Dosage: The Key to Safe and Effective Medication Use
When working with Dosage, the precise amount of a drug taken at one time or over a set period. Also known as dose, it directly influences therapeutic outcomes and side‑effect risk.
Accurate dosage is the bridge between a medication’s promise and its real‑world results. If the amount is too low, the drug may not work; too high and you invite unwanted side effects. This simple principle shows why dosage guidelines are built on patient weight, age, organ function, and disease severity. For example, lenalidomide’s dosing schedule for lupus differs from its oncology use because the disease pathways and safety profiles change. Likewise, doxycycline’s standard 100 mg twice daily for infections becomes a lower 40 mg daily dose when treating acne. These variations illustrate the first semantic triple: Dosage determines medication effectiveness.
Key Factors That Influence Dosage
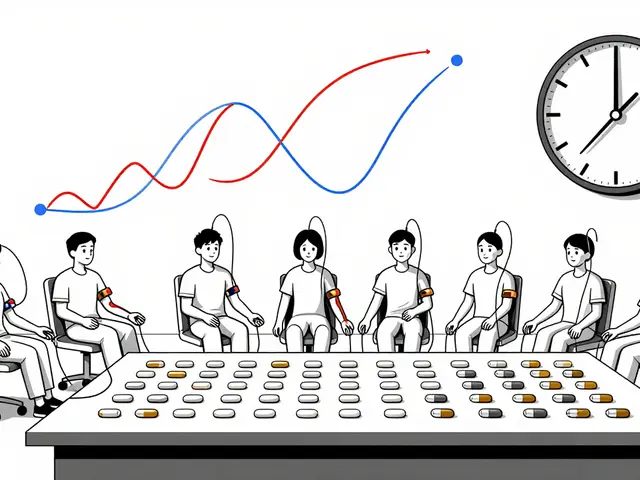
Understanding what drives dosage decisions helps you follow prescriptions with confidence. Three core factors dominate: patient characteristics, disease specifics, and drug properties. Patient characteristics include weight, renal and liver function, and concurrent medications. Disease specifics cover severity, chronic vs. acute status, and target tissue. Drug properties encompass half‑life, therapeutic window, and route of administration. When these elements align, clinicians can set a dose that maximizes benefit while minimizing harm – the second semantic triple: Accurate dosage reduces side effects.
Take the case of Lasix (furosemide). In heart failure, doctors often start with 20‑40 mg once daily, then adjust based on fluid loss and blood pressure. In hypertension without fluid overload, the same drug might be used at a lower 10 mg dose to avoid excessive diuresis. The dosage shift reflects how disease specifics shape dosing rules, reinforcing the link: Dosage guidelines depend on patient condition.
Another practical view comes from over‑the‑counter products like Imodium (loperamide). The standard adult dose is 2 mg after the first loose stool, then 2 mg after each subsequent one, not exceeding 8 mg in 24 hours. This ceiling protects against opioid‑related cardiac events, showing how drug properties (risk of QT prolongation) set upper limits. The same principle applies to prescription meds such as Cymbalta (duloxetine), where the starting dose is 30 mg daily, but patients with liver impairment may need a reduced 20 mg dose.
When you shop for generic drugs online, dosage information stays critical. Whether you’re buying cheap generic doxycycline, gabapentin, or lisinopril, you must verify that the pharmacy lists the correct strength (e.g., 100 mg tablets vs. 50 mg). Mistaking the strength could double your dose unintentionally. This is why safe online purchasing guides stress checking the dosage label, matching it to your prescription, and consulting a pharmacist if anything looks off.
All these examples tie back to the central idea that dosage isn’t a static number; it’s a dynamic decision based on multiple interrelated entities. Below you’ll find a curated list of articles that dive deeper into specific drugs, dosing strategies, safety tips, and buying guides. Use them to sharpen your understanding, compare dosing regimens, and make informed choices about your health regimen.
- By Percival Harrington
- /
- 7 Oct 2025
Diamox (Acetazolamide) vs Alternatives: In‑Depth Comparison
A clear, side‑by‑side comparison of Diamox (acetazolamide) with common alternatives, covering uses, dosing, side effects, and how to pick the right drug.