Rosuvastatin Side Effect Risk Calculator
Personalized Risk Assessment
This tool helps you understand potential side effects based on your specific situation. Enter your details below to get a risk assessment.
Your Risk Assessment
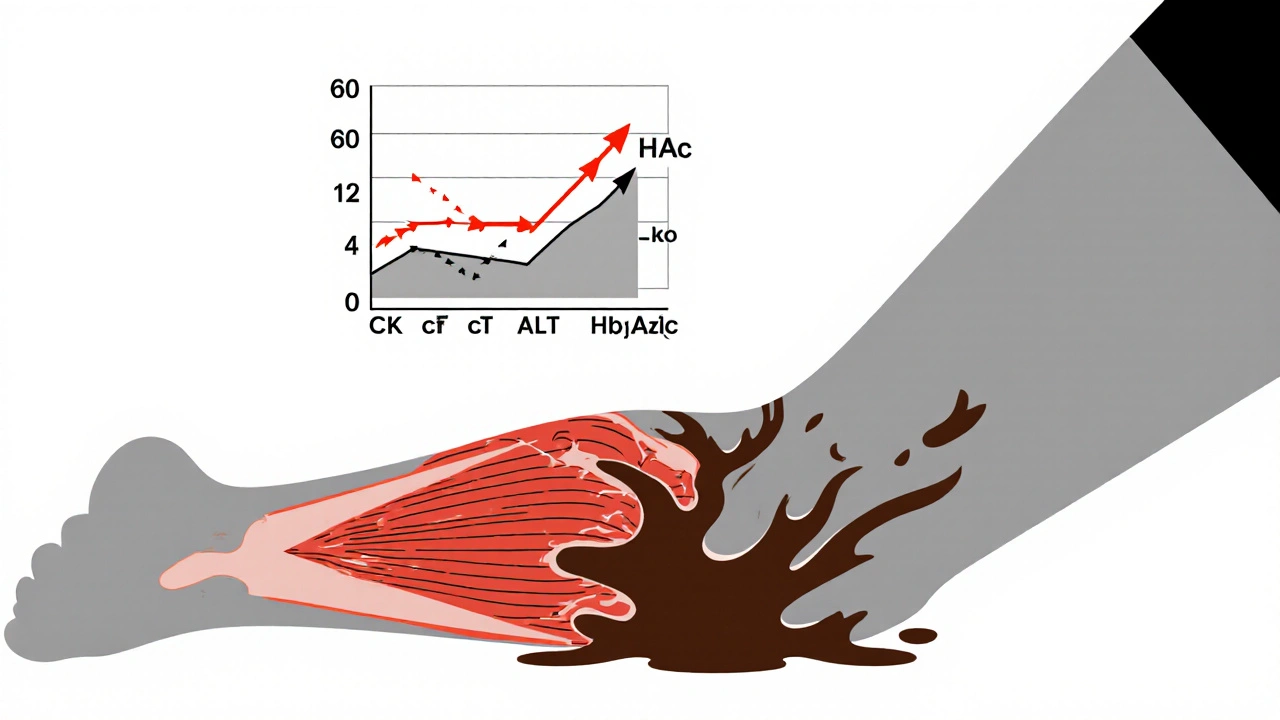
Muscle Side Effects
Rhabdomyolysis Risk
Liver Enzymes
Blood Sugar Impact
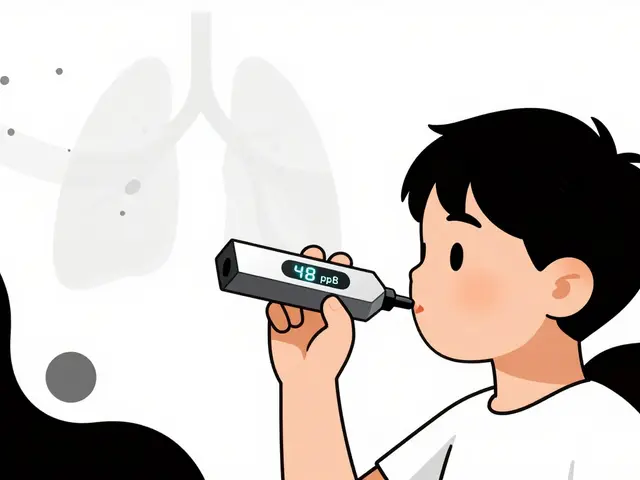
Kidney Function
Rosuvastatin is one of the most powerful statins available today. If you’ve been prescribed this medication, you’re likely being treated for high cholesterol or to lower your risk of a heart attack or stroke. But with great potency comes the need for careful monitoring. Unlike older statins, rosuvastatin doesn’t just lower cholesterol-it lowers it aggressively. That’s good news for your arteries, but it also means your body might react in ways you didn’t expect. The key isn’t avoiding the drug-it’s knowing what to watch for, when to check, and what to do if something feels off.
