Immunodeficiency Mental Health Risk Calculator
Mental Health Risk Assessment
This tool calculates relative risk of depression and anxiety based on immunodeficiency type using clinical study data from the article.
Did you know that people living with a weakened immune system are up to three times more likely to develop depression? Immunodeficiency and mental health may sound like two unrelated topics, but scientists are uncovering a web of biological signals that link them. This article breaks down the science, shows what the latest research says, and gives you practical tips for handling both sides of the coin.
What is Immunodeficiency?
Immunodeficiency is a condition where the body’s defense system fails to protect against infections, tumors, or autoimmune attacks. It can be congenital (primary) or acquired (secondary), and the severity ranges from mild antibody gaps to life‑threatening leukocyte defects. Primary immunodeficiency diseases (PIDD) affect about 1 in 1,200 people, while secondary forms arise from HIV, chemotherapy, or long‑term steroids.
What Do We Mean by Mental Disorders?
Mental disorders are clinical conditions that affect mood, thinking, or behavior, often causing distress or functional impairment. The most common are depression, anxiety, and schizophrenia, but the spectrum also includes bipolar disorder, PTSD, and obsessive‑compulsive disorder.
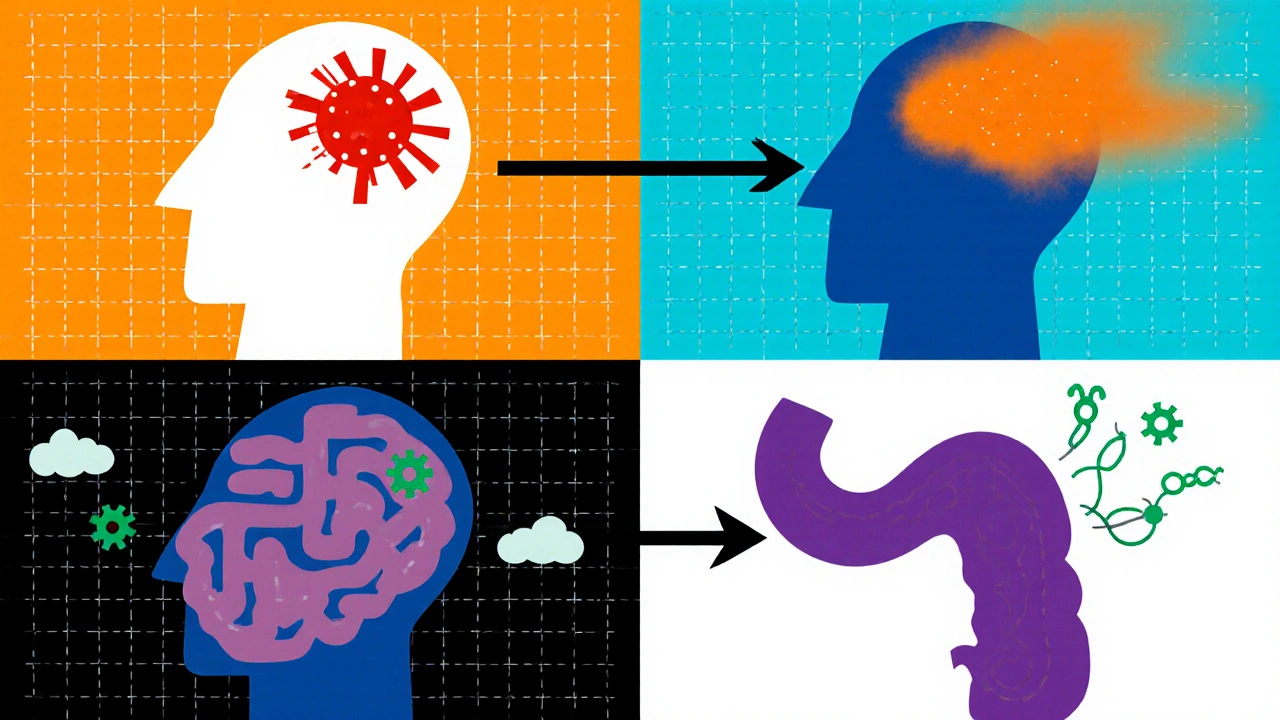
Why the Immune System Talks to the Brain
Four biological pathways keep the immune system and the brain in constant conversation.
