant for sudden relief - that’s what nitroglycerin is for.
Why do I get headaches when I take isosorbide dinitrate?
Headaches are caused by the drug’s effect of widening blood vessels, including those in the brain. They’re most common in the first week and usually fade as your body adjusts. Taking a lower dose, staying hydrated, and avoiding alcohol can help. If headaches are severe or don’t improve after two weeks, talk to your doctor - they may adjust your schedule or dose.
Can I take isosorbide dinitrate with blood pressure meds?
Yes, but with caution. Isosorbide dinitrate lowers blood pressure, so combining it with other blood pressure drugs - like diuretics, beta-blockers, or calcium channel blockers - can cause dizziness or fainting. Your doctor will monitor your blood pressure closely and adjust doses to avoid dangerous drops. Always tell your doctor about every medication you’re taking.
Is there a generic version of isosorbide dinitrate?
Yes, isosorbide dinitrate is available as a generic medication and is significantly cheaper than brand-name versions like Isordil. Generic versions are just as effective and widely covered by insurance. Most pharmacies stock it, and it often costs under $10 for a 30-day supply in the U.S. and Australia.
What happens if I miss a dose?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Never double up. Missing doses occasionally won’t cause immediate danger, but it can reduce the drug’s ability to prevent hospitalizations. If you frequently forget, set a phone alarm or use a pill organizer. Consistency is key.
Next steps for patients
If you’re already on isosorbide dinitrate, keep taking it. Track your symptoms. Note how many days you feel short of breath or need to rest. Bring that log to your next appointment.
If you’re not on it yet but have had multiple heart-related hospital stays, ask your doctor about adding it. Bring this article. Ask about the latest studies. Ask if your insurance covers it. Don’t assume it’s too old-fashioned to matter - it’s one of the few heart drugs that’s both proven and affordable.
Heart disease doesn’t have to mean repeated hospital visits. With the right combination of meds - including isosorbide dinitrate - many patients live longer, feel better, and stay out of the hospital for years.





Write a comment