Steroid Insulin Calculator
Steroid-Induced Hyperglycemia Calculator
When you're prescribed steroids like prednisone or dexamethasone for inflammation, asthma, or an autoimmune flare, your blood sugar can spike-even if you’ve never had diabetes before. This isn’t a coincidence. It’s steroid-induced hyperglycemia, a well-documented and often dangerous side effect that affects up to 40% of hospitalized patients on these drugs. The problem isn’t just high numbers on the glucometer. It’s what happens when you don’t adjust your diabetes meds properly. Too little insulin? Your blood sugar climbs, risking kidney damage, infections, and longer hospital stays. Too much insulin as the steroids taper off? You could crash into hypoglycemia-shaking, sweating, confused, even unconscious. And it’s more common than you think: 30-40% of patients get hypoglycemic because their insulin wasn’t reduced fast enough after the steroid dose dropped.
Why Steroids Raise Blood Sugar
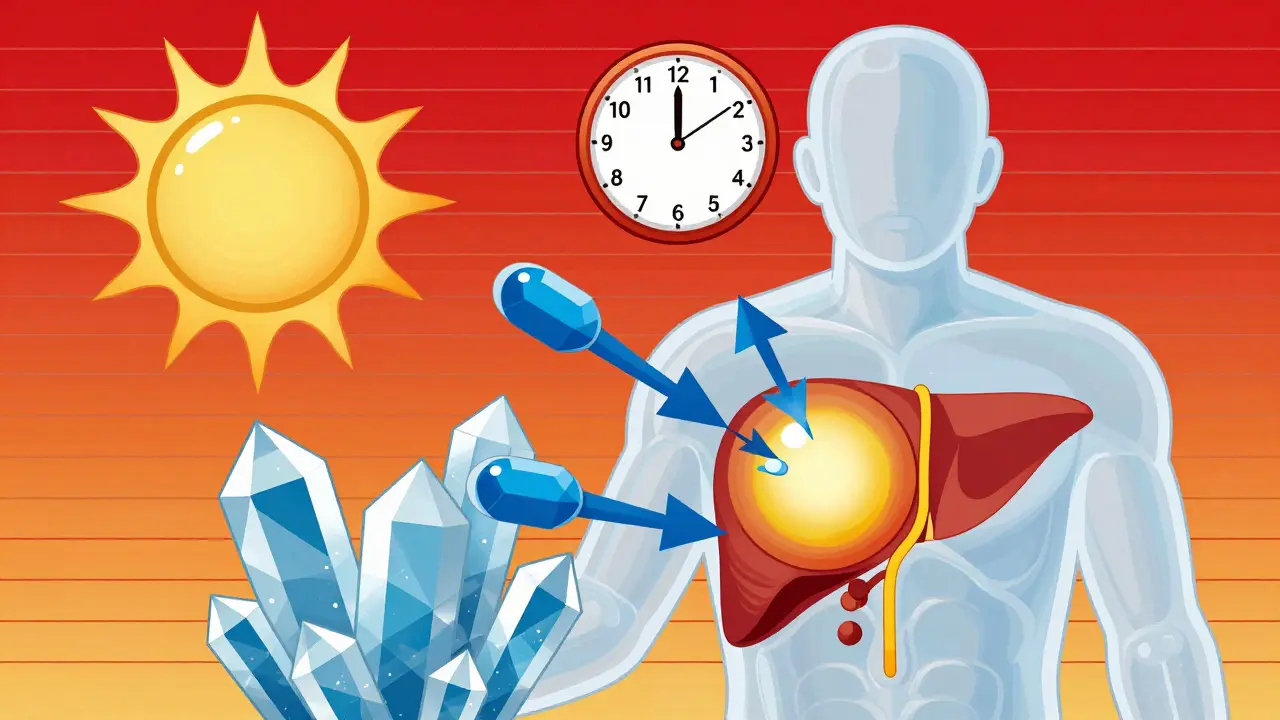
Steroids don’t just make you feel better-they change how your body uses sugar. They make your liver pump out more glucose, even when you’re not eating. At the same time, they block insulin from doing its job, so your muscles and fat cells can’t pull sugar out of the blood. Your pancreas tries to compensate by making more insulin, but over time, it can’t keep up. This combo-more sugar in, less sugar out-creates high blood glucose fast. The rise usually starts 4 to 8 hours after you take the steroid, peaks around 24 hours, and can linger for days after you stop.Insulin Is the First-Line Tool
For most people, especially those in hospital or on high-dose steroids, insulin is the only reliable way to control this spike. Oral diabetes pills like metformin or sulfonylureas are too slow, too unpredictable, and sometimes dangerous. Sulfonylureas, in particular, are risky: a Johns Hopkins study found 27% of patients on these drugs had emergency visits for low blood sugar during steroid tapering. That’s because sulfonylureas keep forcing your pancreas to release insulin-even when the steroid is gone and your body doesn’t need it anymore. Insulin, on the other hand, can be precisely matched to the steroid’s timing. For example, if you’re on prednisone (which lasts 18-36 hours), a single morning dose of NPH insulin works best because it peaks right when the steroid does. If you’re on dexamethasone (which lasts 36-72 hours), a long-acting insulin like glargine or detemir given in the morning covers the prolonged effect. No need to guess. No need to wait for a crisis. Start with a calculated dose.How Much Insulin to Start With
There’s no one-size-fits-all number, but there’s a clear starting point. For patients new to insulin during steroid therapy, guidelines recommend beginning with 0.1 unit per kilogram of body weight. So if you weigh 70 kg, that’s 7 units total per day. Split it: half as basal (background) insulin, half as bolus (meal) insulin. Then adjust based on your glucose readings. Here’s a simple rule for correction doses: if your pre-meal blood sugar is between 11.1 and 16.7 mmol/L (200-300 mg/dL), give 0.04 units per kg. If it’s above 16.7 mmol/L (300 mg/dL), give 0.08 units per kg. These aren’t guesses-they’re evidence-based. A 2021 study in Diabetes Care showed this approach cut average blood sugar from 12.7 to 10.2 mmol/L within days.Adjusting for Pre-Existing Diabetes
