Leishmaniasis Treatment: What Works, What to Avoid, and Where to Find Help
When you're dealing with leishmaniasis treatment, a set of medical approaches used to combat parasitic infections caused by Leishmania protozoa, transmitted by sandfly bites. Also known as kala-azar, visceral leishmaniasis, or cutaneous leishmaniasis depending on the form, this disease affects over a million people each year—mostly in tropical and subtropical regions, but also in parts of Europe and the Americas. It’s not just a travel risk; it’s a public health issue with real consequences if left untreated.
Not all leishmaniasis treatment options are created equal. Antimonial drugs, like sodium stibogluconate, have been the go-to for decades, but resistance is growing in places like India. That’s why alternatives like amphotericin B, a powerful antifungal repurposed for parasites, are now preferred in many cases—especially for the deadly visceral form. Miltefosine, the first oral drug approved for leishmaniasis, changed the game by making treatment possible outside hospitals, but it comes with strict pregnancy warnings and side effects like nausea and liver stress. These aren’t just drug names—they’re life-or-death choices shaped by geography, cost, and access.
What you won’t find in most guides is how often treatment fails because it’s started too late—or because the wrong type is chosen. Cutaneous leishmaniasis might heal on its own, but it leaves scars. Visceral leishmaniasis kills if untreated. And in places with weak health systems, patients often wait months before getting diagnosed. Even then, some clinics still rely on outdated protocols. The real challenge isn’t just finding the right drug—it’s getting the right drug to the right person at the right time.
There’s also a quiet gap in care: people who’ve been treated but still struggle with long-term symptoms. Nerve pain, fatigue, or recurring skin lesions don’t always show up in clinical trials, but they’re real for those living with the aftermath. That’s why some of the posts below dive into drug interactions, side effect monitoring, and how immune status affects recovery—topics that matter if you’re managing this condition long-term.
What you’ll find here aren’t just lists of drugs. You’ll see real comparisons—how miltefosine stacks up against amphotericin B, why some patients need combination therapy, and what alternatives exist when first-line treatments fail. You’ll also find guidance on recognizing warning signs, avoiding dangerous interactions, and knowing when to push for better care. This isn’t theoretical. It’s what people on the ground need to survive.
- By Percival Harrington
- /
- 5 Nov 2025
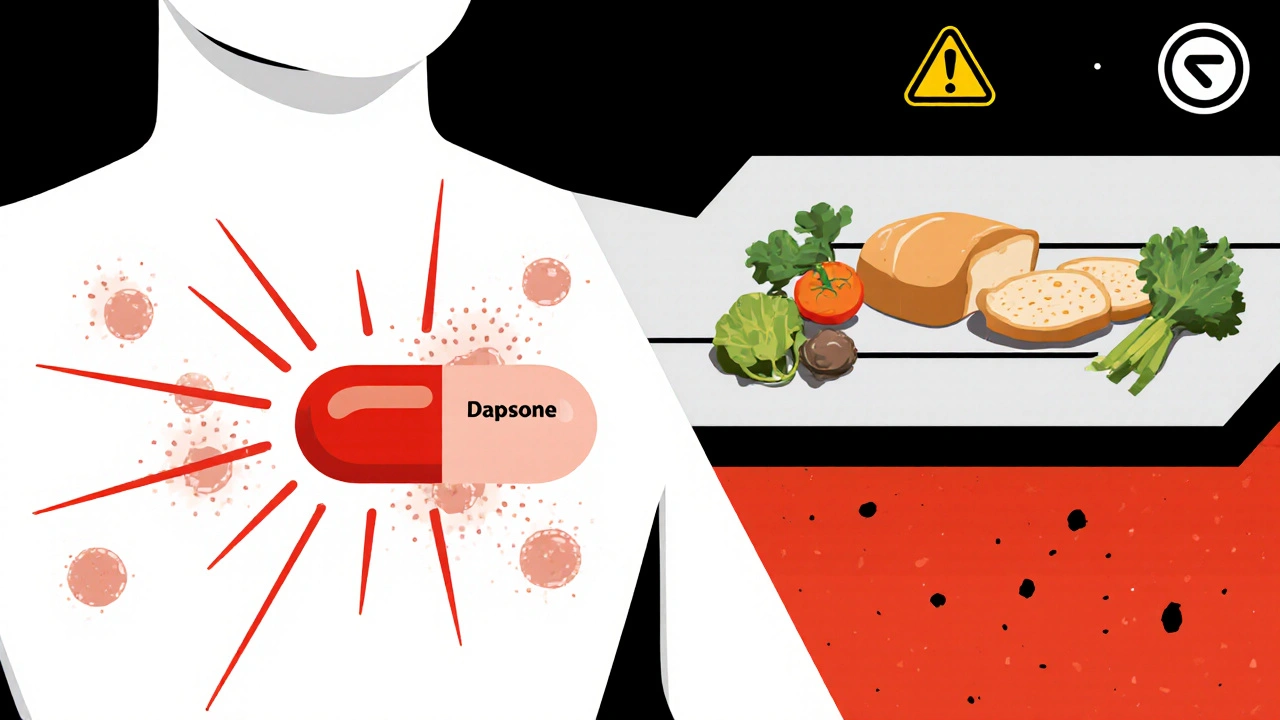
Dapsone vs Alternatives: What Works Best for Skin Conditions Like Leishmaniasis and Dermatitis Herpetiformis
Dapsone treats skin conditions like dermatitis herpetiformis and leishmaniasis, but it has serious side effects. Learn about safer, more effective alternatives including colchicine, miltefosine, and gluten-free diets.