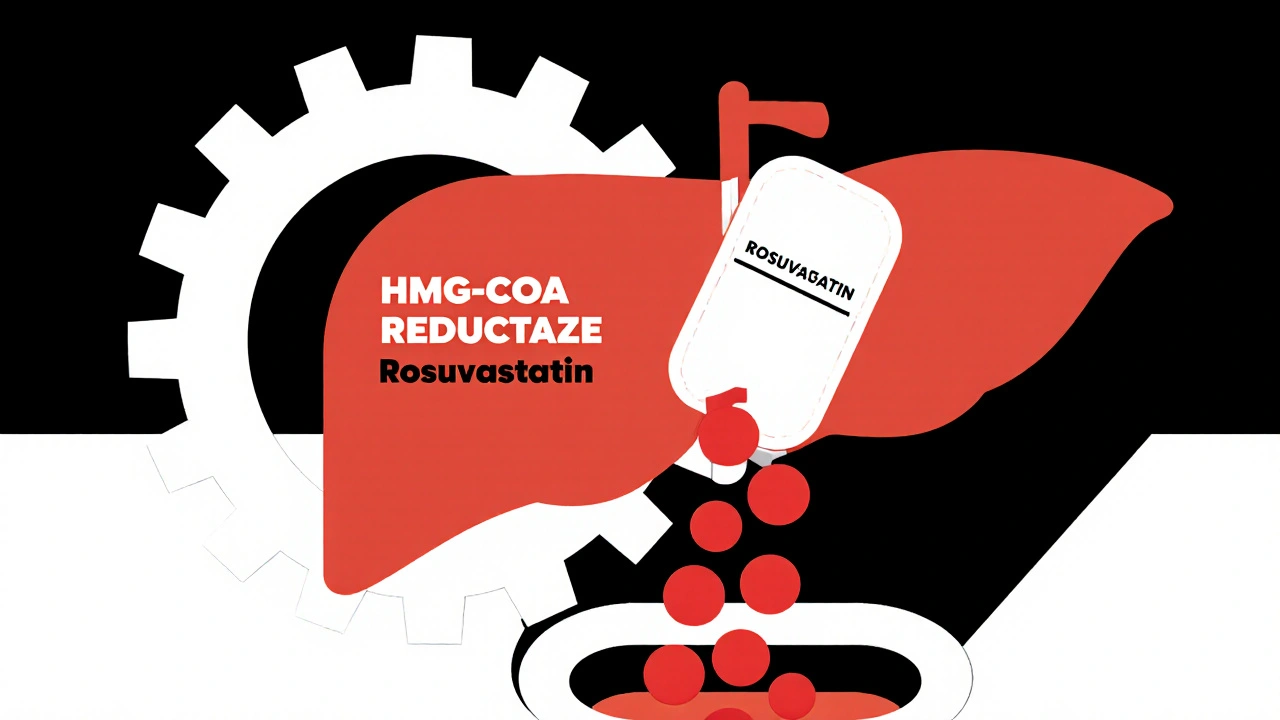
How Strong Is Rosuvastatin Really?
Rosuvastatin works by blocking HMG-CoA reductase, the enzyme your liver uses to make cholesterol. But it doesn’t just nudge the needle-it slams it. At a 20 mg daily dose, it can drop your LDL (bad) cholesterol by about 55%. Compare that to atorvastatin at 40 mg, which typically lowers LDL by 40%, or simvastatin at 40 mg, which only gets you around 30%. That’s why doctors reach for rosuvastatin when they need fast, deep cholesterol control.
The FDA and American College of Cardiology classify 20 mg and 40 mg doses as "high-intensity" statin therapy. That means it’s used for people with established heart disease, diabetes with risk factors, or very high LDL levels (over 190 mg/dL). It’s not a first-line choice for someone with borderline cholesterol. It’s reserved for when you need maximum effect.
