Every year, thousands of children and adults receive the wrong dose of liquid medicine-not because someone was careless, but because the system is broken. A 2023 study in the Journal of Pediatrics found that 80% of pediatric home medication errors involve liquid drugs. That’s not a small number. It’s a crisis. And it’s mostly preventable.
Why Liquid Medications Are So Dangerous
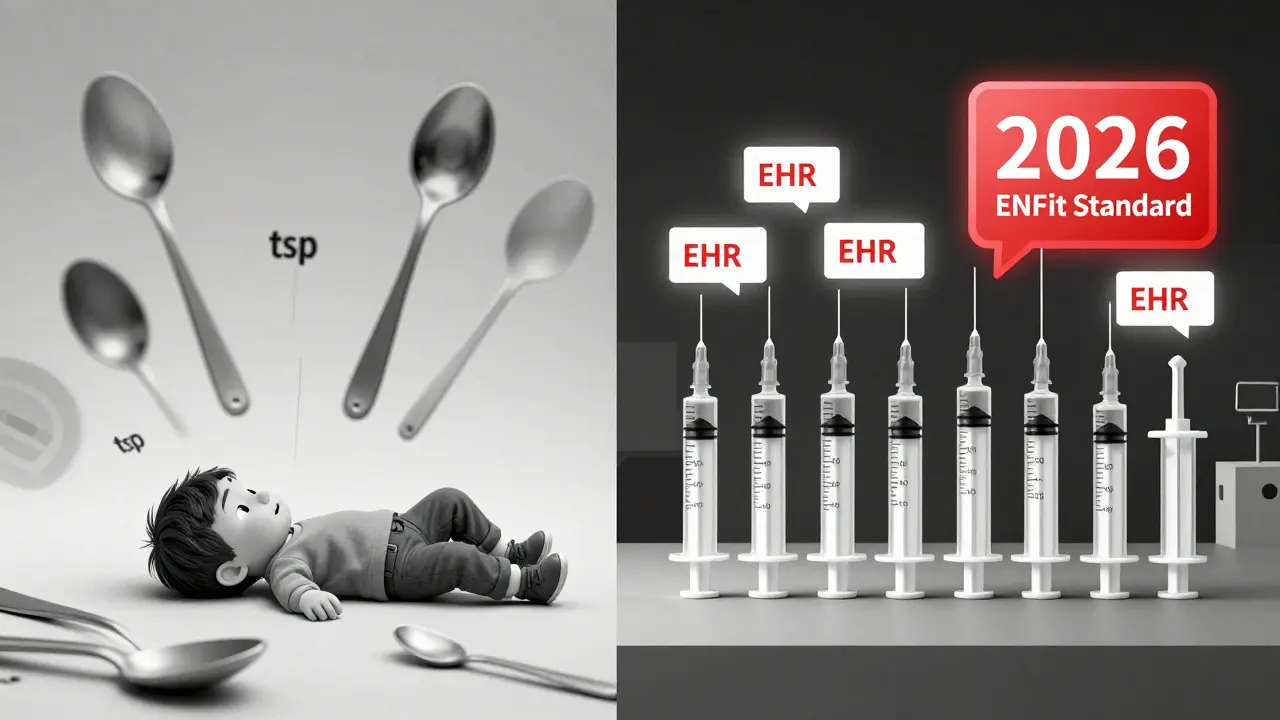
Liquid medicines are tricky. They look simple: pour, measure, give. But that’s where things go wrong. A teaspoon isn’t a teaspoon. A tablespoon isn’t a tablespoon. In fact, household spoons vary by up to 50% in volume. A 2022 NIH study showed that 62% of caregivers using kitchen spoons gave doses that were too high or too low. That’s more than half. In hospitals, the problem is just as bad. A 2021 study in Academic Emergency Medicine found that dosing cups had a 41% error rate for doses under 5 mL. Oral syringes? Just 8.2%. That’s a five-fold difference. And yet, many pharmacies still hand out dosing cups with pediatric prescriptions. Why? Tradition. Convenience. Lack of awareness. The biggest danger? Units. Prescriptions still sometimes say “teaspoon” or “tablespoon.” The American Academy of Pediatrics banned those terms in 2015. The World Health Organization says eliminating non-metric units prevents 33% of all liquid medication errors. But it’s still happening. A 2024 report from the Institute for Safe Medication Practices found that 28% of preventable pediatric errors come from confusing units like tsp and tbsp.The Right Tool: Oral Syringes Are Non-Negotiable
If you’re giving liquid medicine to a child-or even an adult who can’t swallow pills-use an oral syringe. Not a cup. Not a spoon. A syringe. Oral syringes with 0.1 mL graduations are the gold standard for doses under 1 mL. For 1-5 mL, use syringes with 0.5 mL markings. These aren’t luxury items. They’re medical necessities. A 2016 Yale study found they’re 37% more accurate than dosing cups. In real terms: if the doctor prescribes 2.5 mL, a syringe gets you within 0.1 mL. A cup? You’re guessing. Pharmacies should hand out an oral syringe with every liquid prescription. Period. The cost? About $0.85 per unit. That’s less than the price of a coffee. But only 54% of caregivers actually get one, according to a 2023 HealthyChildren.org survey. That’s unacceptable. If you’re given a dosing cup, throw it away. Get a syringe. Ask the pharmacist for one. If they say no, ask why. Then ask for a manager. This isn’t about preference-it’s about safety.Units Must Be in Milliliters Only