If you already have diabetes, your insulin needs will jump. Type 1 patients typically need a 30-50% increase in total daily insulin. Type 2 patients usually need 20-30%. The exact amount depends on your steroid dose and how high your sugars go. Don’t just double your usual dose. Start with a 20% increase, monitor closely, then adjust every 24 hours. For example, if you normally take 40 units a day and start prednisone at 40 mg, begin with 48 units. Check your sugars before meals and at bedtime. If your fasting glucose stays above 11.1 mmol/L for two days in a row, bump your basal insulin by 10-20%.
The Tapering Trap
The biggest mistake? Not reducing insulin as the steroid dose drops. Steroid effects fade slowly-3 to 4 days after the last dose. But many doctors forget to adjust insulin. Patients do, too. A 2023 survey found 68% of people didn’t know when to cut back. One Reddit user, ‘Type1Since99,’ shared: ‘On 40mg prednisone, I needed 50% more basal and 75% more bolus. When I dropped to 20mg, my endo didn’t reduce my insulin fast enough. I had three hypos in two days.’ This is preventable. The Joint British Diabetes Societies (JBDS) recommends a simple rule: reduce your insulin doses in step with your steroid taper. If you cut prednisone from 40 mg to 30 mg, reduce your insulin by 15-20%. If you go from 30 mg to 20 mg, cut another 15-20%. Don’t wait for low sugars to happen. Be proactive. Use your glucose log. Track patterns. If your sugars are dropping below 6 mmol/L consistently, it’s time to reduce.Monitoring: More Than Just Fingersticks
Checking your blood sugar four times a day-before meals and at bedtime-is the bare minimum. But if you’re on high-dose steroids, that’s not enough. You need more frequent checks, especially during dose changes. Every 2-4 hours is ideal if you’re in hospital or your sugars are erratic. Continuous glucose monitors (CGMs) are game-changers. They show you not just the number, but the trend. Are you rising? Falling? Stable? The JBDS now recommends at least 48 hours of real-time CGM use during high-dose steroid therapy. Target: spend more than 70% of your day between 3.9 and 10.0 mmol/L. Less than 4% of your time below 3.9 mmol/L. That’s the sweet spot.Special Cases: Insulin Pumps and Outpatients
If you use an insulin pump, you can adjust your basal rate. During peak steroid effect, increase your basal by 25-50% for 24-48 hours. Then dial it back as the steroid tapers. Don’t forget to reset it fully once the steroid is gone. Many pump users miss this step and end up with hypoglycemia. For outpatients on mild steroids (like 5-10 mg prednisone daily), insulin isn’t always needed. If your fasting glucose stays below 11.1 mmol/L, your doctor might try metformin, GLP-1 agonists, or DPP-4 inhibitors. But if your sugars climb above that, insulin is still the safest bet. Never assume oral meds will work just because you’re not in the hospital.