One big advantage? Rosuvastatin doesn’t rely heavily on liver enzymes to break down. Only about 10% is processed by CYP2C9, unlike simvastatin or atorvastatin, which are mostly handled by CYP3A4. That means fewer dangerous interactions with common medications like antibiotics, antifungals, or even grapefruit juice. That’s why it’s often chosen for patients on multiple prescriptions.
What Side Effects Should You Actually Worry About?
Most people tolerate rosuvastatin well. But side effects do happen-and they’re not all the same. The biggest concerns fall into three buckets: muscles, liver, and blood sugar.
Muscle pain is the most common complaint. About 5-10% of users report mild aches or cramps, especially in the legs. This is usually harmless and goes away on its own. But if you feel deep, persistent pain, weakness, or your urine turns dark (like cola), stop taking it and call your doctor. That could be rhabdomyolysis-a rare but dangerous breakdown of muscle tissue that can damage your kidneys. The risk is under 0.1% in most studies, but it’s higher with doses above 20 mg, especially in older adults or those with kidney problems.
Liver enzymes can rise in a small number of people. The FDA no longer recommends routine monthly blood tests for this. Instead, doctors check ALT and AST before you start, then again at 3 months after starting or increasing the dose. If levels go above 3 times the normal limit, they’ll likely stop the drug. But if you feel fine and your numbers are stable? No need for yearly checks unless something changes.
Higher blood sugar is a real, documented effect. Studies show rosuvastatin can raise fasting glucose by 5-10 mg/dL and HbA1c by 0.1-0.3%. That’s not enough to cause diabetes in healthy people-but if you’re prediabetic, have a family history, or are overweight, it can push you over the edge. That’s why your doctor should check your HbA1c before starting and again at 3-6 months, especially if you’re over 50 or have metabolic syndrome.
Less common, but still important: proteinuria (protein in urine). At 40 mg, the risk of this increases by 2.3 times compared to 10 mg. It’s usually mild and doesn’t cause symptoms, but it’s a sign your kidneys might be under extra stress. If you’re on the 40 mg dose and have even mild kidney impairment, your doctor should reconsider the dose.
Who Should Avoid Rosuvastatin Altogether?
Not everyone can take rosuvastatin safely. The biggest red flag is kidney function. If your eGFR (a measure of kidney filtering ability) is below 60 mL/min/1.73m², you shouldn’t take the 40 mg dose. If it’s below 30, you shouldn’t take it at all. That’s because rosuvastatin is cleared mostly by the kidneys, not the liver. In kidney disease, the drug builds up, increasing side effect risks.
People with active liver disease, like hepatitis or cirrhosis, should also avoid it. And if you’ve had a previous allergic reaction to rosuvastatin or any statin, don’t restart it.
Women who are pregnant or breastfeeding shouldn’t take it. Statins cross the placenta and can harm fetal development. If you’re planning pregnancy, talk to your doctor about switching to a safer option like cholestyramine or lifestyle changes first.
What to Monitor and When
Monitoring isn’t about endless blood tests. It’s about smart, targeted checks at the right times.
- Before starting: Get a full lipid panel, ALT, AST, CK, eGFR, and HbA1c. This gives you a baseline.
- At 3 months: Repeat ALT, AST, eGFR, and HbA1c. This is when most side effects show up, if they’re going to.
- Annually: Lipid panel and eGFR. If you’re stable and feeling fine, you don’t need more frequent liver tests.
- When you feel something wrong: If you have unexplained muscle pain, weakness, or dark urine, get a CK test immediately. Don’t wait.
- If your dose changes: Always recheck liver enzymes and kidney function 3 months after increasing to 20 mg or 40 mg.
Some doctors now use patient-reported outcomes instead of just lab numbers. If you say your legs feel heavy or you’re more tired than usual, that matters-even if your CK is normal. Your experience is part of the data.
What to Do If Side Effects Happen
Let’s say you’re on 10 mg and start getting leg cramps every night. Don’t panic. Don’t stop cold turkey. Call your doctor.
They might:
- Lower your dose to 5 mg. Many people get 50% LDL reduction at 5 mg-enough for primary prevention.
- Switch you to pravastatin or fluvastatin. These are gentler on kidneys and muscles.
- Check for other causes: vitamin D deficiency, thyroid issues, or overtraining can mimic statin muscle pain.
