Antiplatelet Drug Decision Tool
Find the Right Antiplatelet Medication
When your doctor prescribes a blood thinner, you probably wonder how it stacks up against the other options. Dipyridamole is a platelet‑aggregation inhibitor that’s often tucked into the ‘anticoagulant’ aisle, but it isn’t the only player. This guide walks through what makes Dipyridamole unique, compares it with the most common alternatives, and helps you figure out which drug fits your health goals.
What is Dipyridamole?
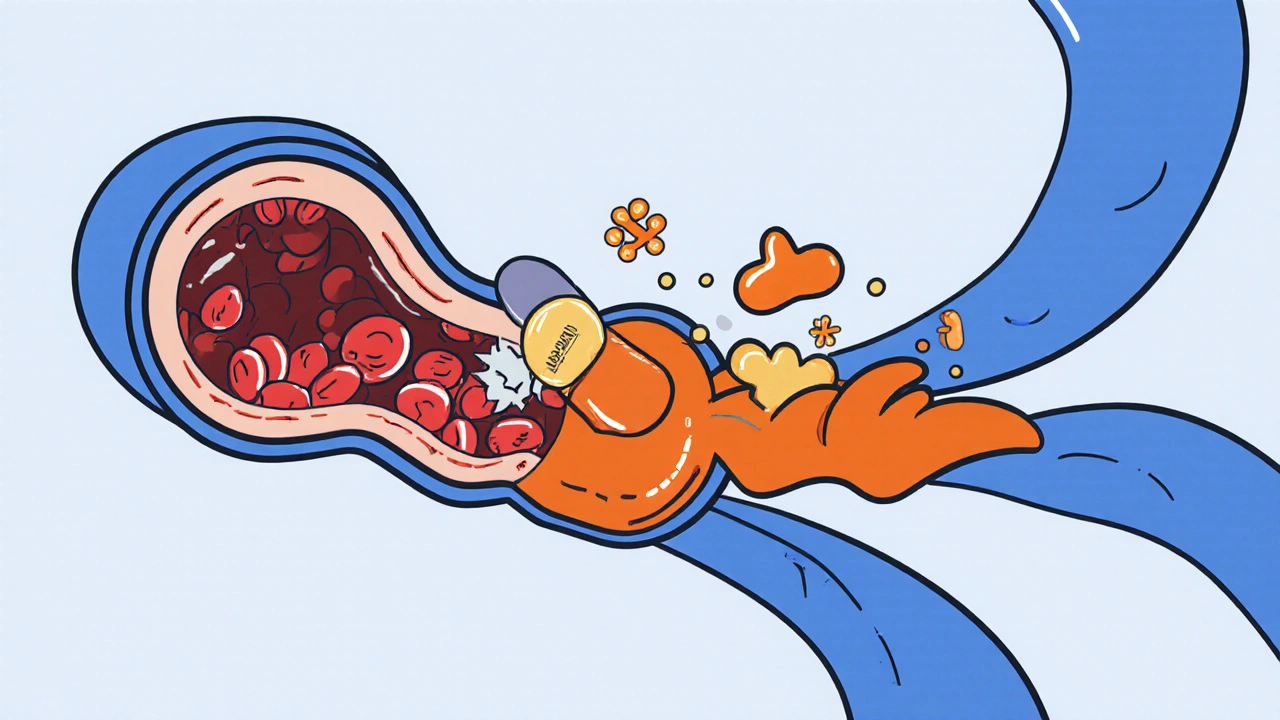
Dipyridamole is a synthetic medication first approved in the 1960s. It belongs to the class of phosphodiesterase inhibitors and works by raising cyclic AMP levels in platelets, which reduces their ability to clump together. Unlike classic anticoagulants that target clotting factors, Dipyridamole acts upstream, keeping platelets from forming the initial plug.
How Dipyridamole Works
The drug blocks the uptake of adenosine into red blood cells and endothelial cells. More adenosine stays in the bloodstream, causing vasodilation and inhibiting platelet activation. In practical terms, the higher adenosine level creates a smoother blood flow, especially in the brain’s small vessels, which is why Dipyridamole is often paired with aspirin for stroke prevention.
Primary Clinical Uses
- Secondary prevention of ischemic stroke when combined with low‑dose aspirin.
- Prevention of restenosis after coronary angioplasty (off‑label in many countries).
- Adjunct therapy in certain cases of peripheral artery disease.
Pros and Cons of Dipyridamole
Pros
- Synergistic effect with aspirin improves protection against non‑cardioembolic strokes.
- Relatively low cost compared with newer antiplatelet agents.