What to Avoid
Don’t use sulfonylureas. Don’t ignore your glucose logs. Don’t wait for symptoms to act. Don’t assume your usual insulin dose will still work. And don’t assume your doctor knows this stuff-many don’t. A 2022 study at Massachusetts General Hospital found 37% of cases of hypoglycemia during steroid tapering happened because insulin wasn’t reduced enough. That’s not bad luck. That’s a system failure.Real-World Tips
- Keep a glucose log: write down your steroid dose, insulin dose, and every reading. Look for patterns.- Talk to your diabetes educator. They know how to match insulin to steroid timing.
- Set phone alarms for glucose checks during the day.
- Tell family or roommates what low blood sugar looks like-shakiness, confusion, sweating-and what to do if you can’t treat it yourself.
- When the steroid ends, schedule a follow-up with your endocrinologist or diabetes team within 3 days. Your insulin needs will keep changing for a week.
What’s Next for Management
Hospitals are starting to use automated systems that link steroid doses in the electronic record to insulin dosing algorithms. If you’re on 40 mg prednisone, the system suggests 0.15 units/kg insulin. If you’re on dexamethasone, it suggests a longer-acting insulin and higher basal. These tools are still new, but they’re cutting errors. In 2023, 68% of U.S. hospitals had formal protocols for this-up from 42% in 2019. Research is moving fast. A 2023 study used machine learning to predict insulin needs based on your weight, steroid dose, and HbA1c. It got it right 85% of the time. Imagine a future where your insulin pump auto-adjusts based on your steroid prescription. That’s not sci-fi-it’s coming.Can steroid-induced hyperglycemia cause permanent diabetes?
Usually not. For most people, blood sugar returns to normal within days or weeks after stopping steroids. But if you already have prediabetes or are at high risk for type 2 diabetes, the stress of high glucose during steroid therapy can push you over the edge. Studies show about 10-15% of people who develop steroid-induced hyperglycemia are later diagnosed with type 2 diabetes within a year. That’s why monitoring after steroids is just as important as during them.
Is it safe to use metformin with steroids?
It can be, but only in mild cases. If your fasting blood sugar stays below 11.1 mmol/L and you’re on low-dose steroids (like 5-10 mg prednisone), metformin may help. But if your sugars are rising fast, or you’re in the hospital, insulin is safer and faster. Metformin doesn’t work well when insulin resistance is severe-which is exactly what steroids cause. Also, avoid metformin if you’re dehydrated or have kidney issues, which can happen with high blood sugar.
How long does steroid-induced high blood sugar last after stopping steroids?
It depends on the steroid. Prednisone’s effect fades in 2-4 days after the last dose. Dexamethasone can linger for 5-7 days because it stays in your system longer. Your blood sugar won’t drop instantly. That’s why you need to keep adjusting insulin for several days after stopping. Don’t assume you’re safe just because you took your last pill.
Can I use GLP-1 agonists like Ozempic during steroid therapy?
They’re not recommended during acute steroid use. GLP-1 agonists slow digestion and reduce appetite, which can make it harder to manage sudden glucose spikes. They’re also slow to act-steroid-induced hyperglycemia moves fast. Insulin is the only tool that responds quickly enough. Once the steroid is fully stopped and your sugars are stable, GLP-1 agonists can be reintroduced safely.
What should I do if I miss a steroid dose?
Don’t panic. But do check your blood sugar. If you missed a steroid dose, your blood sugar may start to drop within hours. If you took your usual insulin dose, you could go low. Hold your bolus insulin for meals and reduce your basal insulin by 20-30% until you resume the steroid. Contact your care team for specific advice. Never double up on steroids to make up for a missed dose-this can cause dangerous spikes.






Write a comment