If you’re on 40 mg and have proteinuria or elevated liver enzymes, your doctor will likely reduce you to 20 mg or less. That’s not failure-it’s smart management. You still get 45-50% LDL reduction at 20 mg, which is more than enough for most people.
And if you’ve been told you have "statin intolerance"? That doesn’t mean you can never take one again. Studies show up to 70% of people who quit statins due to side effects can tolerate a lower dose or a different one after a break.
Real Stories, Real Results
On Reddit, a 58-year-old man wrote: "Took 20 mg for 6 months. My LDL dropped from 178 to 72. Then I started getting calf cramps every night. My doctor cut me to 10 mg. Cramps gone in 10 days. LDL is 88. Still way better than before."
A 65-year-old woman in Sydney shared on a patient forum: "I was on simvastatin and kept getting liver spikes. My cardiologist switched me to rosuvastatin 10 mg. No more liver issues. My cholesterol’s stable. I take it with breakfast and forget about it."
But another user on Drugs.com wrote: "40 mg made me feel like I’d run a marathon every day. My CK was 2,100. They stopped it. Took 3 months to feel normal again."
These aren’t outliers. They’re common patterns. The drug works-but it’s not one-size-fits-all.
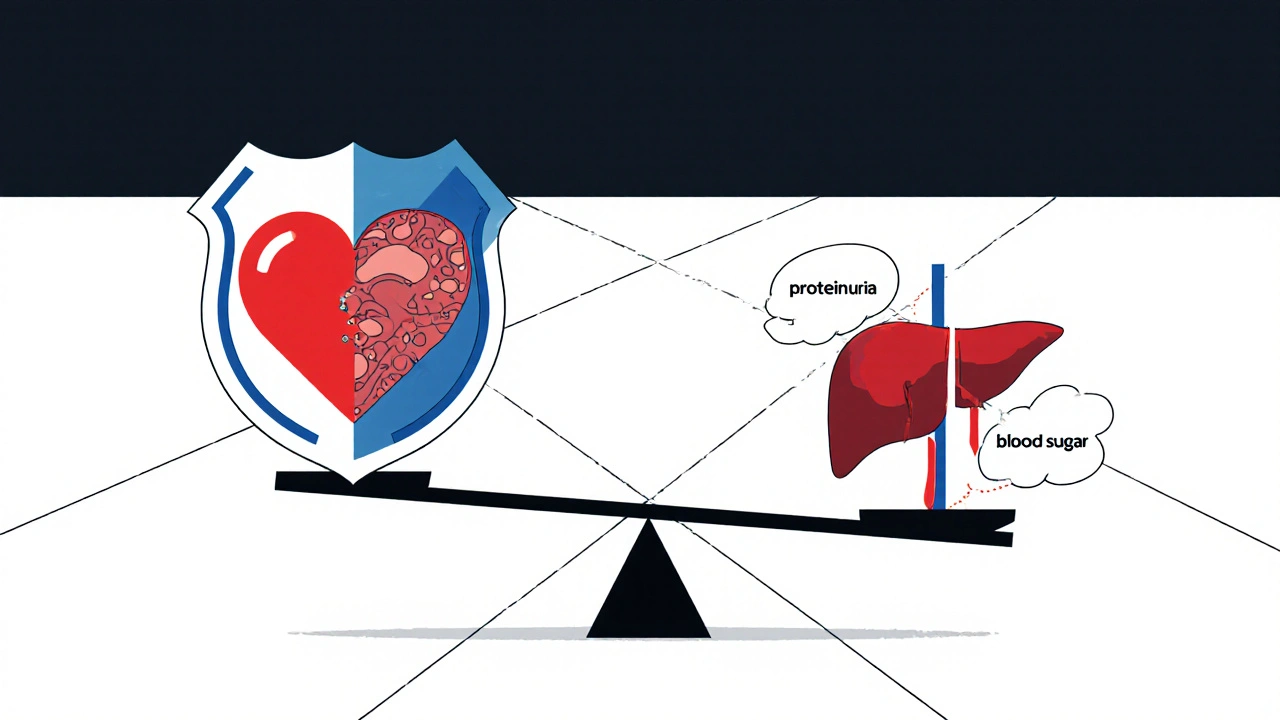
The Bigger Picture: Benefits vs. Risks
The JUPITER trial showed that for people with normal LDL but high inflammation (CRP), rosuvastatin cut heart attacks and strokes by 44%. That’s huge. The METEOR trial showed it actually reversed plaque buildup in arteries.