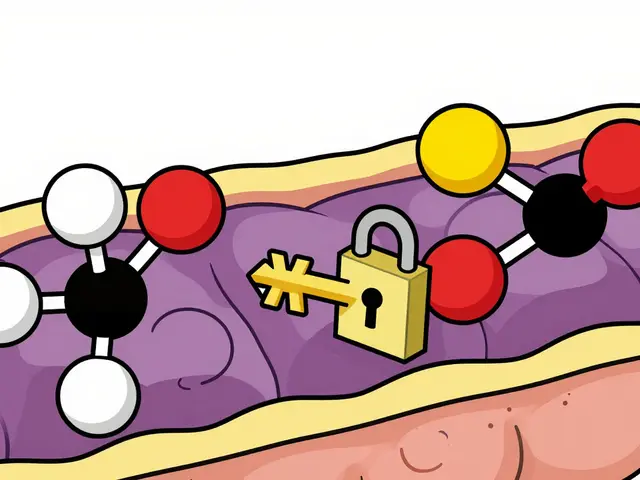
- Cytokine imbalance: When immune cells release too many pro‑inflammatory cytokines (like IL‑6, TNF‑α), they can cross the blood‑brain barrier and tweak neurotransmitter production.
- Chronic inflammation: Persistent low‑grade inflammation nudges the brain toward a depressive‑like state by altering serotonin and dopamine pathways.
- Gut‑brain axis: The gut microbiome produces metabolites that influence both immunity and mood. Dysbiosis-common in immunodeficient patients-often coincides with anxiety and depression.
- Stress hormones: An overactive hypothalamic‑pituitary‑adrenal (HPA) axis spikes cortisol, suppressing immune function while also heightening anxiety.
Evidence from Recent Studies
Researchers have published dozens of papers linking immune deficits to mental health outcomes. A 2023 meta‑analysis of 45 cohort studies found that individuals with primary immunodeficiency had a 2.8‑fold higher odds of depression compared to the general population. Another 2024 longitudinal study of 12,000 patients on long‑term corticosteroids reported a 30% rise in anxiety scores after just six months of treatment.
Case reports also illustrate the connection. A teenager with X‑linked agammaglobulinemia (a PIDD) developed severe social withdrawal, which improved dramatically after immunoglobulin replacement therapy restored normal cytokine levels.
Practical Implications for Patients and Clinicians
If you or someone you care for lives with immunodeficiency, consider mental health a core part of the treatment plan.
- Screen regularly: Use brief tools like PHQ‑9 for depression and GAD‑7 for anxiety during routine check‑ups.
- Address inflammation: Anti‑inflammatory diets (rich in omega‑3s, fiber, and antioxidants) can lower cytokine spikes.
- Support the gut: Probiotic strains such as Bifidobacterium longum have shown promise in reducing anxiety scores in immunocompromised patients.
- Monitor medications: Steroids and certain biologics can worsen mood; discuss dose‑adjustments with your physician.
- Promote sleep hygiene: Adequate rest balances cortisol and supports both immunity and mood.

How Common Are These Overlaps? A Quick Comparison
| Group | Depression Rate | Study Sample Size |
|---|---|---|
| General Population | 7% | 10,000 |
| Primary Immunodeficiency (PIDD) | 20% | 1,200 |
| Secondary Immunodeficiency (e.g., HIV, chemotherapy) | 25% | 3,500 |
These numbers underline that mental health screening is not optional-it’s a preventive measure.
Checklist for Managing the Dual Challenge
- Schedule a mental‑health review at least once a year.
- Ask your doctor about cytokine‑targeted therapies if inflammation feels “constant.”
- Include probiotic‑rich foods (yogurt, kefir, fermented vegetables) in daily meals.
- Track mood changes alongside infection episodes; patterns can guide treatment.
- Connect with support groups for immunodeficient patients-shared experience reduces isolation.
Frequently Asked Questions
Can immunodeficiency cause anxiety?
Yes. Chronic infection risk and ongoing medical appointments trigger stress hormones, which can lead to persistent worry and panic attacks.
Do immunoglobulin replacements improve mood?
In many patients, restoring antibody levels reduces infection‑driven inflammation, and several case series report noticeable mood lifts within weeks.
Is there a direct test for cytokine‑related depression?
Not yet in routine clinical practice. Research labs can measure IL‑6 or TNF‑α, but the results are still experimental for diagnosing depression.
How does the gut‑brain axis affect patients with weak immunity?
A compromised gut barrier lets bacterial products leak into circulation, sparking inflammation that reaches the brain and can worsen anxiety or depressive symptoms.
Should I avoid all probiotics if I have an immunodeficiency?
Most research supports safe, well‑studied strains like Lactobacillus rhamnosus. However, severely immunocompromised patients should discuss any supplement with their doctor first.
Understanding the bridge between a fragile immune system and mental health opens doors to better care. By screening early, tackling inflammation, and nurturing the gut, patients can keep both their bodies and minds in better shape.




Write a comment