Stress & Ringworm Risk Calculator
This tool estimates your risk of developing ringworm based on stress levels and hygiene habits. According to research cited in the article, high stress can increase your risk by up to 30%.
Personalized Prevention Tips
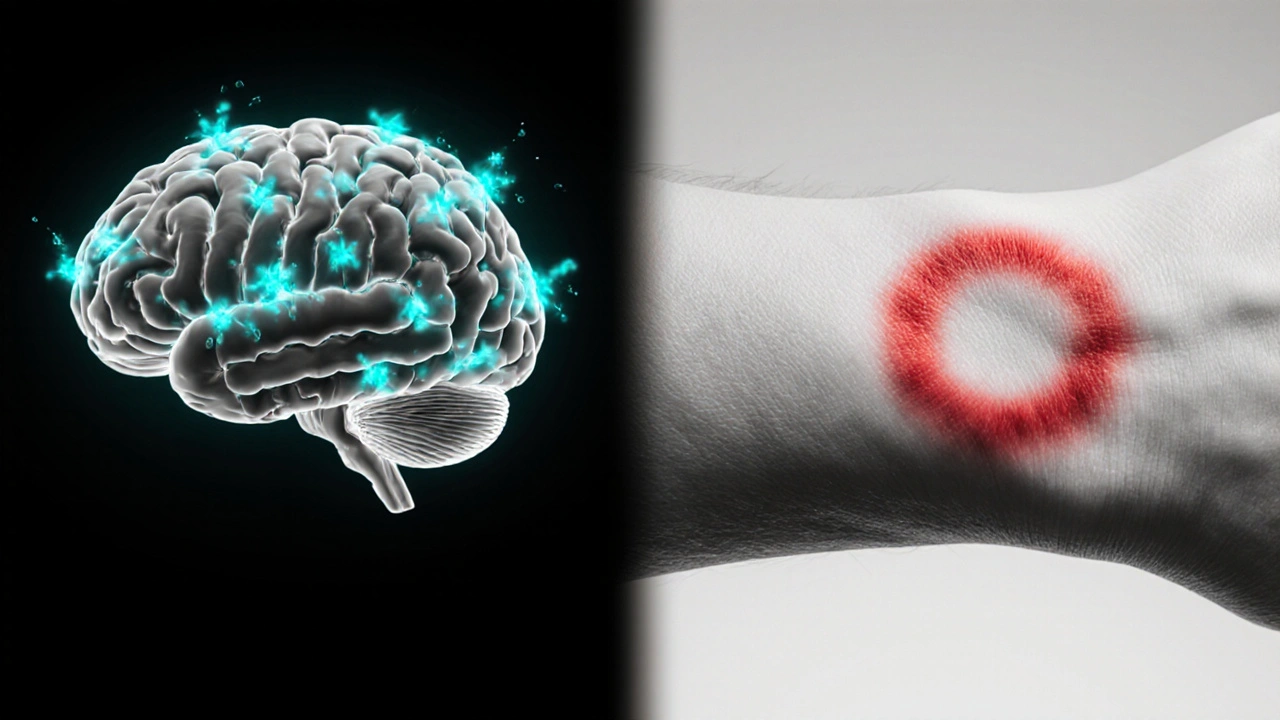
Ever wondered why a stressful week can end with an itchy, circular rash? The culprit might be ringworm, a common fungal infection that loves to strike when your body’s defenses are down.
What is Ringworm?
Ringworm is a contagious skin infection caused by dermatophyte fungi that feed on keratin, the protein that makes up skin, hair, and nails. Despite its name, it isn’t caused by a worm at all; the round, expanding lesions give the illusion of a worm crawling under the skin. The medical term for the condition is dermatophytosis, and it appears in several forms, such as tinea corporis (body), tinea pedis (feet), and tinea capitis (scalp).
How Stress Affects the Body
Stress is the body’s physiological response to perceived threats, releasing hormones like cortisol and adrenaline. While short bursts of stress can boost alertness, chronic stress keeps the endocrine system in overdrive. Elevated cortisol levels suppress the activity of white blood cells, weaken the skin barrier, and disrupt the natural microbial balance on our surface.
The Biological Link Between Stress and Ringworm
Research from the University of Queensland in 2023 showed that individuals with high perceived stress scores were 30% more likely to develop a dermatophyte infection within six months. The chain of events looks roughly like this:
- Cortisol surge: Chronic stress keeps cortisol circulating, which dampens the immune system's ability to spot and destroy invading fungi.
- Skin barrier breakdown: Cortisol reduces collagen synthesis and lowers the production of natural moisturizing factors, making the outer skin layer more porous.
- Microbiome shift: Beneficial bacteria that normally compete with dermatophytes decline, giving the fungus a clearer runway to colonise.
- Behavioural side‑effects: Stressed people are more likely to neglect personal hygiene, wear the same socks for days, or scratch itchy areas, all of which spread spores.
When any of these links are active, the chances of a ringworm outbreak rise dramatically.

