DOAC Obesity Dosing Assistant
Patient Assessment
Recommendation
When you’re overweight or obese, taking blood thinners isn’t as simple as picking up a prescription and going about your day. For millions of people with body mass index (BMI) over 40 kg/m² or weighing more than 120 kg, the question isn’t just whether a direct oral anticoagulant (DOAC) will work - it’s whether the standard dose will work at all. The answer, based on the latest data from 2023 and 2024, is mostly yes - but with important exceptions.
Why Obesity Changes the Game
Obesity isn’t just about weight. It changes how your body absorbs, distributes, and clears medications. That’s especially true for anticoagulants, where even small shifts in drug levels can mean the difference between preventing a clot and causing a bleed. The original clinical trials for DOACs - apixaban, rivaroxaban, dabigatran, and edoxaban - included very few people with severe obesity. Most participants had BMIs under 35. So when doctors started prescribing these drugs to patients with BMI 40, 50, or even higher, they were flying blind.Apixaban: The Most Reliable Choice
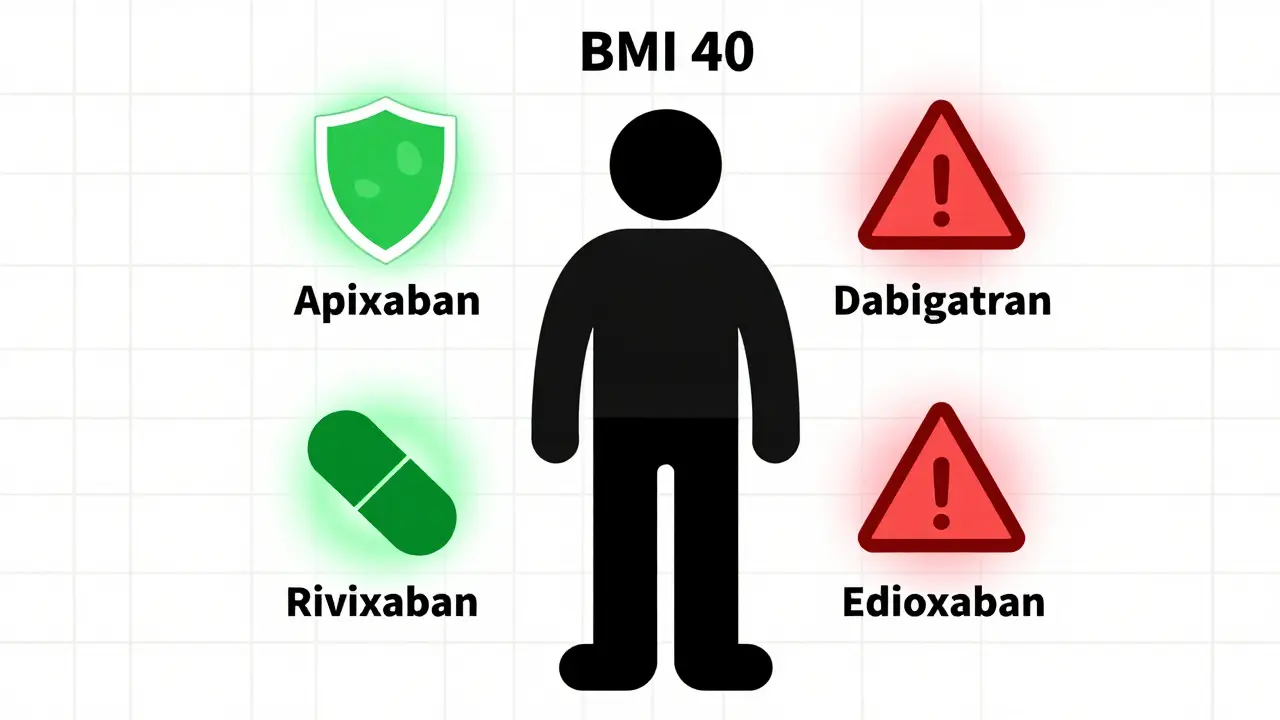
If you’re obese and need a blood thinner, apixaban is the safest bet. Multiple studies - including a 2020 meta-analysis of over 15,000 patients - show it works just as well in people with BMI over 40 as it does in those with normal weight. The standard dose - 5 mg twice daily for atrial fibrillation, or 10 mg twice daily for the first week of deep vein thrombosis treatment - remains effective and safe. A 2022 registry of 2,147 obese patients found zero thrombotic events in those on standard-dose apixaban, even among those with BMI over 40. Major bleeding rates were around 2.1% per year - no worse than in non-obese patients. The International Society on Thrombosis and Haemostasis (ISTH) says clearly: use standard doses of apixaban regardless of weight or BMI. There’s no need to increase the dose. No need to check blood levels. Just prescribe the same dose you’d give anyone else. And if the patient is over 80, weighs under 60 kg, or has kidney issues? Drop to 2.5 mg twice daily - same as for non-obese patients.Rivaroxaban: Almost as Good
Rivaroxaban is a close second. For atrial fibrillation, 20 mg once daily (or 15 mg if kidney function is low) is effective and safe in obese patients. For treating clots, the initial 15 mg twice daily for three weeks, followed by 20 mg once daily, works without adjustment. A 2021 review of 28 studies found no increase in bleeding or clotting with standard rivaroxaban doses in patients weighing over 120 kg. The European Heart Rhythm Association and the Anticoagulation Forum both endorse this approach. Like apixaban, there’s no evidence that higher doses help - and there’s no reason to try them.Dabigatran: Proceed With Caution
This is where things get risky. Dabigatran is the outlier. While it still prevents strokes in obese patients with atrial fibrillation, it significantly increases the chance of serious gastrointestinal bleeding. Data from the ISTH 2021 update shows that patients with BMI over 40 have a 37% higher risk of GI bleeding on dabigatran compared to those with normal weight. One study found a 2.3-fold increase in major GI bleeds in the morbidly obese. That’s not a small risk - it’s a red flag. If a patient has a history of ulcers, GERD, or stomach issues, dabigatran should be avoided entirely. Even without those problems, the bleeding risk is too high to justify using it over apixaban or rivaroxaban. The European Heart Rhythm Association and the Anticoagulation Forum both say: use dabigatran with caution in obesity. Many experts now avoid it altogether in patients with BMI over 40.