For every 100 people who take rosuvastatin for 5 years, about 2-3 heart attacks or strokes are prevented. Meanwhile, about 1-2 might develop diabetes they wouldn’t have otherwise. Muscle problems severe enough to stop the drug? Less than 1 in 100.
The math is clear: the benefit outweighs the risk-by a lot. But only if you’re monitored properly. Don’t skip your follow-ups. Don’t ignore muscle pain. Don’t assume "it’s just aging."
What’s Next?
Genetic testing for SLCO1B1 gene variants is starting to show up in lipid clinics. People with certain variants absorb rosuvastatin too well, raising their risk of muscle side effects. If you’ve had repeated problems with statins, ask your doctor if genetic testing could help.
Also, newer guidelines are pushing for lower doses in more people. You don’t always need 20 mg to get the job done. A 5 mg or 10 mg dose, paired with diet and exercise, can be enough for long-term safety and control.
Rosuvastatin is a powerful tool. But like any tool, it’s only as good as how you use it. Know your numbers. Listen to your body. And never be afraid to ask: "Is this dose still right for me?"
Can rosuvastatin cause memory loss or brain fog?
Some people report memory issues or brain fog while taking rosuvastatin, but these are rare-reported in about 1-2% of users. The FDA says these effects are usually mild and reversible once the drug is stopped. Most patients notice improvement within 2-3 weeks. There’s no strong evidence that rosuvastatin causes permanent cognitive damage. If you’re concerned, talk to your doctor before stopping.
Is it safe to take rosuvastatin with other medications?
Rosuvastatin has fewer drug interactions than other statins because it’s not heavily processed by liver enzymes. But it can still interact with cyclosporine, gemfibrozil, and some HIV or hepatitis C drugs. Always tell your doctor and pharmacist about everything you’re taking-even over-the-counter supplements. Avoid high-dose niacin and red yeast rice, which can increase muscle risk.
Why do I need to check my kidney function before taking rosuvastatin?
Rosuvastatin is cleared from your body mainly by your kidneys. If your kidneys aren’t working well, the drug builds up in your blood, raising the risk of muscle damage and other side effects. That’s why the 40 mg dose is banned if your eGFR is below 60, and completely avoided if it’s below 30. Checking kidney function isn’t optional-it’s essential for safety.
Can I take rosuvastatin if I have type 2 diabetes?
Yes, and you should. People with diabetes have a much higher risk of heart disease. Rosuvastatin reduces that risk significantly. However, it can slightly raise blood sugar levels, so your doctor will monitor your HbA1c more closely-usually every 3-6 months. The heart protection benefits far outweigh the small increase in glucose.
What’s the best time of day to take rosuvastatin?
You can take rosuvastatin at any time of day-morning, night, with or without food. Unlike older statins, it doesn’t matter when you take it because its half-life is long (about 19 hours). The key is consistency. Pick a time you won’t forget and stick with it.
Are there natural alternatives to rosuvastatin?
Diet, exercise, and weight loss can lower LDL by 10-20%. Plant sterols, soluble fiber (like oats and psyllium), and omega-3s help too. But none match the power of rosuvastatin. If your LDL is above 190 or you’ve had a heart event, natural methods alone won’t cut it. Rosuvastatin is the most effective option for high-risk patients. Use lifestyle changes to support it, not replace it.
How long do I need to stay on rosuvastatin?
For most people, it’s a lifelong medication. Cholesterol doesn’t fix itself. Stopping means your LDL will rise again, and your risk of heart attack or stroke returns. Unless your doctor says otherwise, keep taking it. If you’re worried about side effects, talk about lowering the dose instead of quitting.
Final Thoughts: Don’t Fear the Drug-Manage It
Rosuvastatin isn’t dangerous. It’s powerful. And like any powerful tool, it demands respect. The goal isn’t to avoid side effects at all costs-it’s to catch them early, adjust smartly, and keep your heart protected. Most people take it for years without issue. The ones who have problems? They’re usually the ones who didn’t get checked, ignored symptoms, or took the highest dose without need.
Know your numbers. Talk to your doctor. Don’t assume side effects are normal. And don’t stop without a plan. Your arteries will thank you.





Write a comment