No more “teaspoons.” No more “tablespoons.” No more “cc” or “mL” written in tiny font next to “tsp.” The label must say only milliliters (mL). The American Society of Health-System Pharmacists (ASHP) made this a requirement in 2023. The Joint Commission backs it. The FDA’s 2024 draft guidance now requires all over-the-counter liquid medicines to include enclosed dosing devices with metric-only labeling. This is happening. But not fast enough. If you see a prescription that says “give 1 tsp,” ask the prescriber to rewrite it as “give 5 mL.” If you’re a pharmacist and you’re dispensing a bottle with “tsp” on the label, refuse to fill it. Push back. Document it. Your refusal could save a life.
Technology Can Help-But Only If It’s Used Right
Hospitals and clinics have tools that can stop errors before they happen. Computerized physician order entry (CPOE) systems with clinical decision support can flag a dose that’s outside the safe range for a child’s weight. A 2023 Cochrane Review found these systems reduce pediatric liquid errors by 58%. Barcode medication administration (BCMA) systems scan the patient’s wristband, the medication, and the dose before giving it. They cut wrong-dose errors by 48%. But only if used 100% of the time. If a nurse skips the scan because they’re rushed? The system fails. Electronic prescribing (e-prescribing) cuts calculation errors by 63% compared to paper. But it’s expensive. The average cost per physician is $12,500. That’s why rural clinics still use paper. That’s why errors still happen. The ENFit connector system is another game-changer. Since 2016, ISO standards require liquid medication syringes to have a unique, non-interchangeable connector that won’t fit into IV lines. Before ENFit, people accidentally gave oral meds through IVs. That killed people. Now, hospitals using ENFit report 98% fewer wrong-route errors. But adoption is patchy. Only 42% of U.S. hospitals have fully switched to ENFit. Why? Cost. Training. Resistance. The average hospital spends $85,000 to replace all connectors. But the cost of one death? Unmeasurable.What Caregivers Can Do Right Now
You don’t need a hospital budget to prevent a wrong dose. Here’s what you can do today:- Always use an oral syringe. If you don’t have one, go to the pharmacy and ask for one. They’re free or cheap.
- Ignore teaspoons and tablespoons. If the label says “tsp,” convert it: 1 tsp = 5 mL, 1 tbsp = 15 mL. Write it down.
- Measure at eye level. Don’t tilt the syringe. Hold it up to your eyes so the liquid line matches the mark.
- Don’t use kitchen spoons. Even if you think you’re being careful. They’re not calibrated. Ever.
- Ask for a pre-measured dose. Some pharmacies offer single-dose syringes already filled. Ask. It’s safer.
- Keep a log. Write down what you gave, when, and how much. If you’re unsure later, you’ll know what you did.
