Every year, millions of people reach for ibuprofen or naproxen to ease a headache, back pain, or arthritis flare-up. It’s quick, cheap, and seems harmless-until it isn’t. The truth is, NSAIDs aren’t just harmless pain relievers. They quietly damage your stomach, kidneys, and gut in ways you might not notice until it’s too late. If you’ve been taking them for weeks or months, you’re not alone-but you might be at risk.
How NSAIDs Hurt Your Stomach (Even When You Feel Fine)
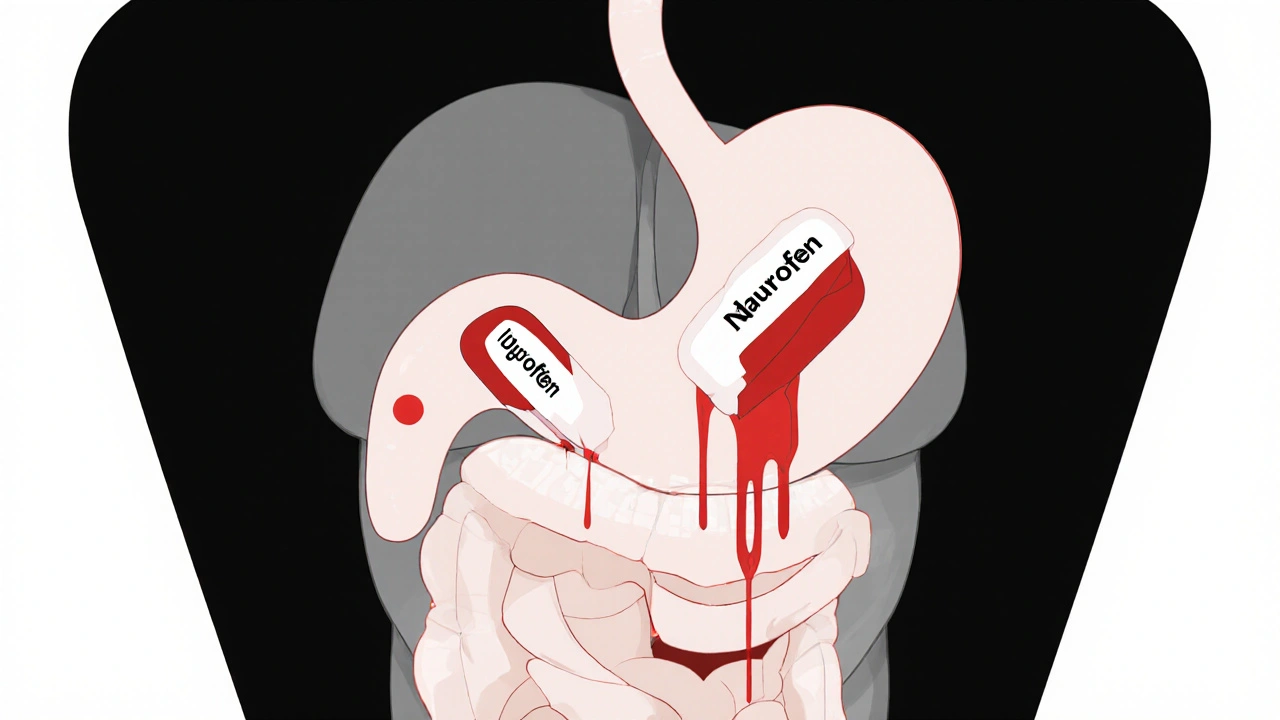
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 causes inflammation and pain, so blocking it helps. But COX-1 protects your stomach lining by producing prostaglandins-natural chemicals that keep mucus and blood flow steady. When NSAIDs shut down COX-1, your stomach loses its shield. That’s when ulcers form, bleeding starts, and you might not feel a thing until you’re vomiting blood or passing black, tarry stools.
