Calcium Supplement Selector
Your Calcium Needs Assessment
Recommended Calcium Supplement
Important: Consult your healthcare provider before starting any new supplement regimen.
Please fill out all fields to get a recommendation.
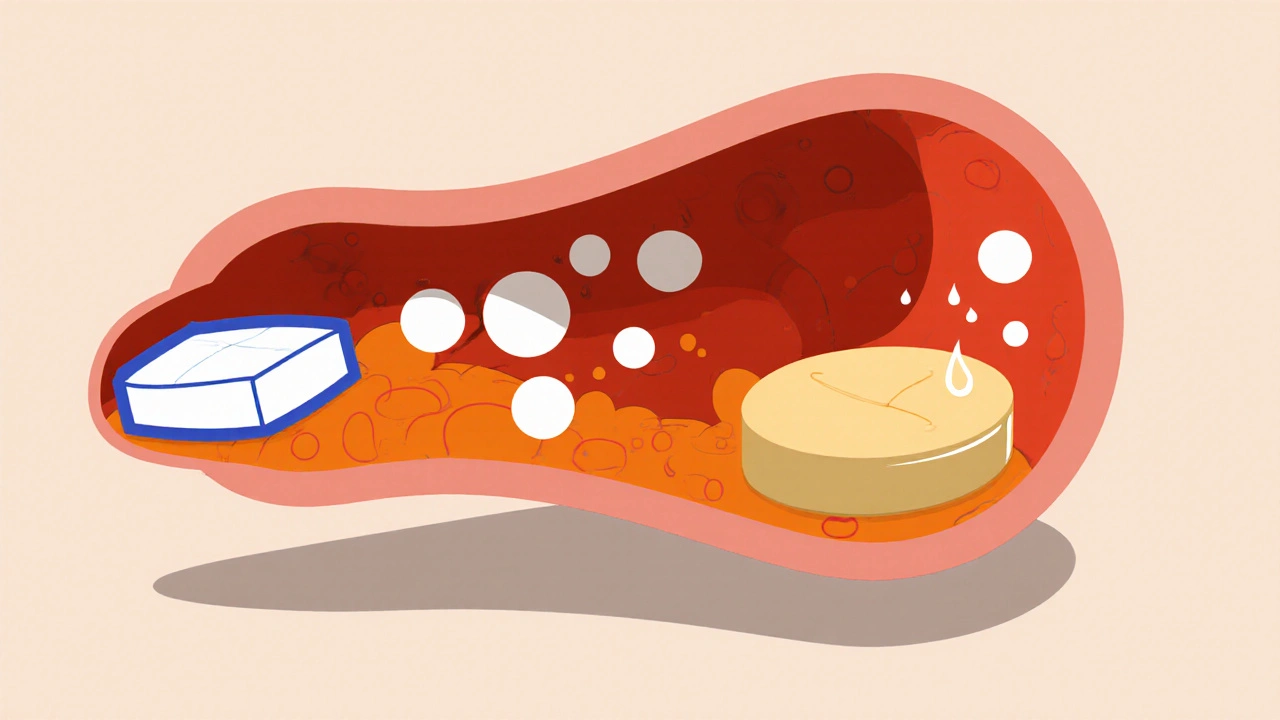
When it comes to boosting calcium intake, Calcium carbonate is the go‑to choice for many, but it’s not the only game in town. From digestive comfort to absorption speed, each calcium source brings its own quirks. This guide breaks down the most common alternatives, weighs them against calcium carbonate, and helps you pick the right supplement for your goals.
Quick Takeaways
- Calcium carbonate offers the highest elemental calcium (40%) at the lowest price.
- Calcium citrate absorbs better on an empty stomach and is gentler on the gut.
- Magnesium carbonate adds a magnesium boost but provides less calcium per dose.
- Vitamin D isn’t a calcium source, but it dramatically improves absorption of all forms.
- Choose based on your digestive health, budget, and specific bone‑support needs.
What is Calcium Carbonate?
Calcium carbonate is a mineral compound naturally found in chalk, limestone, and shells. In supplement form, it delivers the highest amount of elemental calcium-about 40 % of the tablet weight-making it a cost‑effective option for daily dosing. It works best when taken with a meal, as stomach acid helps break it down for absorption.
Typical uses include supporting bone density, aiding muscle function, and preventing calcium deficiency during pregnancy or aging.
Major Alternatives at a Glance
| Supplement | Elemental Calcium % | Absorption Context | Typical Cost (USD per 100 g) | Common Side Effects |
|---|---|---|---|---|
| Calcium citrate | 21 % | Works well on an empty stomach; less dependent on stomach acid | 1.80 | Rare digestive upset |
| Magnesium carbonate | - (focus on magnesium) | Absorbed in the small intestine; often paired with calcium | 2.20 | Laxative effect at high doses |
| Calcium lactate | 13 % | Better than carbonate for low‑acid environments | 2.00 | Mild stomach discomfort |
| Hydroxyapatite | 38 % | Highly bioavailable; mimics bone mineral | 3.50 | Usually well tolerated |
| Vitamin D | 0 % (facilitator) | Enhances calcium absorption across all forms | 0.30 | Rare hypercalcemia if overdosed |
Absorption: How the Body Handles Each Form
Absorption isn’t just about the % of elemental calcium; it’s also about the environment in your gut.