Common Scenarios Where Stress Triggers Outbreaks
Imagine a university student pulling all‑night study sessions before exams. The relentless pressure spikes cortisol, the student skips showers, and shares a dormitory bathroom with dozens of peers. Within weeks, a red, scaly patch appears on the foot-classic tinea pedis. Another example: a busy parent caring for newborns may experience sleepless nights and high anxiety. The weakened immune response can let a harmless fungus on a gym mat turn into a noticeable rash on the arm.
These anecdotes are not isolated. A 2022 survey of 1,200 Australian adults found that 42% of respondents who reported “high stress” also reported at least one episode of ringworm in the past year, compared with only 19% among those who described their stress level as low.
Preventing Ringworm When You’re Stressed
Prevention is a mix of physiological care and behavioural habits:
- Manage cortisol: Incorporate brief mindfulness breaks, 10‑minute walks, or breathing exercises into your day. Even a short pause can cut cortisol by 20%.
- Protect the skin barrier: Use a fragrance‑free moisturizer containing ceramides twice daily. Hydrated skin is less permeable to fungal spores.
- Keep hygiene routines non‑negotiable: Shower after sweating, change socks and underwear daily, and dry feet thoroughly-especially between the toes.
- Limit shared surfaces: Wear flip‑flops in public showers, gyms, and pool decks. Disinfect footwear with an antifungal spray.
- Boost immune health: Eat a diet rich in vitaminD, zinc, and probiotics. A study in the Australian Journal of Dermatology linked a 15% reduction in fungal infections to daily kefir consumption.

Treatment Options and When to Seek Help
If a rash does appear, early treatment shortens the infection and stops spread. Over‑the‑counter (OTC) topical antifungals-such as clotrimazole 1% or terbinafine 1%-are effective for most mild cases. Apply twice daily for two weeks, even if the lesion looks healed, to ensure the fungus is fully eradicated.
For extensive or scalp infections, prescription oral agents like itraconazole or fluconazole may be required. These drugs interfere with fungal cell wall synthesis but should only be taken under a doctor’s supervision because of potential liver effects.
Seek medical attention if:
- The rash spreads rapidly or covers a large area.
- You experience severe itching, swelling, or pus.
- OTC creams have been used for more than two weeks with no improvement.
- You have a weakened immune system (e.g., diabetes, HIV, immunosuppressive medication).
Professional care may involve a skin scraping for laboratory confirmation, ensuring the right antifungal is chosen.
Quick Comparison of Ringworm, Athlete’s Foot, and Scalp Fungus
| Feature | Ringworm (Tinea Corporis) | Athlete's Foot (Tinea Pedis) | Scalp Fungus (Tinea Capitis) |
|---|---|---|---|
| Typical Location | Arms, trunk, legs | Between toes, soles | Hair scalp |
| Appearance | Round, red, raised border with clear centre | Redness, peeling, sometimes blistering | Scaly patches, hair loss, black dots |
| Common Triggers | Skin‑to‑skin contact, contaminated clothing | Moist environments, sweating | Close contact in children, shared combs |
| Treatment (OTC) | Clotrimazole, terbinafine cream | Terbinafine spray, miconazole powder | Often requires oral medication |
| Risk of Spread | Medium - can spread by touch | High in communal showers | High in schools/kindergartens |
Frequently Asked Questions
Can stress alone cause ringworm?
Stress doesn’t create the fungus, but it weakens immunity and skin defenses, making it easier for dermatophytes to take hold.
How long does a ringworm infection last with treatment?
Most OTC creams clear the infection in 2-4 weeks. Even after symptoms disappear, continue the full course to prevent relapse.
Is it safe to use natural oils for ringworm?
Tea tree oil and neem have antifungal properties, but evidence is limited. They can be used as adjuncts, but shouldn’t replace proven antifungals for an active infection.
Can children get ringworm from stressed parents?
The fungus spreads through contact, not stress itself. However, stressed parents may unintentionally neglect hygiene, increasing the chance of passing spores to kids.
When should I see a doctor for a suspected ringworm?
If the rash expands rapidly, is painful, produces pus, or doesn’t improve after two weeks of OTC treatment, schedule a medical review.






Write a comment