Here’s the scary part: about half of all NSAID-related stomach damage shows no warning signs. You won’t get heartburn. You won’t feel pain. You just wake up one day with iron deficiency anemia because your gut has been bleeding slowly for weeks. A 2023 study from the American College of Gastroenterology found that NSAIDs cause over 107,000 hospitalizations and 16,500 deaths in the U.S. every year-mostly from silent bleeding.
Even over-the-counter doses add up. Taking 400 mg of ibuprofen three times a day for two weeks? That’s enough to increase your risk of a stomach ulcer by 40%. And it’s not just the stomach. NSAIDs also damage the small intestine, causing inflammation, ulcers, and leaks. Unlike stomach ulcers, there’s no reliable way to prevent or fully treat this lower GI damage. No pill, no supplement, no magic fix.
Your Kidneys Aren’t Immune Either
Your kidneys rely on prostaglandins to keep blood flowing, especially when you’re dehydrated, sick, or have high blood pressure. NSAIDs block those same prostaglandins. That’s why kidney problems are one of the most underreported side effects.
Acute kidney injury can happen in 1% to 5% of NSAID users-even healthy ones. For people over 65, with diabetes, heart failure, or existing kidney disease, the risk jumps dramatically. The FDA now requires a boxed warning on all prescription NSAIDs for kidney risks in older adults. Chronic use can lead to interstitial nephritis, papillary necrosis, and even permanent loss of kidney function.
Many patients don’t know their kidneys are under stress because symptoms are vague: fatigue, swelling in the ankles, or just feeling off. By the time creatinine levels spike, damage may already be done. A 2023 Medicare analysis found only 52% of NSAID users had their kidney function checked within 90 days of starting the drug. That’s not monitoring-that’s waiting for disaster.
Not All NSAIDs Are Created Equal
Some NSAIDs are riskier than others. Naproxen, for example, carries a 4.2 times higher risk of upper GI bleeding than not taking any NSAID. Celecoxib, a COX-2 inhibitor, has about half that risk-but it’s not risk-free. It still affects the kidneys and can cause fluid retention, leading to swollen legs or high blood pressure.
Here’s what the data shows:
| NSAID | GI Bleeding Risk (vs. non-user) | Kidney Risk | Cardiovascular Risk |
|---|---|---|---|
| Naproxen | 4.2x | High | Moderate |
| Ibuprofen | 2.7x | High | High (especially at >1200 mg/day) |
| Celecoxib | 1.9x | Medium | Medium |
| Diclofenac | 3.5x | High | High |
For most people, the lowest effective dose for the shortest time is the safest approach. If you need long-term pain control, talk to your doctor about alternatives like physical therapy, acetaminophen, or topical treatments. NSAIDs should be a last resort, not a daily habit.

Monitoring: What You Need to Check and When
If you’re on NSAIDs for more than a few weeks, you need a monitoring plan. Not a suggestion-a necessity. Here’s what your doctor should track:
- Serum creatinine and eGFR: Check within 30 days of starting, then every 3-6 months if you’re over 60, have high blood pressure, or kidney disease.
- Complete blood count (CBC): Look for low hemoglobin or hematocrit-signs of slow, hidden bleeding.
- Fecal occult blood test: Recommended every 6 months for high-risk patients (age >65, history of ulcers, on blood thinners).
- Blood pressure: NSAIDs can raise it. Monitor monthly if you’re hypertensive.
Don’t wait for symptoms. By the time you feel sick, the damage may already be advanced. A 2022 study showed patients who had regular kidney checks were 40% less likely to develop severe kidney injury.
When PPIs Don’t Help-and Might Make Things Worse
Doctors often prescribe proton pump inhibitors (PPIs) like omeprazole alongside NSAIDs to protect the stomach. That sounds smart-but it’s not a cure-all. PPIs reduce upper GI ulcers by 70-90%, but they do nothing for the small intestine. Worse, long-term use (4-12 months) increases the risk of microscopic colitis by more than six times, according to the American Gastroenterological Association.