- Well‑studied safety profile in elderly patients.
Cons
- Can cause headaches and flushing due to vasodilation.
- Not as potent as newer P2Y12 inhibitors for preventing coronary events.
- Requires multiple daily doses, which may affect adherence.
Key Alternatives to Dipyridamole
Below are the most widely used antiplatelet or anticoagulant drugs that clinicians consider alongside Dipyridamole.
Aspirin (acetylsalicylic acid) irreversibly blocks COX‑1, lowering thromboxane A2 production. It’s the backbone of most cardiovascular prevention regimens.
Clopidogrel is a pro‑drug that inhibits the P2Y12 ADP receptor on platelets. It’s frequently used in patients who can’t tolerate aspirin.
Ticagrelor is a reversible P2Y12 inhibitor with a faster onset and more consistent platelet inhibition than Clopidogrel.
Warfarin acts on the vitamin K cycle, reducing synthesis of clotting factors II, VII, IX, and X. It’s an anticoagulant, not a platelet inhibitor, but it’s sometimes combined with antiplatelets for high‑risk patients.
Heparin (including low‑molecular‑weight variants) enhances antithrombin III activity and blocks thrombin formation. It’s mainly used in acute care settings.
Other drugs that occasionally appear in the same conversation include Cilostazol, a phosphodiesterase‑3 inhibitor used for intermittent claudication, and Prasugrel, a more potent P2Y12 blocker reserved for certain percutaneous coronary intervention (PCI) patients.
Side‑Effect Comparison Table
| Drug | Common Side Effects | Serious Risks | Typical Dose Frequency |
|---|---|---|---|
| Dipyridamole | Headache, flushing, nausea | Bleeding (mild), hypotension when combined with nitrate | Twice daily |
| Aspirin | Gastro‑intestinal upset, heartburn | Gastro‑intestinal bleeding, hemorrhagic stroke | Once daily |
| Clopidogrel | Bruising, diarrhea | Severe bleeding, rare thrombotic thrombocytopenic purpura | Once daily |
| Ticagrelor | Dyspnea, cough | Major bleeding, hyperuricemia | Twice daily |
| Warfarin | Dietary restrictions, minor bruising | Life‑threatening bleeding, skin necrosis | Once daily (adjusted to INR) |
How to Choose the Right Antiplatelet
Picking a blood‑thinner isn’t a one‑size‑fits‑all decision. Here’s a quick decision flow you can run through with your doctor.
- Is stroke prevention the main goal? If yes, Dipyridamole + Aspirin has strong evidence for non‑cardioembolic strokes.
- Do you have a high bleeding risk? Aspirin alone or low‑dose Clopidogrel may be safer than combining agents.
- Are you undergoing coronary stenting? P2Y12 inhibitors (Clopidogrel, Ticagrelor, Prasugrel) are preferred over Dipyridamole.
- Do you need rapid platelet inhibition? Ticagrelor’s quick on‑set beats Dipyridamole’s slower action.
- Is cost a major factor? Dipyridamole and Aspirin are generally the cheapest options.
Always weigh the benefit‑risk balance with your clinician. The best drug for one patient could be the worst for another because of genetics, comorbidities, or lifestyle.
Quick Takeaways
- Dipyridamole boosts adenosine, causing vasodilation and platelet inhibition.
- It shines in stroke prevention when paired with aspirin.
- Side‑effects like headache are common; serious bleeding is rare but possible.
- Alternatives such as Clopidogrel, Ticagrelor, and Warfarin target different pathways and suit other cardiovascular scenarios.
- Discuss your personal risk profile with a healthcare professional before switching.
Frequently Asked Questions
Can I take Dipyridamole without aspirin?
Dipyridamole can be used alone for certain indications, but its stroke‑prevention benefit is strongest when combined with low‑dose aspirin. Your doctor will decide based on your risk factors.
How quickly does Dipyridamole start working?
Peak platelet inhibition occurs about 1-2 hours after ingestion, but full therapeutic effect may take several days of consistent dosing.
Is Dipyridamole safe during pregnancy?
Animal studies raise concerns about fetal toxicity, and human data are limited. It is generally avoided unless the benefit clearly outweighs the risk.
What should I do if I experience severe headache on Dipyridamole?
Contact your healthcare provider. They may lower the dose, add a short‑acting analgesic, or switch to an alternative antiplatelet.
Can Dipyridamole interact with other medications?
Yes. Nitrates can cause excessive blood‑pressure drop, and certain antihypertensives may amplify the vasodilatory effect. Always list all current meds to your doctor.







Write a comment