What Clinicians and Pharmacies Must Do
If you’re a doctor, nurse, or pharmacist, you’re on the front lines. Here’s what you need to do:- Prescribe in mL only. No exceptions. If your EHR auto-fills “tsp,” change the template.
- Hand out an oral syringe with every liquid prescription. Even if the patient says they have one. Give them a new one. It’s sterile. It’s accurate.
- Label bottles in bold, clear mL. Use ANSI Z535.4-2011 safety label standards. “FOR ORAL USE ONLY” must be visible from across the room.
- Train your staff. A 2023 ASHP survey found 72% of facilities don’t give enough training time. That’s a recipe for error.
- Adopt ENFit. Don’t wait. The cost is high, but the risk of a wrong-route error is higher.
- Use EHR alerts. Make sure your system flags doses that exceed 20% of the standard weight-based range.
Why This Matters More Than You Think
Medication errors cost the U.S. healthcare system $42 billion a year. Liquid medication errors make up $8.3 billion of that. That’s not just money. That’s hospitalizations. That’s ER visits. That’s children who get sick because they got too much acetaminophen. That’s adults who have seizures because they got too much morphine. The good news? We know how to fix this. A 2022 meta-analysis in the American Journal of Health-System Pharmacy showed that when hospitals use a full safety bundle-oral syringes, mL-only labeling, staff training, and EHR alerts-they reduce errors by up to 65%. Kaiser Permanente did it. They mandated oral syringes, trained every caregiver, and integrated dose calculators into their EHR. They cut errors by 92%. You don’t need to be Kaiser to make a difference. You just need to care enough to do the right thing.What’s Coming Next
The future is getting smarter. Boston Children’s Hospital is testing smartphone apps that use augmented reality to show you exactly where the dose line should be. Johns Hopkins is piloting RFID-tagged syringes that auto-record doses in the EHR. These aren’t sci-fi. They’re real-and they’re coming fast. By 2026, all certified EHRs in the U.S. will be required to include pediatric dose-checking. The FDA will enforce metric-only labeling on all OTC liquids. The ENFit standard will be universal. But none of that matters if we don’t act now. Because the next wrong dose? It could be your child’s. Or your parent’s. Or yours.Why are dosing cups still used if they’re so inaccurate?
Dosing cups are still used because they’re cheaper, easier to store, and familiar. Many pharmacies stock them by default. But they’re not safe. Studies show they have error rates over 40% for small doses. Oral syringes are more accurate, more reliable, and cost less than a coffee. There’s no good reason to keep using cups for pediatric or high-risk liquid medications.
Can I use a regular syringe from the pharmacy for liquid meds?
No. Regular syringes are designed for injections and have Luer lock tips that can accidentally connect to IV lines. That’s dangerous. Always use an oral syringe-these have a wide, non-locking tip designed only for mouth use. Look for packaging that says “oral syringe” or “for oral use.”
What if the prescription says “give 1/2 tsp”?
Convert it immediately: 1/2 tsp = 2.5 mL. Write it down. Then use an oral syringe to measure 2.5 mL. Never guess. Never use a spoon. Even if the label says “tsp,” treat it as a mistake and correct it. Your safety depends on it.
Are there free oral syringes I can get?
Yes. Many pharmacies give them for free if you ask. Public health clinics, children’s hospitals, and some insurance programs also provide them. If your pharmacy refuses, ask to speak to the pharmacist in charge. You have a right to a safe dosing tool.
How do I know if my EHR has dose-checking alerts?
Ask your clinic’s IT or pharmacy team. A good system will pop up a warning if you enter a dose that’s more than 20% above or below the standard weight-based range for a child’s age or weight. If you don’t see these alerts, request them. It’s part of the Joint Commission’s National Patient Safety Goals.
What should I do if I think I gave the wrong dose?
Call your doctor or poison control immediately. Don’t wait for symptoms. In the U.S., call 1-800-222-1222. Keep the medication bottle and syringe handy. Even if you’re unsure, it’s better to be safe. Many errors are caught before harm happens-because someone spoke up.







Write a comment