And here’s another hidden danger: combining PPIs with SSRIs (common antidepressants) can triple your risk of bleeding. If you’re on both, ask your doctor if you really need both.
Many patients stop taking their PPI because they feel fine. But that’s exactly when the risk spikes. One Reddit user wrote: “I stopped my omeprazole after three months. Two weeks later, I ended up in the ER with a bleeding ulcer.”
Who’s at Highest Risk?
Not everyone needs the same level of caution. Use this quick checklist to assess your risk:
- Age over 65 (add 2 points)
- History of stomach ulcer or GI bleeding (add 3 points)
- Taking blood thinners like warfarin or aspirin (add 2 points)
- Using corticosteroids (add 1 point)
- Having kidney disease, heart failure, or high blood pressure (add 1 point each)
If your total is 4 or higher, you’re high risk. That means you should avoid NSAIDs if possible. If you must use them, you need a PPI, regular kidney checks, and a plan to stop as soon as you can.
The Bottom Line: Use Smart, Not Just Often
NSAIDs are powerful tools-but they’re not harmless. They’re like a chainsaw: great for cutting wood, dangerous if you use them without training or safety gear.
If you’ve been taking them daily for months, ask yourself: Do I still need them? Could I try stretching, heat therapy, or physical therapy instead? Is there a lower-dose option? Are my kidneys and stomach being checked?
Every extra week on NSAIDs increases your risk of complications by 3-5%. That’s not a small number. It’s a ticking clock.
There’s no perfect NSAID. But there is a smarter way to use them: the lowest dose, for the shortest time, with the right monitoring. And if you’re over 65, have kidney issues, or have ever had a stomach ulcer-talk to your doctor before the next pill.
Can I take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and reduce the effectiveness of some blood pressure medications. If you have hypertension, avoid long-term use. Ibuprofen and diclofenac are especially risky. Naproxen may be slightly safer, but still requires close monitoring. Always check with your doctor before starting.
Are there NSAIDs that don’t hurt the kidneys?
No. All NSAIDs affect kidney function by reducing blood flow. Some, like celecoxib, may be slightly less harmful in people with normal kidneys, but none are safe for long-term use in those with existing kidney disease. The American College of Cardiology now advises avoiding all NSAIDs in patients with stage 3 or worse chronic kidney disease.
How do I know if I’m bleeding internally from NSAIDs?
Signs include fatigue, pale skin, shortness of breath, or dark, tarry stools. But many people have no symptoms at all. The only reliable way to catch hidden bleeding is through a blood test (CBC for low hemoglobin) and a fecal occult blood test. Don’t wait for symptoms-get tested if you’ve been on NSAIDs for more than 4 weeks.
Is it safe to take NSAIDs with alcohol?
No. Alcohol increases stomach irritation and bleeding risk. Combining it with NSAIDs can cause ulcers and bleeding even in people who’ve never had stomach problems. Avoid alcohol completely while taking NSAIDs, especially if you’re over 50 or have a history of ulcers.
What are safer alternatives to NSAIDs for chronic pain?
For joint pain, try physical therapy, weight loss, heat/cold therapy, or topical capsaicin. For headaches or mild pain, acetaminophen (Tylenol) is often safer-though it’s not anti-inflammatory. For inflammatory conditions like arthritis, disease-modifying drugs (DMARDs) or biologics may be options. Always discuss alternatives with your doctor before stopping NSAIDs.
What to Do Next
If you’re currently taking NSAIDs regularly:
- Check your last kidney test result. If it’s older than 3 months, schedule one.
- Ask your doctor if you need a CBC or fecal occult blood test.
- Review your dose. Can you lower it? Can you cut back to every other day?
- Consider non-drug options: stretching, yoga, massage, or acupuncture.
- If you’re on a PPI, ask if you still need it-or if you’ve been on it too long.
NSAIDs aren’t evil. But they’re not harmless either. The safest choice isn’t always the easiest one. It’s the one that keeps you healthy long after the pain is gone.






Write a comment