- Calcium carbonate: Needs stomach acid. Best taken with meals containing protein or fat. People on proton‑pump inhibitors may see reduced uptake.
- Calcium citrate: Dissolves in water, so the stomach’s acid level matters less. Ideal for those with low stomach acidity or those who take the supplement on an empty stomach.
- Calcium lactate: Similar to citrate but offers a lower calcium boost per tablet.
- Hydroxyapatite: Structurally identical to bone mineral, so it’s highly bioavailable, especially when combined with vitamin D.
- Magnesium carbonate: Not a calcium source, but when paired with calcium carbonate, it can offset the latter’s potential to cause constipation.
Cost vs. Benefit: Which Offers the Best Value?
Price matters, especially for long‑term users. Below is a quick cost‑benefit snapshot:
- Calcium carbonate: Roughly $0.05 per 500 mg elemental calcium - cheapest per dose.
- Calcium citrate: About $0.09 per 500 mg - higher price, but worth it for people with acid‑reduction medication.
- Hydroxyapatite: $0.12 per 500 mg - premium price, justified by superior bioavailability for bone‑repair patients.
- Magnesium carbonate: Adds $0.02 per 100 mg magnesium - useful as a complementary mineral, not a primary calcium source.
Side Effects and Tolerability
Most calcium supplements are safe at recommended levels (up to 2,000 mg per day for adults). Still, each form has distinct tolerability profiles:
- Calcium carbonate: Can cause constipation or gas, especially in higher doses.
- Calcium citrate: Generally gentler on the gut; less likely to cause constipation.
- Calcium lactate: Mild stomach upset in sensitive individuals.
- Hydroxyapatite: Well tolerated; rare reports of mild nausea.
- Magnesium carbonate: May act as a mild laxative; good for counteracting carbonate‑induced constipation.
When to Choose Each Alternative
Pick the supplement that matches your health profile.
| Scenario | Recommended Form | Why? |
|---|---|---|
| Budget‑conscious adult needing daily calcium | Calcium carbonate | Highest elemental calcium per dollar |
| Older adult on acid‑reducing meds | Calcium citrate | Absorbs without stomach acid |
| People with a history of kidney stones | Hydroxyapatite + Vitamin D | Lower risk of oxalate buildup; mimics bone mineral |
| Those needing both calcium and magnesium | Combined calcium carbonate + magnesium carbonate | Balances calcium load while preventing constipation |
| Individuals with sensitive stomachs | Calcium citrate or calcium lactate | Gentler dissolution, fewer GI issues |
How to Build an Effective Calcium Regimen
- Assess your daily calcium need (usually 1,000 mg for adults, 1,200 mg for post‑menopausal women).
- Calculate dietary intake from foods (dairy, leafy greens, fortified products).
- Pick a supplement that fills the gap without exceeding the total recommended intake.
- Pair with Vitamin D (800‑1,000 IU daily) to boost absorption.
- Take calcium carbonate with a main meal; take calcium citrate anytime you like.
- Monitor for side effects-constipation, gas, or unusual fatigue-and adjust the form or dosage.
Frequently Asked Questions
Is calcium carbonate better than calcium citrate for bone health?
Both provide the same amount of elemental calcium when taken in equivalent doses, but calcium citrate is absorbed more reliably in people with low stomach acid. If you’re healthy and can afford the cheaper option, calcium carbonate works fine; otherwise, citrate is the safer bet.
Can I take calcium carbonate and magnesium carbonate together?
Yes, many multi‑mineral formulas combine them. Magnesium can help offset the constipation some people experience with calcium carbonate, and the two minerals work synergistically for muscle and nerve function.
Do I need vitamin D with calcium supplements?
Vitamin D is essential for calcium absorption. Even a modest daily dose (800‑1,000 IU) can raise uptake by 30‑40 %. Without it, the body discards much of the calcium you consume.
Is hydroxyapatite safe for long‑term use?
Hydroxyapatite mimics the mineral composition of bone, making it very bioavailable and generally safe. It’s often recommended for patients with osteoporosis or after fracture surgery.
Can calcium supplements cause kidney stones?
Excess calcium, especially from calcium oxalate‑rich foods, can increase stone risk. Using calcium carbonate with adequate fluid intake and balancing with magnesium reduces this danger. Always stay within the recommended daily limit.
Bottom Line
There’s no one‑size‑fits‑all answer. Calcium carbonate wins on price and sheer calcium content, but it demands stomach acid and can be harsh on the gut. Calcium citrate shines for people on acid‑blocking meds or with a sensitive stomach. Magnesium carbonate adds a helpful secondary mineral, while hydroxyapatite offers premium bone‑repair benefits at a higher cost. Pair any calcium source with vitamin D, watch your total intake, and choose the form that aligns with your health profile.







Write a comment