Edoxaban: Mostly Safe - But Watch the Very Heavy
For most obese patients, edoxaban at standard doses (60 mg once daily for AF, 30 mg for reduced kidney function) works fine. Studies show drug levels and anti-Xa activity stay within therapeutic range even at BMI over 50. But here’s the catch: in patients with BMI over 50 or weight over 160 kg, some clinicians have seen subtherapeutic levels. A 2021 study from Massachusetts General Hospital found that 18.2% of patients with BMI over 50 on standard-dose edoxaban had levels too low to prevent clots. That’s nearly 1 in 5. The 2023 ACC/AHA/ACCP/HRS guidelines suggest considering the reduced dose (30 mg) for these extreme cases - not because it’s safer, but because we don’t yet know if the standard dose is enough. Until more data comes in, some providers are opting for therapeutic drug monitoring in patients with BMI over 50. That means checking anti-Xa levels to make sure the drug is working.What About Warfarin?
You might think, “Why not just use warfarin? We’ve been monitoring it for decades.” But warfarin isn’t better - it’s harder. It requires frequent blood tests, dietary restrictions, and interacts with dozens of medications. In obese patients, warfarin dosing is even more unpredictable because fat tissue changes how the drug is distributed. Studies show DOACs are just as effective as warfarin in obese patients - and safer. The 2023 ACC/AHA guideline gives DOACs a Class IIa recommendation for stroke prevention in AF, even for those with obesity. That means they’re preferred over warfarin.What to Avoid
Don’t increase the dose. No matter how heavy the patient, there’s no evidence that doubling apixaban or rivaroxaban improves outcomes - and it increases bleeding risk. Don’t switch to warfarin just because the patient is obese. Don’t skip the drug entirely out of fear. The biggest mistake? Assuming that because a patient is heavy, they need a higher dose. That’s not how DOACs work. They’re designed to be fixed-dose. Their pharmacokinetics don’t change enough in obesity to require adjustment - except in rare, extreme cases.
Real-World Numbers Don’t Lie
In the U.S., over 42% of adults are obese. Nearly 1 in 10 are morbidly obese. Since 2016, DOAC prescriptions for obese patients have jumped from 32% to 78%. Why? Because doctors saw the results: fewer clots, fewer bleeds, fewer hospital visits. A 2020 study tracking 4,821 obese AF patients found stroke rates were nearly identical to those with normal weight: 1.41 vs. 1.32 per 100 patient-years. Major bleeding? 2.38 vs. 2.33. No difference. That’s the power of evidence-based dosing.What’s Next?
The DOAC-Obesity trial (NCT04588071) is now enrolling 500 patients with BMI over 40. Results are expected in late 2024. It’s the first large study designed specifically for this group. Until then, we rely on the data we have. Experts agree: for most obese patients, apixaban and rivaroxaban are the clear winners. Dabigatran should be avoided. Edoxaban is fine for most, but watch those over 160 kg. And never, ever guess the dose.Bottom Line
If you’re obese and need a blood thinner:- Choose apixaban - it’s the most proven, safest option.
- Rivaroxaban is a solid alternative.
- Avoid dabigatran - too much risk of stomach bleeding.
- Use edoxaban with caution if you weigh over 160 kg.
- Stick to standard doses. Don’t increase them.
- Don’t go back to warfarin unless there’s no other choice.





Write a comment